Case report - Volume 3 - Issue 3
Chronic cough: An unlikely complication of pharyngolaryngeal herpes zoster
Stavros N. Nikitopoulos1, Anastasia A. Oikonomou1, Methodios T. Stavridopoulos1, Georgia K. Tsiouma2
1Resident in Otorhinolaryngology, ENT department of General Hospital of Volos “Achillopouleio”, Greece.
2Attending in Otorhinolaryngology, ENT department of General Hospital of Volos “Achillopouleio”, Greece.
Received Date : April 03, 2023
Accepted Date : May 05, 2023
Published Date: May 12, 2023
Copyright:© Georgia K. Tsiouma 2023
*Corresponding Author : Georgia K. Tsiouma, Attending in Otorhinolaryngology, ENT department of General Hospital of Volos “Achillopouleio”, Greece.
Email: gtsiouma@yahoo.gr
DOI: Doi.org/10.55920/2771-019X/1437
Abstract
Herpes zoster, occurs by the reactivation of the varicella-zoster virus (VZV), the same virus that causes varicella, also known as chickenpox. Once varicella resolves, the virus remains inactive in the dorsal root and cranial ganglia. Pharyngolaryngeal zoster constitutes a rare clinical manifestation of this medical entity. The unilateral varicelliform eruptions of the oral cavity, pharynx and larynx are the typical clinical presentation. Postherpetic complications, with the exception of neuralgia, are rarely mentioned in the literature. We present the case of an 80-year-old male with pharyngolaryngeal zoster and normal function of the glossopharyngeal and vagal nerve, who suffered from persistent postherpetic dry cough and neuralgia, which subsided with pregabalin.
Keywords: Herpes zoster; Pharyngolaryngeal zoster; postherpetic neuralgia; Postherpetic cough.
Introduction
After the primary infection by varicella zoster virus (VZV), known as chickenpox, the virus remains latent at the dorsal roots or cranial nerve ganglia. The reactivation of the virus can result to herpes zoster and any autonomic ganglion or cranial nerve can be involved. It is rare for herpes zoster to be located in the pharynx or larynx, especially without vagal and/or glossopharyngeal palsy being present. Although postherpetic neuralgia (PHN) is a common complication of herpes zoster, chronic cough after the infection is extremely rare.
Case report
An 80-year-old male presented to the ENT department with a five-day history of a sore throat, hoarseness of voice and dysphagia. He had been previously diagnosed with acute bacterial pharyngitis by a private practice physician and received cefprozil as treatment, without any improvement of the symptoms. Throughout the clinical examination no skin lesion was noted on the facial or auricular area. The patient was afebrile and fully alert and oriented. The examination of the oral cavity showed vesicles on the mucosa of the soft and hard palate, the uvula and the left tonsil, which are innervated by the tonsilar and lingual branches of the glossopharyngeal nerve (Figure 1). In addition, the presence of vesicles of the mucosa of the posterolateral wall of the pharynx suggest that the pharyngeal plexus was affected. Rigid fiberoptic laryngoscopy revealed a generalized erythema of the left supraglottic area and left lateral and posterior wall of the pharynx along with multiple lesions covered by white exudates (Figures 2). The lesions were located unilaterally, on the left side, affecting the laryngeal aspect of the epiglottis, the aryepiglottic fold, the pyriform sinus and the posterolateral wall of the hypopharynx, which are all innervated by the internal branch of the superior laryngeal nerve. The mobility of the vocal cords and the palate were normal and the gag reflex was not affected. The patient had a known history of hypothyroidism, hypertension, dyslipidemia, benign prostatic hyperplasia and type 2 diabetes mellitus. The patient’s VZV antibodies were elevated, specifically VZV IgG= >4000 IU/ml (negative <135 IU/mL) and VZV IgM= 1.60 (negative <0.9 index). The patient was treated with acyclovir and the lesions subsided completely on the fifth day of hospitalization. The patient complained subsequently about persistent dry cough, caused by no specific triggering factors and persistent sharp pain located on the left tonsillar and auricular area. We excluded asthma, chronic rhinosinusitis, allergies, gastroesophageal reflux disease (GERD), SARS-COV-19 infection and post COVID syndromes as a potential cause of the cough. Given the acute onset of the symptoms they were considered to be complications of the herpetic infection. After presenting to the patient the treatment options, according to the literature, it was collectively decided to proceed with the pregabalin treatment plan starting with 25mg per os daily and adjusting the dose in the next monthly follow-up visits reaching up to 75mg daily. The cough and pain subsided after three months of treatment and dose tapering instructions were provided over a course of three additional months. The patient remained asymptomatic six months after completion of the treatment plan.
Discussion
VZV belongs to the subfamily of alpha herpes viruses. It can manifest as a primoherpetic infection, more commonly known as chickenpox, or as herpes zoster, which occurs after the reactivation of the virus from the dorsal roots or cranial nerve ganglia [1]. The reactivation takes place usually in people with

Figure 1: Unilateral herpetic vesicles of the palate and uvula.
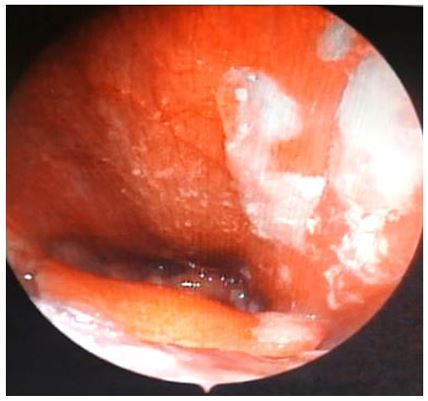
Figure 2: Unilateral herpetic vesicles of the pharynx and epiglottis.
an impaired cell-mediated immunity, namely patients suffering from malignancies, receiving treatment with immunosuppressant drugs, patients with history of organ transplantation or HIV positive patients [2]. The incidence of herpes zoster is higher in older patients and can be triggered by psychological or physical stress like infection or trauma [1,2]. The reactivation of VZV typically manifests as varicelliform cutaneous lesions corresponding to the dermatomes innervated by one or more spinal or cranial nerves. The most common clinical manifestation of VZV that concerns otorhinolaryngologists is Ramsay Hunt syndrome mainly involving cranial nerve VII [3]. However, our study highlights a rare case of pharyngolaryngeal zoster which affected the glossopharyngeal and vagal nerve without the presence of skin lesions, vocal cord palsy or Ramsay Hunt syndrome.
Although the diagnosis of pharyngolaryngeal zoster is based on the clinical findings, definitive diagnosis requires serological or immunological evidence. Acute VZV infection may be diagnosed by PCR analysis of the vesicle content (method of choice), through viral isolation and growth in cell culture or via direct immunofluorescence test using monoclonal antibody specific for VZV [4]. In our institution these methods were unavailable. Thus, we conducted a serum test specific for VZV IgM and IgG antibodies, even though it is not considered reliable for the early diagnosis of the disease [5]. Based on the characteristic clinical findings and the elevated titers of IgM and IgG specific antibodies, diagnosis of VZV was confirmed. A review of the literature performed by Nisa et al. listed the complications occurring in patients with pharyngolaryngeal involvement of herpes zoster infection [6]. Out of the nonfull recovery outcomes, the most common complication was laryngeal paresis. Moreover, pharyngeal paresis, pharyngeal hypesthesia, sudden neurosensory hearing loss, facial paresis, hypogeusia, vestibular deficits, and PHN were included while meningoencephalitis occurred in one patient. Our patient presented PHN, manifesting as unilateral tonsillar pain and otalgia, as well as chronic cough.
Chronic cough is an extremely rare complication of VZV. A search of the literature revealed only two cases described in an article by Ling et al [7]. They suggested that as a consequence of VZV infection, the vagal nerve and its branches are prone to abnormal rewiring within the cough reflex arc or they may be rendered hyper reactive towards normal stimuli. Morrison et al. list viral infection as one of the causes of the “irritable larynx syndrome” which they initially described [8]. They proposed that damage to the nerves supplying the upper respiratory system may lead to altering of the connections of the neural network or to changes of the phenotype of the neuronal cells in the brainstem. The latter occurs through activation of plasticity related genes such as c-fos or c-jun. This leaves the neural cell in a state of hyper-excitability causing symptoms such as cough, laryngospasm, dysphonia or globus. A considerable amount of research has been conducted on neuromodulatory agent drugs and their potential use in patients with chronic refractory cough (CRC). The CHEST Expert Cough Panel suggests the trial treatment with gabapentin in adults with unexplained chronic cough [9]. In addition, among the recommendations of the European Respiratory Society guidelines, a trial treatment of low dose slow-release morphine and a trial therapy of pregabalin or gabapentin in adults with CRC are included [10]
Conclusion
Pharyngolaryngeal herpes zoster is a rare manifestation of VZV, but it can present with common clinical symptoms such as sore throat and hoarse voice. Patients that present with unilateral lesions of the oral cavity and oropharynx should be referred to an ENT specialist, for evaluation of the function of the relative cranial nerves. The complications of pharyngolaryngeal herpes zoster, mainly nerve palsies and chronic pain, affect the patient’s quality of life and render early diagnosis crucial, even though they are rarely life-threatening. Pregabalin should be considered as a treatment option for future encounters with similar cases.
Acknowledgements: All authors participated in the research design and writing of the paper.
Funding: The authors declare no funding.
Disclosure: The authors declare no conflicts of interest.
Statement of consent: The authors have received consent from the patient to publish the attached images and case details.
References
- Chen PS, Lin YY, Huang BR. Pharyngolaryngeal zoster: a case report. Archives of 1. Chen PS, Lin YY, Huang BR. Pharyngolaryngeal zoster: a case report. Archives of otolaryngology--head & neck surgery. 2012; 138(6): 592-5.
- Johnson RW, Dworkin RH. Treatment of herpes zoster and postherpetic neuralgia. Bmj. 2003; 326(7392): 748-50.
- Sweeney CJ, Gilden DH. Ramsay Hunt syndrome. Journal of neurology, neurosurgery, and psychiatry. 2001; 71(2): 149-54.
- Sauerbrei A. Diagnosis, antiviral therapy, and prophylaxis of varicella-zoster virus infections. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 2016;35(5):723-34.
- Sauerbrei A, Eichhorn U, Schacke M, Wutzler P. Laboratory diagnosis of herpes zoster. Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology. 1999; 14(1): 31-6.
- Nisa L, Landis BN, Giger R, Leuchter I. Pharyngolaryngeal involvement by varicella-zoster virus. Journal of voice : official journal of the Voice Foundation. 2013; 27(5): 636-41.
- Ling B, Novakovic D, Sulica L. Cough after laryngeal herpes zoster: a new aspect of post-herpetic sensory disturbance. The Journal of laryngology and otology. 2014; 128(2): 209-11.
- Morrison M, Rammage L, Emami AJ. The irritable larynx syndrome. Journal of voice : official journal of the Voice Foundation. 1999; 13(3): 447-55.
- Gibson P, Wang G, McGarvey L, Vertigan AE, Altman KW, Birring SS, et al. Treatment of Unexplained Chronic Cough: CHEST Guideline and Expert Panel Report. Chest. 2016; 149(1): 27-44.
- Morice AH, Millqvist E, Bieksiene K, Birring SS, Dicpinigaitis P, Domingo Ribas C, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. The European respiratory journal. 2020; 55(1).

