Clinical Image - Volume 3 - Issue 3
Life Story of a Mycotic Pulmonary Artery Aneurysm
Borna Amir-Kabirian1*; Scott Morehead2
1Resident, Department of Internal Medicine, Charleston Area Medical Center/West Virginia University-Charleston, USA.
2Professor of Medicine, Department of Critical Care and Pulmonology, West Virginia University- Charleston Division and Charleston Area Medical Center, USA.
Received Date : April 04, 2023
Accepted Date : May 10, 2023
Published Date: May 17, 2023
Copyright:© Borna Amir-Kabirian 2023
*Corresponding Author : Borna Amir-Kabirian, Resident, Department of Internal Medicine, Charleston Area Medical Center/West Virginia University-Charleston, USA.
Email: Borna.Amir-Kabirian@camc.org
DOI: Doi.org/10.55920/2771-019X/1440
Clinical Image
A 29-year-old woman with a history of IV heroin use presented to the emergency department with hemoptysis. Prior to admission, she had a large tricuspid valve vegetation with embolism to the left lower lobe (Figure 1A). At that time, she had an embolic event to the right lower lobe pulmonary artery (Figure 1B) and underwent tricuspid valvuloplasty. Intraoperative microbiology confirmed Candida albicans. On this admission, she was intubated, and CT-angiography suggested mycotic pseudoaneurysm (Figure 1C) of the right lower lobe pulmonary artery, resulting in endovascular coiling by interventional radiology (Figure 1D). However, she had recurrent, massive hemoptysis. Bronchoscopy isolated the hemorrhage to the right mainstem bronchus, requiring emergent bronchial blocker placement. She subsequently underwent angiography with successful right bronchial artery embolization. She was extubated, but again had recurrent hemoptysis. Repeat bronchoscopy revealed extensive hemorrhage and bronchial blocker was again placed in the right bronchus. She ultimately underwent lobectomy. Mycotic aneurysms are irreversible vessel wall dilations caused by an infectious etiology. True aneurysms include all three layers of the vessel wall. By contrast, pseudoaneurysms typically involve two layers and lack adventitial involvement [1]. They are thought to arise from intimal involvement from septic emboli or bacteremia [2,3]. Mortality exceeds 50%, and treatment is individualized and includes observation, embolization, and/or surgery. In the presence of life-threatening hemoptysis, surgical resection, including pneumectomy, should be considered [3].
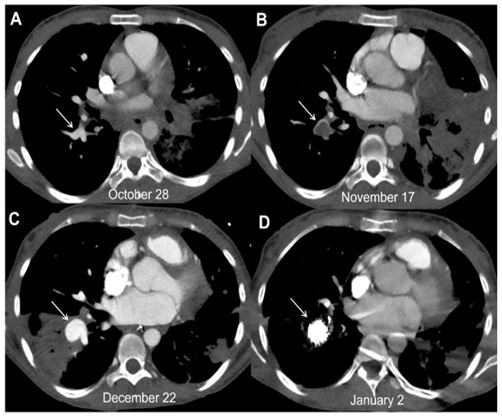
Figure 1: Axial contrast-enhanced computed tompgraphy scans in soft tissue windows. Right lower lobe pulmonary artery (arrows): before embolism (A); after embolism (B); aneurysmal dilation (C); after multiple coils placed (D).
References
- Sharma PK, Garisa SS, Kuma ran SV, Varma S. Mycotic (Infected) Pseudoaneurysm, a Diagnostic Challenge - Case Series. J Clin Imaging Sci. 2020; 10:86.
- Mody GN, Lau CL, Bhalla S, et al. Mycotic pulmonary artery pseudoaneurysm. J Thorac Imaging. 2005; 20(4): 310-312.
- Torpey E, Spears J, Al-Saiegh Y, Roeser M. A Conservative Approach to a Large Mycotic Pulmonary Pseudoaneurysm. Case Rep Pulmonol. 2021; 2021: 6456216.

