Case report - Volume 3 - Issue 3
The AMSAN Variant of GBS, A Rare Complication of COVID-19: A Case Report and Literature Review
Rakhshinda Jabeen1; Misbah Maktoob2*; Imran Khan2; Ahsan Mobin3
1Associate Professor, Dow University of Health Sciences, Pakistan.
2Resident Medical Officer, Dow University of Health Sciences, Pakistan.
3Assistant Professor, Dow University of Health Sciences, Pakistan.
Received Date : April 08, 2023
Accepted Date : May 12, 2023
Published Date: May 19, 2023
Copyright:© Misbah Maktoob 2023
*Corresponding Author : Misbah Maktoob, Resident Medical Officer, Dow University of Health Sciences, Pakistan.
Email: misbah.butla@gmail.com
DOI: Doi.org/10.55920/2771-019X/1442
Abstract
We here report an unusual presentation of the SARS CoV-2, in which the patient did not have any respiratory symptoms rather the presenting complaint was bilateral lower limb weakness, which was later found to be the AMSAN variant of GBS, a rare complication of COVID-19.
Introduction
SARS-CoV-2, a beta coronavirus, produces fever, cough, and difficulty breathing as the presenting symptoms were very much similar to SARS and MERS [1]. Mao et al. study was the first who reported Neurological manifestations of COVID-19. About one-third of COVID-19 sufferers manifest neurological complications, including nausea, vomiting, headache, dizziness, anosmia, ageusia, altered level of consciousness, and acute cerebrovascular disease. Anosmia and ageusia are the commonest neurological symptoms. Neurological symptoms result from the direct viral invasion of the neurological system [2].
Case report
Our patient is a fifteen-year-old male, farmer, who was up and about 3 days before the illness. The disease started with a feverish feeling and later on the development of sudden weakness of the bilateral lower limb which the patient
notices while working in the field. As he presents to us in ED he was unable to stand on his feet or with support and can’t move his lower limbs. On further questioning, he denies urinary or bowel incontinence or retention, shortness of breath, any alteration of mentation, backache, or any symptom related to gastrointestinal and cardiovascular symptoms. There was no significant past medical history, no history of Tuberculosis or Tuberculosis in nearby contact. On examination, power is 4/5 in bilateral upper limbs of all joints and 2/5 in bilateral lower limbs as per the Medical Research Council (MRC) grading of muscle power with mute planters and absent deep tendon reflexes. Apart from the neurological examination, there was an unremarkable general physical and systemic examination. His initial lab parameters show a TLC of 10.8 with lymphopenia.
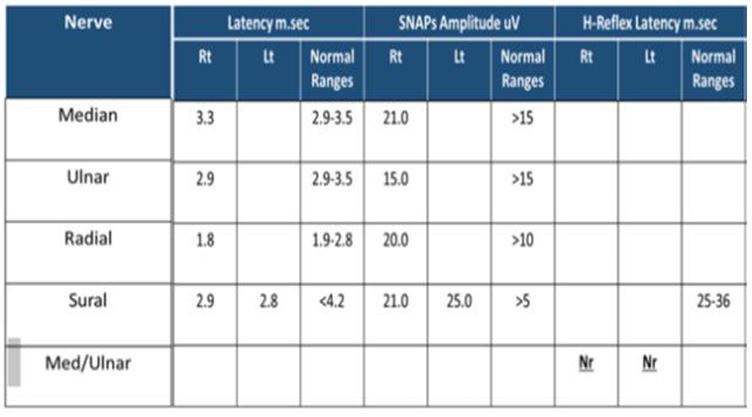
Talking about the inflammatory markers, his initial C-Reactive Protein (CRP) was 2.3 mg/dL, Serum Ferritin levels were 77, while serum lactate dehydrogenase levels were a bit elevated i.e 435 IU/L (Table.1). Despite not having any chest symptoms and an unremarkable CXR (Figure.1), we went for a PCR test for SARS-CoV which came out to be positive. His CSF D/R shows glucose 62gm/dL of with a normal protein and cellular content (Table.2). However, Nerve conduction studies findings consistent with acute sensory motor axonal polyneuropathy with non-recordable H-reflexes and F-latencies. MRI spine showed no pathology. Anti-nuclear antibodies were performed which came out to be negative as well. Regarding concern for his glycemic control no derangement in Fasting Blood Sugars and HbA1C of 5.6%. Based on the aforementioned workup, the patient is being diagnosed as having Guillain Barre Syndrome secondary to COVID. Sessions of plasmapheresis were scheduled, and there was a remarkable improvement in symptoms as well as lab parameters. He was able to move his lower limbs against gravity after the second session of plasmapheresis and was able to stand with support after the fourth session. Serum lactate dehydrogenase level improved to 201 IU/L, and serum Ferritin to 16. The patient was able to walk without support
soon after his fifth session of plasmapheresis. Injectable anti-viral ( REMDESEVIR) and subcutaneous anti-coagulation (enoxaparin) were added to the treatment.
Table 1: Blood investigations during the admission.
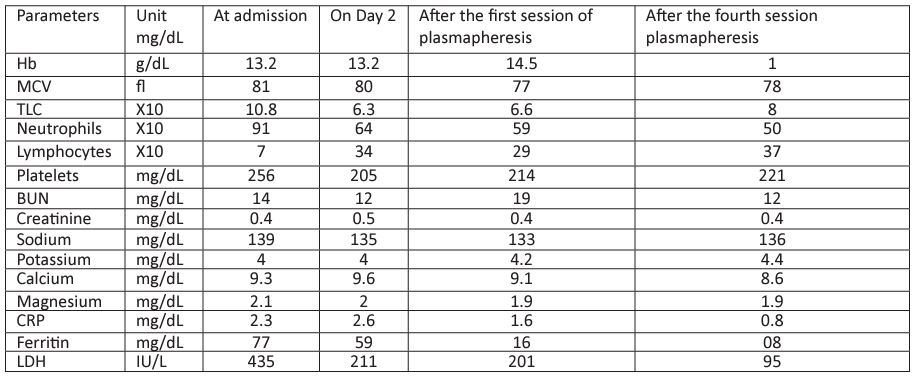
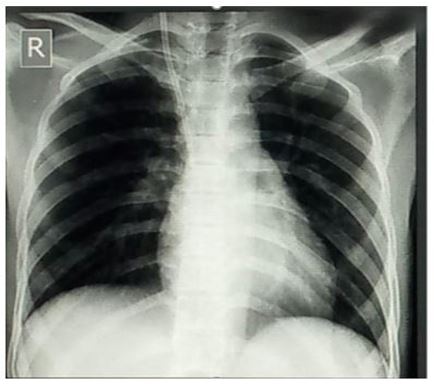
Figure 1: Chest X-ray PA view.
Table 2: CSF detailed report on the second day of admission.
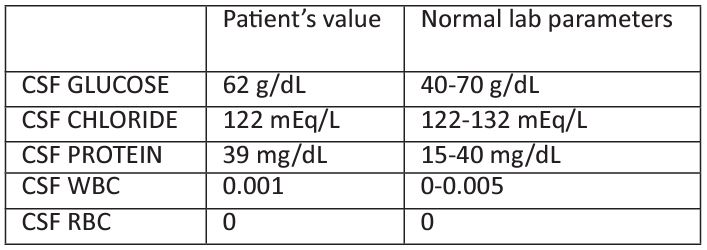
Table 3: Nerve Conduction Studies.
Discussion
GBS is yet a unique and rare neurological manifestation of SARS-CoV-2, and still, 42 cases are being reported in the literature [3]. Our case of a young boy, presented with sudden onset symmetrical lower limb weakness followed by an episode of fever is a unique presentation of COVID-19 provoking the GBS-AMSAN variant. GBS, an acute monophasic polyneuropathy affects patients from around the world indifferent of race, age, and gender. This acute paralyzing illness most of the time proceeded by an infectious disease [4]. Apart from COVID-19, various other microbes are found to be a culprit in provoking this life-threatening illness which includes Campylobacter jejuni, Haemophilus influenza, Ebstein Barr virus, Cytomegalovirus, Zika virus, Influenza A virus, Mycoplasma and SARS-CoV-2 akin SARS and MERS [5]. Several different mechanisms are being proposed as the sole cause of GBS formation [6]. Four subtypes of acute peripheral neuropathy are included in GBS. As time propels, we get to know a few mechanisms to understand the pathophysiology behind the formation of GBS. There exists a marked resemblance between acute inflammatory demyelinating polyneuropathy (AIDP) and experimental autoimmune neuritis based on histology. The main culprit behind all the mayhem is the T-cell, which became active against peptides from myelin proteins P0, P2, and PMP22. Although this T-cell mediation is dubious there is substantiation of autoantibodies and compliment. The axonal subtypes of GBS, AMAN, and AMSAN, are antecedent by the formation of antibodies to the axolemmal gangliosides that direct macrophage to attack the axons at the nodes of Ranvier [7].
The pathogenesis of the formation of GBS in patients suffering from COVID-19 is still debatable. SARS-CoV-2 triggers inflammatory cells which leads to the cascade of the production of several different inflammatory cytokines and inflammatory processes [8]. ACE-2-R is the common site to be attacked by both SARS and SARS-CoV-2 [1, 8]. Various organs (lung, kidney, skeletal muscle, nervous system, and liver) inside human beings have these receptors over their cell membrane [2]. The notorious COVID-19 attaches to the cell membrane by its viral spike (S) protein, which later binds to the ACE-2 enzyme and sialic acid residue containing ganglioside, including GaINAC residues of GM1 [9]. Molecular mimicry is the proposed mechanism of autoimmunity for the formation of GBS [10]. COVID-19-causing GBS may sometimes deficit with the autoantibody formation, in such cases a parainfectious phenomenon is proposed, arbitrated by a generalized, hyper-inflammatory response. Talking about an axonal variant of GBS, AMSAN, which is in our case an unusual presentation [11]. However, a similar pattern of progression of the disease, i.e, respiratory symptoms of COVID-19 later progresses to GBS, supports COVID-19 as being the sole reason behind causing this acute paralyzing illness. So, in the pandemic of COVID-19, it’s the keen responsibility of every physician to have this dreadful neurological manifestation somewhere in the back of his mind, while managing patients suffering from the virus and arranging at least one follow-up visit soon after discharge. To prevent dreadful complications of GBS like respiratory paralysis, pulmonary embolism, cardiac arrest, and sepsis, an aggressive management plan including IVIG should be planned earlier. As far as the causative mechanisms whether due to molecular mimicry or direct neurological invasion has yet to be established and need more clinical review and literature studies [11].
Conclusion
With the ongoing pandemic caused by SARS-CoV-2, we came across a different and interesting presentation of the virus. Symptomatology is not bound only to the chest rather it’s a multisystem presentation. Being a physician, everyone should beyond the basic scope as medicine is evolving day by day. GBS caused by COVID-19 is yet a unique presentation and knowledge of it, is ace in patient management.
Competing interest
The authors declared no competıng interest.
Consent from patient
Written informed consent for patient information and images to be published was provided by the patient.
References
- Sedaghat Z, Karimi N. Guillain Barre syndrome associated with COVID-19 infection: A case report. J Clin Neurosci. 2020; 76: 233-235.
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77(6): 683-690.
- Uncini A, Vallat JM, Jacobs BC. Guillain-Barré syndrome in SARS-CoV-2 infection: an instant systematic review of the first six months of pandemic. J Neurol Neurosurg Psychiatry. 2020; 91(10): 1105-1110.
- Wijdicks EF, Klein CJ. Guillain-Barré Syndrome. Mayo Clin Proc. 2017; 92(3): 467-479.
- Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016; 388(10045): 717-27.
- Jasti AK, Selmi C, Sarmiento-Monroy JC, Vega DA, Anaya JM, Gershwin ME. Guillain-Barré syndrome: causes, immunopathogenic mechanisms, and treatment. Expert Rev Clin Immunol. 2016; 12(11): 1175-1189.
- Hughes RA, Cornblath DR. Guillain-Barré syndrome. Lancet. 2005; 366(9497): 1653-66.
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223): 497-506.
- Caress JB, Castoro RJ, Simmons Z, Scelsa SN, Lewis RA, Ahlawat A, et al. COVID-19-associated Guillain-Barré syndrome: The early pandemic experience. Muscle Nerve. 2020; 62(4): 485-491
- Jacobs BC, Rothbarth PH, van der Meché FG, Herbrink P, Schmitz PI, de Klerk MA, van Doorn PA. The spectrum of antecedent infections in Guillain-Barré syndrome: a case-control study. Neurology. 1998; 51(4): 1110-5.
- Singh R, Shiza ST, Saadat R, Dawe M, Rehman U. Association of Guillain-Barre Syndrome With COVID-19: A Case Report and Literature Review. Cureus. 2021; 13(3): e13828.

