Case report - Volume 3 - Issue 3
Spontaneous maxillary mucocele: Diagnosis and management
Bechraoui Rim1; Jbali Souheil2* Ghabi Marwene1; Khaldi Amira1; Mediouni Azza1; Turki Senda3; Besbes Ghazi1
1ENT HNS department, La Rabta Hospital, Tunis University of Medicine, University Tunis El Manar, Tunis, Tunisia.
2ENT HNS department, Salah Azaiez Institute of Cancer, Tunis University of Medicine, University Tunis El Manar, Tunis, Tunisia.
3ENT HNS department, ISF Hospital, Tunis University of Medicine, University Tunis El Manar, Tunis, Tunisia.
Received Date : April 08, 2023
Accepted Date : May 15, 2023
Published Date: May 22, 2023
Copyright:© Jbali Souheil 2023
*Corresponding Author : Jbali Souheil, ENT HNS department, Salah Azaiez Institute of Cancer, Tunis, Tunisia.
Email: jbalisouheil@gmail.com
DOI: Doi.org/10.55920/2771-019X/1443
Abstract
Introduction and Importance: Paranasal sinus mucoceles are benign lesion that usually result from tumors, inflammation and face trauma. Seldom, these lesions can occur spontaneously. Delayed diagnosis or inadequate management can result in severe complications.
Case Presentation: We report a case of a 67 -year-old man with no medical or surgical rhinological history, referred to our department for fortuitous discovery on imaging of a mass of the maxillary sinus. Facial pain was the only complaint of the patient. Computed tomography and magnetic resonance imaging confirmed the diagnosis of mucocele. The patient had endoscopic surgery with uneventful evolution.
Keywords: Maxillary sinus, Spontaneous, Mucocele.
Introduction
Maxillary sinus mucocele is a rare and benign lesion that accounts for approximately 10% of all paranasal sinus mucoceles [1]. Although it is a slow growing tumor, it can cause bone erosion and remodeling [2] resulting in facial asymmetry, pain and other symptoms depending on its extension. We report in this study a case of spontaneous maxillary mucocele causing facial and hard palate deformity.
Case presentation
A 67 -year-old man was referred to our department for evaluation and treatment of a left midfacial deforming mass. At the beginning, it was not clinically apparent and was incidentally discovered on a CT scan without contrast done four months previously to explore an ischemic stroke. There was no history of cranial trauma or rhinological complaints. Presenting symptoms were limited to a slight inflammatory facial pain evolving for one year. On clinical examination, a painful left sided swelling of the face without visible skin lesions was observed (Figure 1). A left palatal submucosal swelling was present on examination of the oral cavity (Figure 1). This same tumefaction was present on the endo-nasal endoscopic examination deforming the inter sinuso-nasal septum.
The CT scan showed a hypodense opacification of the left maxillary sinus eroding its bony walls. It measured 40 * 30 * 46 mm with a liquid density according to the CT scan Hounsfield scale approximation. The other paranasal sinuses were normal (figure 2).
Magnetic resonance imaging (MRI) confirmed the CT scan findings showing the left maxillary sinus mass with the following features: hyper-signal T2, hypo-signal T1 and Gadolinium peripheral enhancement. Besides the erosion of the left maxillary sinus walls, the left orbit floor was eaten up and lost its integrity (Figure 4).
Endoscopic sinus surgery was performed under general anesthesia. It consisted of a wide opening of the maxillary sinus with mucocele marsupialization. The postoperative course was uneventful.
Discussion
Mucoceles are benign, mucus-containing cystic lesions. They are gradually expanding lesions involving paranasal sinuses. They usually result from an obstruction within the normal drainage ostia of paranasal sinuses leading to pent up secretions and a gradual expansion of the sinus cavity volume [3].

Figure 1: Physical examination of the patient: cheek and palate swelling (red arrows).
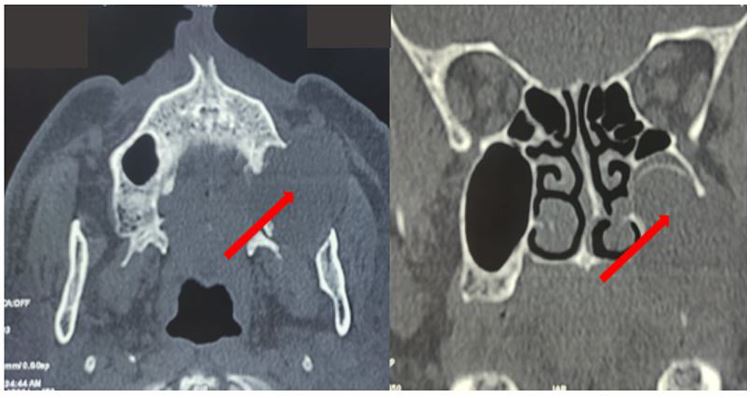
Figure 2: CT scan without contrast (axial and coronal sections): hypodense left maxillary image (red arrows).
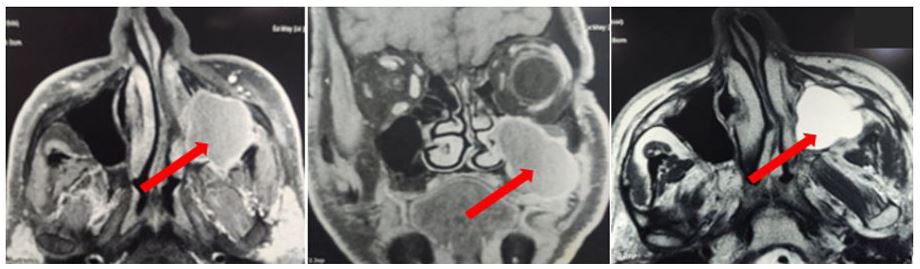
Figure 3: Contrasted Magnetic Resonance Imaging (MRI) (axial and coronal T1-weighted sections and axial T2-weighted section): hyper-signal T2, hypo-signal T1 and Gadolinium peripheral enhancement of a left maxillary sinus mass (red arrows).
Mucocele is said to be secondary if there is an identifiable cause behind it, such as craniofacial trauma, chronic rhinosinusitis or paranasal sinus surgery [4,5]. In some cases, there is no clear cause, the mucocele is then considered as spontaneous as illustrated by our case report.
Maxillary and sphenoid sinuses are less affected by this pathology than ethmoidal and frontal sinus [6]. Early diagnosis is often challenging due to this lesion slow growing and the poor clinical presentation which boils down to non-specific rhinological signs such as rhinorrhea, nasal obstruction, hemi-facial pain or swelling [7,8].
Although benign, mucoceles of the maxillary sinus can cause bony walls erosion and extend beyond the sinus cavity causing ophthalmic complications and facial deformities as illustrated by our case report. Sinus cavities’ CT scan is essential for diagnosis and extension assessment [9]. CT scan is, indeed, efficient in detection of bone remodeling and erosion.
Surgery is the treatment of choice in paranasal sinus mucoceles. Surgical approach is usually endoscopic but can be external or mixed depending on the extension assessment and the availability of a technical endoscopic surgery tray. In all cases, surgery consists of a marsupialization of the cystic lesion, cleaning of its contents and middle meatotomy when considering the maxillary sinus [10, 11]. In skilled hands, the endoscopic approach is associated with fewer complications compared to external approaches. However, the experienced surgeon must be wary of insufficient marsupialization, source of synechiae and recurrences. It is also necessary to keep in mind the idea of a possible tumoral process associated with the mucocele in which case biopsy specimens must be sent for histological examination [12].
A CT scan may be indicated afterwards. It helps to assess marsupialization quality, sinus vacuity and possible re-ossification of sinus walls [13]. The follow-up in our case is insufficient to judge evolution. Paranasal sinuses’ mucoceles can recur several years after surgery [14]. The recurrence rate varies according to authors from 3 to 35% [15]. In all cases, follow-up should be as long as possible.
Conclusion
Mucoceles of the maxillary sinus are rare. Their diagnosis is often evoked when exteriorized or complicated. Nevertheless detecting early forms helps to avoid complications. Marsupialization through Endoscopic approach is currently the most recommended surgery technique. Clinical follow-up aided by imaging when needed is also mandatory to detect recurrences.
Patient informed Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of Interest
All the authors declare no conflict of interest and have no financial or personal gains and benefits from this work.
Funding
This research did not receive any specific fundings
References
- Costan VV, Popescu E, Stratulat SI. A new approach to aesthetic maxillofacial surgery: surgical treatment of unilateral exophthalmos due to maxillary sinus mucocele. J Craniofac Surg. 2013; 24(3): 914-6.
- Durr ML, Goldberg AN. Endoscopic partial medial maxillectomy with mucosal flap for maxillary sinus mucoceles. Am J Otolaryngol. 2014; 35(2): 115-9.
- Sreedharan S, Kamath MP, Hegde MC, Bhojwani K, Alva A, Waheeda C. Giant mucocoele of the maxillary antrum: a case report. Indian J Otolaryngol Head Neck Surg. 2011; 63(1): 87-8.
- Devars du Mayne M, Moya-Plana A, Malinvaud D, Laccourreye O, Bonfils P. Sinus mucocele: natural history and long-term recurrence rate. Eur Ann Otorhinolaryngol Head Neck Dis. 2012; 129(3): 125-30.
- Scangas GA, Gudis DA, Kennedy DW. The natural history and clinical characteristics of paranasal sinus mucoceles: a clinical review. Int Forum Allergy Rhinol. 2013; 3(9): 712-7.
- Simões JC, Nogueira-Neto FB, Gregório LL, Caparroz Fde A, Kosugi EM. Visual loss: a rare complication of maxillary sinus mucocele. Braz J Otorhinolaryngol. 2015; 81(4): 451-3.
- Abdel-Aziz M, El-Hoshy H, Azooz K, Naguib N, Hussein A. Maxillary sinus mucocele: predisposing factors, clinical presentations, and treatment. Oral Maxillofac Surg. 2017; 21(1): 55-58.
- Pyo SB, Song JK, Ju HS, Lim SY. Reconstruction of Large Orbital Floor Defect Caused by Maxillary Sinus Mucocele. Arch Craniofac Surg. 2017; 18(3): 197-201.
- Jang TY, Lee SJ, Kim KT, Choi YS. Management of postoperative mucocele of the maxillary sinus through endoscopic approach. Korean J Otolaryngol-Head Neck Surg. 2005; 48: 314-319.
- Terranova P, Karligkiotis A, Digilio E et al. Bone regeneration after sinonasal mucocele marsupialization: What really happens over time? Laryngoscope. 2015; 125(07): 1568-1572.
- Marrakchi J, Dimassi H, Chiboub D, Chahed H, Bachraoui R, Mediouni A, et al. Prise en charge chirurgicale des mucocèles naso-sinusiennes. Journal Tunisien d’ORL. 2017; (37): 20-23.
- Ba M, Tall A, Hossini A, Ly Ba A, Ndoye N, Sakho Y, et al. Les mucocèles du sinus frontal en milieu neurochirurgical : A propos 6 cas. Africain journal of neurological sciences. 2005; 24(2) : 40-46.
- Ferrie JC, Klossek J-M. Les mucocèles sphénoïdales, J. Neuroradiol, 2003; 30 : 219-223.
- Rombaux P, Ledeghen S, Hamoir M, Bertrand B, Eloy P, Coche E, et al. Computer assisted surgery and endoscopic endonasal approach in 32 procedures. Acta Otorhinolaryngol Belg. 2003; 57(2):131-7.
- Beasley NJP, Jones NS. Paranasal sinus mucoceles: modem management. AJR. 1995; 9: 251-256.

