Case report - Volume 3 - Issue 3
Maxillary’s cystic lymphangioma: A rare location
Bechraoui Rim1; Jbali Souheil2*; Khaldi Amira1; Mediouni Azza1; Turki Senda3; Besbes Ghazi1
1ENT HNS department, La Rabta Hospital, Tunis University of Medicine, University Tunis El Manar, Tunis, Tunisia.
2ENT HNS department, Salah Azaiez Institute of Cancer, Tunis University of Medicine, University Tunis El Manar, Tunis, Tunisia.
3ENT HNS department, ISF Hospital, Tunis University of Medicine, University Tunis El Manar, Tunis, Tunisia.
Received Date : April 08, 2023
Accepted Date : May 16, 2023
Published Date: May 23, 2023
Copyright:© Jbali Souheil 2023
*Corresponding Author : Jbali Souheil, ENT HNS department, Salah Azaiez Institute of Cancer, Tunis, Tunisia.
Email: jbalisouheil@gmail.com
DOI: Doi.org/10.55920/2771-019X/1444
Abstract
Lymphangiomas are benign hamartomas of the lymphatic vessels. They are congenital malformations that are usually present at birth or diagnosed within the first two years of age. Almost 75% of lymphangiomas occur in the head and neck region. Its occurrence in the maxillary antrum is one of the rarest locations. Very few cases have been reported in the literature. We report a case of maxillary sinus’ lymphangioma in a 73 year old female patient which presented for a 2 years evolving 3 cm right cheek swelling. Complete surgical excision was done without later recurrence.
Keywords: Lymphangiomas; Hamartoma; Maxillary sinus.
Introduction
Lymphangiomas are developmental malformations that arise from the proliferation of the sequestered lymphatic tissues during embryogenesis. It is a benign congenital lymphatic malformation [1]. It is usually diagnosis in children under 2 years old [2]. In adults, cystic lymphangioma (CL) is a fairly rare disease [3]. Its etiology remains unclear, but it is supposed to be congenital or to result from the lymph fluid pathway obstruction and its retention in the developing lymphatic vessels. Head and neck is the main region affected probably due to the rich lymphatic network in this area. Usually lymphangiomas are asymptomatic, painless and slow growing. Associated symptoms result rather from the nearby structures local compression [4,5]. Treatment options of these lymphangiomas include surgical excision when possible, cryotherapy, sclerotherapy, laser photocoagulation, chemotherapy and radiotherapy [6].
Case presentation
A 73-year-old female without past medical history presented to otolaryngology department for a right-sided painless cheek swelling, hypoesthesia and anosmia. She does not complaint of associated symptoms such epistaxis or nasal obstruction. This symptomatology dated back to 2 years before her first consultation.
Physical examination showed the right cheek mass with an intact overlying skin. It was tender in consistency and there was no associated lymph nodes on the neck palpation. A decreased sensitivity in the V2 nerve territory was noted without any facial nerve deficiency. Nasal endoscopy showed a polypoid mass of the right middle meatus.
On CT scan, this mass was described as a right maxillary tumoral process with osteolysis, extension to the anterior subcutaneous tissues, the infra-temporal fossa and to the adjoining nasal fossa (Figure 1).
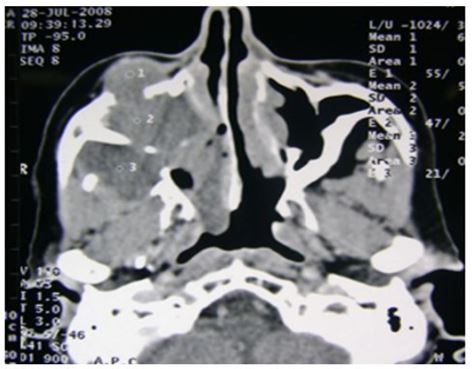
Figure 1: Face bones CT scan (axial section): hypodense tumor formation of the right maxillary sinus.
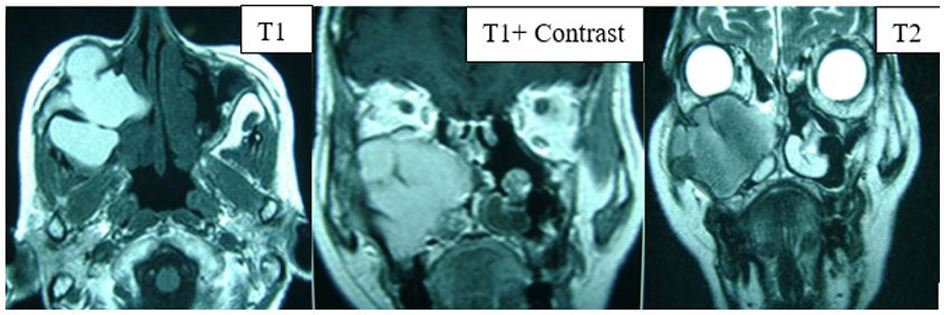
Figure 2: Face bones MRI (axial and coronal sections): Tumor located in the right maxillary sinus with a hypersignal on T1 sequences and iso-signal on T2 sequences and slight enhancement after gadolinium injection.
These findings were supported by Magnetic resonance imaging (MRI) showing a 4x4x3 cm tumor located in the right maxillary sinus, which was in hypersignal on T1 sequences and iso-signal on T2 sequences with slight enhancement after gadolinium injection (Figure 2).
The patient underwent surgical excision under general anesthesia using Caldwell Luc approach. Intraoperatively, the tumor adhered to cheek muscles, to the orbit bony floor and extends to the infratemporal fossa through a large lysis of the maxillary sinus’ posterior wall. The surgical procedure was completed by a reaming of the different sinus walls and opening of the inter-sinuso-nasal septum. The entire surgical specimen was sent for histopathological examination.
Macroscopically, cysts bigger than 3cm were observed. Microscopically, the mass was composed by a variety of dilated lymph vessels involved in a fibrovascular stroma. The diagnosis of cystic lymphangioma was, then, retained. At the date, 5 years follow-up after surgery, no relapses were noticed.
Discussion
Lymphangiomas are vascular malformations that usually occur in neonates and children below 2 years with no sex predilection. According to some authors [3], several hypotheses can explain the origin of this malformation: the first hypothesis suppose a blockage or arrest of the normal primitive lymphatic network growth during embryogenesis. The second hypothesis, suppose that the proliferation of the primitive lymphatic sac is insufficient to reach the venous system. The third one and probably not the last suppose a wrong proliferation of lymphatic tissues in wrong sites during embryogenesis.
The incidence of lymphangiomas ranges from 1,2 to 2,8 cases per 1000 live births and account for about 30% of all the lesions that arise from the lymphatic vessels [6]. Head and neck has a marked predilection for the lesion, in which case, it is more localized in the posterior triangle of the neck, submandibular and parotid regions. In the oral cavity, the tongue is the usually affected site followed by the palate, buccal mucosa, gingiva and the lips [7].
Based on the histopathology, lymphangiomas are categorized into simplex (small lymphatic vessels with thin walled endothelium), cavernous (dilated lymphatic vessels with surrounding adventitia) and cystic lymphangiomas (huge lymphatic vessels with surrounding fibrovascular tissues and smooth muscle) [2]. In the indexed literature, only one case of cystic lymphangioma located in the maxillary sinus was reported [9]. The symptomatology in this location associates nasal obstruction and may mimic chronic sinusitis. As all tumors of face bones, accurate location, local extension and relationship to the surrounding organs should be evaluated through cross-sectional imaging (CT scan and MRI).
Immunohistochemical study can help to confirm the diagnosis when there is doubt about other vascular malformations. Some markers were, indeed, described in this pathology. We can cite D2-40 (Monoclonal antibody to Podoplanin): a specific lymphatic endothelial that marks the lymphatic vessels sparing the blood capillaries. Other specific lymphatic markers were also reported including LYVE-1 (lymphatic vessel endothelial HA receptor-1), VEGR3 (vascular endothelial growth factor receptor 3) and Prox1 [7].
Genetic studies have showed mutations in the vascular growth factor (VEGF-C) and its receptors in patients diagnosed with lymphangiomas [2].
Lymphangiomas can be treated with a wide range of treatment modalities according to their extent and location. These therapeutic options include sclerotherapy, radio frequency, photodynamic treatment and surgery when possible. Our patient was treated surgically. Only complete excision is the guarantor of non-recurrence later.
Conclusion
Lymphangiomas’ maxillary localization of is exceptional. Treatment in this case does not differ from other locations and surgery is preferred when possible. However, recurrence after surgery was reported in 40% of cases, all locations combined. Thus, early diagnosis allows appropriate treatment and reduces recurrence situations. Nevertheless, long-term follow-up is constantly required.
Patient informed Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of Interest
All the authors declare no conflict of interest and have no financial or personal gains and benefits from this work.
Funding
This research did not receive any specific fundings.
References
- Dos Santos G T, Dos Santos J M, Pinheiro Soares L G, Silva Santos N R, Dos Santos J N, Barbosa Pinheiro A L. Surgical Treatment of Oral Lymphangiomas with CO2 Laser : Report of Two Uncommon Cases. Braz Dent J. 2010; 21(4): 365-369.
- M Kheur S M, Routray S, IngaleY, Desai R S. Lymphangioma of Tongue: A Rare entity Indian Journal of dental advancements. 2011; 3(3): 635-637.
- Hudson J.W. Submucoal lymphangiomas of the maxillary sinsus: Journal of oral and Maxillofacial surgery. 2003; 61: 390-392.
- Rao A P, Reddy N V, Krishnakumar R, Nirma R M, Muhammed S, Louis C J. Oral lymphangioma presenting as multiple papular lesions of the lip: Hong Kong Dent J. 2011; 8: 107-10.
- Gigue`re C M, Bauman N M, Sato Y, Burke DK, Greinwald J H, Pransky S, et al. Treatment of Lymphangiomas with OK-432 (Picibanil) Sclerotherapy: Arch Otolaryngol Head Neck Surg. 2002; 128: 1137-1144.
- Grasso D L, Pelizzo G, Zocconi E, Schleef J. Lymphangiomas of the head and neck in children: ACTA Otorhinolarynologica Italica. 2008; 28: 17-20.
- Vasconcelos M G, Santos B C, Peixoto Lemos L C, Ribeiro B F, Paraíso Iglesias D P, Vasconcelo R G. Oral lymphangioma: case report. Réseau de recherche en santé buccodentaire et osseuse. 2011; 8(3): 352-6.
- Motahhary P, Sarrafpour B, Abdirad A. Bilateral symmetrical lymphangiomas of the gingiva: case report. Diagnostic Pathology. 2006; 1: 9.
- Price C. Cystic lymphangioma in the maxillary sinus: a case report. British journal of oral surgery. 1976; 14: 41-46.

