Case report - Volume 3 - Issue 3
Radiologic issue in central venous catheter insertion in children: A rare case report
Samileh Noorbakhsh1*; Haleh Pashaii2; Mohammad Radgoodarzi3
1Full professor in Pediatric Infectious Disease, Pediatric Infectious Diseases department, Iran University of Medical Sciences, Tehran, Iran.
2Fellowship in Pediatric infectious disease, Pediatric Infectious Diseases department, Iran University of Medical Sciences, Tehran, Iran.
3Associate professor in Pediatric Cardiology, Pediatrics department, Iran University of Medical Sciences, Tehran, Iran.
Received Date : April 10, 2023
Accepted Date : May 17, 2023
Published Date: May 24, 2023
Copyright:© Samileh Noorbakhsh 2023
*Corresponding Author : Samileh Noorbakhsh, Departement of Pediatric Infectious Diseases, 4th floor Hazrat Rasul Hospital, Niayesh Street, Satarkhan Avenue, Tehran, 14455 Islamic Republic of Iran.
Email: Samileh_noorbakhsh@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1445
Abstract
Back ground: Central venous catheterization (CVCs) is a procedure, used widely in healthcare facilities. In addition, use of subcutaneous central venous catheter, known as portal catheter, is spreading among pediatric patients in need of several injections.
Case presentation: Here we present a 12-year-old boy with proven acute lymphocytic leukemia (ALL). The patient had received three courses of chemotherapy, and it was planned to receive his 4th course of chemotherapy by subcutaneous CVCs. The portal catheters were inserted for receiving chemotherapy. The patient was admitted with generalized weakness and fever and finally diagnosed with bacterial endocarditis. In spite of the correct location of the catheter tip in the superior vena cava in the primary chest x-ray, the tip was shown to be located in the right atrium in the secondary evaluations using echocardiography. Fatal Infective endocarditis superimposed on tip of CVC in cardiac chamber.
Conclusion: Re-evaluating the catheter tip seems to be beneficial in patients with high risk of tip migration for early diagnosis and preventing its consequent complications.
Keywords: Infective endocarditis; pediatrics; children. Central Venous Catheter; Tip Migration.
Introduction
Central venous catheterization was used first in 1929 and the subclavian vein was introduced as an access to the central veins in 1952. On the other hand, silicon catheters were used in 70s to access the central veins [1,2]. Walser et al described indications, implantation technique, follow-Up, and complications the portal catheter in 2012 [1] Radiologic placement of long-term central venous peripheral access system portsin 150 patients [2]. There are limited contraindications for portal catheter insertion, including severe coagulopathy, sepsis, and not tolerating subcutaneous devices in case of burn, trauma, and other connective tissue disorders in the chest wall [1-2]. Currently, the portal catheters are known as subcutaneous central venous catheters, with minimum interference with the patients’ lifestyle and providing easy access to the central vein for injection and blood sampling. In addition, use of interventional radiology approaches have facilitated the portal catheter insertion in the recent years [2-4]. The immediate and short-term complications of portal catheterization includes bleeding, air emboli, pneumothorax, catheter tip dislocation, catheter migration, cardiac perforation, arrhythmia, and infections (3-5). Merrer et al showed complications of femoral and subclavian venous catheterization in critically ill patients [3]. Schwarz et al analysed device-related morbidity factors of transcutaneously tunneled central venous lines in cancer patients [4].
Marcy et al fully described the central venous access: techniques and indications in oncology [5]. Among these complications, catheter tip dislocation is a major mistake, which can yield to arrhythmia or catheter malfunctioning [6-9]. Wright et al showed the correct position of central venous catheter tip position on chest radiographs [6].
Prabaharan et al reported the migration of central venous catheter tip following extubation [7]. Also,electrocardiography-controlled central venous catheter tip positioning in patients with atrial fibrillation [8]. P-wave amplitudes by intracavitary electrocardiogram was used by Wang et al for Tip position of peripherally inserted central catheter in cancer patients [9]. In last decade ,indwelling central venous catheters (CVCs) widely used in children.especially in cancer patients for chemotherapy reatment [10-15].
Infectious complication of central vein catheter is so important and more common in children. According to Fratino et al study, the Central venous catheter-related complications in children with oncological/hematological diseases,Overall, 234 complications were documented: 93 infectious complication rate per 1000 catheter days at risk (CR) = 0.87], 84 malfunctioning (CR = 0.78), 48 mechanical (CR = 0.45) and nine thrombotic (CR = 0.08) [10] . They conclouded that CVCs may cause complications in up to 40% of patients [10].
The rates of infectious complications reported by Levi et [11] were lower than for tunneled central venous catheters. Accidental dislodgement is not uncommon and may be prevented by use of sutures, occlusive dressing, and education of patients, families, and medical staff [11].
Jurmanji reported the CVCs complication in 1807 children. Complications necessitating catheter removal occurred in 20.8%. These included accidental dislodgement (4.6%), infection (4.3%), occlusion (3.7%), local infiltration (3.0%), leakage (1.5%), breakage (1.4%), phlebitis (1.2%), and thrombosis (0.5%) [12]. Pediatric ICU exposure and age younger than 1 year were independently associated with complications necessitating removal of CVCs [12].
Infective endocarditis is an uncommon disease in pediatric group. During past decades, inspite of great advancements in clinical practice to improve outcomes in patients with infective endocarditis, when it happen can lead to severe complication even death [13-14]. The most common causative organisms are Staphylococcus aureus and the viridans group of streptococci [15,16]. Alhalimi presented a rare case of infective endocarditis caused by P. luteola in a young female patient after being on a long-term peripherally inserted central venous catheter [15].
In addition to congenital heart diseases as the most common risk factor, predisposing conditions, such as CVCs insertion or children with chronic debilitating conditions in previously healthy children with no medical history are also seen [15-17]. The spectrum of symptoms varies widely in children and this produces difficulty in the diagnosis of infective endocarditis. Infective endocarditis in children is reliant on the modified Duke criteria [14-16]. Diagnosis is complex, although it has improved with the use of multimodal imaging techniques .Imaging techniques used include echocardiograms, computed tomography and positron emission tomography [28,19]. Biomarkers utilised in diagnosis are C-reactive protein, with recent literature reviewing the use of interleukin-15 and C-C motif chemokine ligand for reliable risk prediction. The American Heart Association (AHA) and European Society of Cardiology (ESC) guidelines have been compared to describe the differences in the approach to infective endocarditis in children. Medical intervention antibiotic treatment should be started early, according to causative microorganism and risk factors. Surgical interventions (repair and replacement of cardiac valves) might be added to treatment .However, complications are frequent and continue to cause significant morbidity [17,18].
Changing the pediatric pattern of Infective endocarditis during recent years published [19,20]. At least 3 Iranian studies defined the changing pattern of infective endocarditis in Iran like as other part of world [21-23]. Hajihossainlou et al reported (2013) the changing pattern of infective endocarditis in Iran [22]. On the country scale, age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR), age-standardized mortality rate (ASMR), and age-standardized DALYs rate changed The ASIR and ASPR of endocarditis increased, and the ASMR and age-standardized DALYs rate declined over the past 30 years in Iran, nearly all the provinces followed the same pattern with North Khorasan having the Highest ASIR, ASPR, ASMR, and DALYs rates in both years. High systolic blood pressure (SBP) had the greatest attributed burden among risk factors [23].
Here, we report a young patient with CVC tip malposition and finally died due to Infective endocarditis superimposed on tip of CVC.
Case Report
The patient was a 12-year-old boy with proven diagnosis of acute lymphocytic leukemia (ALL) during 6 months ago. He received three courses of chemotherapy and was planned to receive his fourth course. The patient experienced chills and 39 degrees fever after receiving his third course of chemotherapy, followed by a generalized weakness. He was admitted for having 860 white blood cells and 37000 platelets in each mL of his blood, in his complete blood test (CBC) test, in addition to having c-reactive protein (CRP) of 63. The initial lab tests after admission are shown in Table 1.
Table 1: The initial lab tests of the patient.
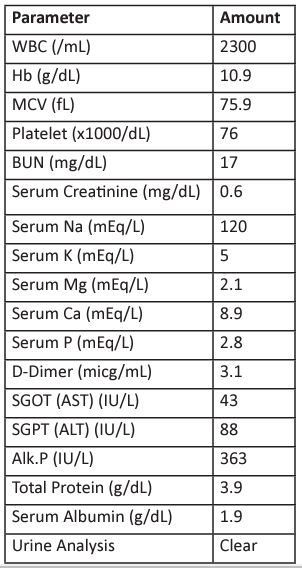
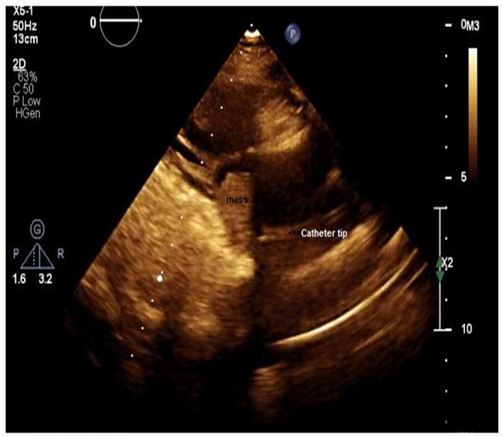
Figure 1: A large relatively fixed mass in the right atrium, with inappropriate location of the catheter tip, in favor of infectious endocarditis.
The mass was removed by a cardiac surgeon and reported as a vancomycin-resistant enterococci, sensitive to linezolid. The patients experienced multiple hyponatremic episodes, got covid-19 infection, and positive blood culture of acinetobacter, sensitive to colistin, cefepime, and ampicillin-sulbactam. A secondary chest CT-scan was taken, showing covid-19 infection besides inappropriate port access catheter location, into the right atrium. The repeated echocardiography also showed a fixed 1.5cm x 1cm mass in the right atrium. (Figure 2).
The patient was intubated in his 16th day of admission due to severe respiratory distress and received appropriate antibiotic therapy in combination with other conservative treatments. However, he had bradycardia and dropped O2 saturation in his 30st day of admission and expired, in spite of 60 minutes of standard cardiopulmonary resuscitation.
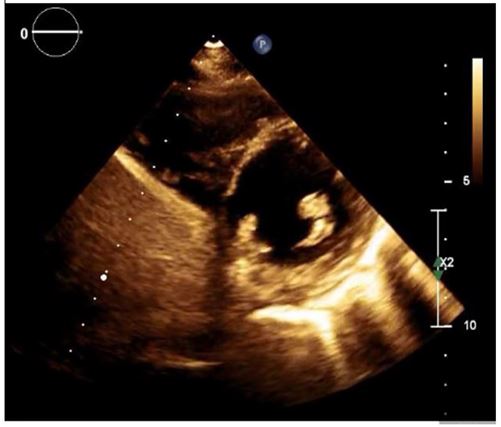
Figure 2: A Fixed 1.5cm x 1cm mass in the right atrium.
Discussion
Inserting a central venous catheter is an intervention, performed in the healthcare facilities widely. In addition, subcutaneous central venous catheter, or portal catheter, is a newly developed technique, mainly used by patients in need for long-term multiple injections, such as patients with cancer [1]. The location of the catheter tip has a key role in the occurrence of short-term and long-term side effects, including catheter flip, thrombosis, and arrhythmia.
It is believed that cavoatrial junction, identified as two vertebral bodies below carina, is the optimal location for catheter tip. Locating the tip above this level can increase the risk of catheter flip by Valsalva maneuver. Every guideline currently have suggested confirming the catheter tip using an imaging modality [4,5].
In this paper, a 12-year-old boy is presented, diagnosed with ALL 6 months ago and started receiving chemotherapy using portal catheter. The appropriate location of the catheter tip was confirmed by chest X-ray. The patient was admitted due to generalized weakness, fever, leukopenia, and thrombocytopenia. Endocarditis was diagnosed for the patient, with inappropriate location of the catheter tip, using echocardiography which can explain the patient’s deteriorating condition. There are multiple suggestions in confirming catheter tip location, using the inserted length or chest X-ray images [6]. However, tip malpositioning was evident in the reported patient. It is suggested that any activity, associated with increased chest pressure can be a risk for catheter tip migration. These activities include coughing, sneezing, lifting heavy weights, some rapid body movements, vomiting, or even extubation [7]. As the presented patient had covid-19 infection with recurrent coughs, the tip migration and its consequences were not out of expectation. However, instant imaging techniques, including chest X-ray and chest CT-scan record one frame and the catheter tip can temporarily get out of the atrium, due to the chest pressure alteration during recording the image.
There are currently modalities, including chest X-ray and chest CT-scan, which can help in locating the catheter tip. The echocardiography can also be a useful modality, as used in this patient. In addition, there are studies evaluating the electrocardiography evidences to estimate the location of the catheter tip. On the other hand, the real-time nature of echocardiography technique can help the physician to monitor the tip location for a period of time to make sure about the temporary alterations of the catheter tip location [8,9]. It seems that locating the tip of the catheter using real-time techniques such as echocardiography can be beneficial in patients at risk of tip migration and prevent its consequent adverse effects.
Changing pattern of infective endocarditis in Iran like as other part of world happened in last decade [21-23]. Infective endocarditis reported due to CVCs insertion by some authors [12,15]. Karuru et al reported the infective endocarditis-induced complete closure of a ventricular septal defect and complete heart block in a child [16]. In addition to congenital heart diseases as the most common risk factor for infective endocarditis , predisposing conditions , such as CVCs insertion or children with chronic debilitating conditions in previously healthy children with no medical history are also seen [15-17].
They reported the CVCs complication in 1807 children [12]. Complications necessitating catheter removal occurred in 20.8%. These included accidental dislodgement (4.6%), infection (4.3%), occlusion (3.7%), local infiltration (3.0%), leakage (1.5%), breakage (1.4%), phlebitis (1.2%), and thrombosis (0.5%) [12]. Pediatric ICU exposure and age younger than 1 year were independently associated with complications necessitating removal of CVCs [12].
Also, Alhalimi presented a rare case of infective endocarditis caused by P. luteola in a young female patient after being on a long-term peripherally inserted central venous catheter [15]. According to Ahmadi et al study (2014) in Isfahan( central part of Iran)during 5 years survey of infective endocarditis in children (41% of patients < 2 years and 70% aged < 6 years), 76.5% of patients had a history of congenital heart disease or cardiac surgery. Like here, Coagulase-negative staphylococci (23.5%) and Staphylococcus aureus (11.7%) were the most common organisms [21].
Strengths of study
Extreme use of diagnostic imaging and laboratory tests for rapid diagnosis in our case .The reports for CVs complication in young cases are limited. Limitations of study: retrospective single case report. The prospective reports for complication of CVs in children are helpful .
Conclusion
Re-evaluating the catheter tip seems to be beneficial in patients with high risk of tip migration for early diagnosis and preventing its consequent complications.
Ethics approval and consent to participate: Written informed consent was obtained from the parents of the patient for publication of this study. This study has adhered to the principles of Helsinki rules.
Availability of data and material: The datasets used during the current study are available from the corresponding author on reasonable request.
Competing interests: The authors declare no conflict of interest in preparing this study.
Funding: This case presentation funded by Iran University of Medical Sciences Faculty of Medicine.
Consent for publication: All authors confirmed that the manuscript has not been and will not be published elsewhere. The consent for publication of personal detailed data
All figures of our manuscripts are original
Acknowledgment: The authors would like to thank the Rasoul Akram Hospital for their technical assistance.
References
- Walser EM. Venous Access Ports: Indications, Implantation Technique, Follow-Up, and Complications. Cardiovasc Intervent Radiol. 2012; 35: 751-64.
- Foley MJ. Radiologic placement of long-term central venous peripheral access system ports (PAS Port): results in 150 patients. J Vasc Interv Radiol. 6: 255- 62.
- Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001; 286: 700-7.
- Schwarz RE, Coit DG, Groeger JS. Transcutaneously tunneled central venous lines in cancer patients: an analysis of device-related morbidity factors based on prospective data collection. Ann Surg Oncol. 2000; 7: 441-9.
- Marcy P-Y. Central venous access: techniques and indications in oncology. Eur Radiol. 2008; 18: 2333-44.
- Wright D, Williams D. Central venous catheter tip position on chest radiographs. Anaesthesia. 2020; 75: 124-5.
- Prabaharan B, Thomas S. Spontaneous migration of central venous catheter tip following extubation. Saudi J Anaesth. 2014; 8: 131.
- Steinhagen F, Kanthak M, Kukuk G, Bode C, Hoeft A, Weber S, et al. Electrocardiography-controlled central venous catheter tip positioning in patients with atrial fibrillation. J Vasc Access. 2018; 19: 528-34.
- Wang X, Yang Y, Dong J, Wang X, Zheng Y, Chen J, et al. A comparative study on the tip position of peripherally inserted central catheter inserted at two forward P-wave amplitudes by intracavitary electrocardiogram in cancer patients. Ann Palliat Med. 2021; 10: 10228-35.
- G Fratino, AC Molinari, S Parodi, S Longo, P Saracco, E Castagnola, et al. Central venous catheter-related complications in children with oncological/hematological diseases: an observational study of 418 devices. Annals of Oncology. 2005; 16(4): 648-654.
- I Levy 1, M Bendet, Z Samra, I Shalit, J Katz. Infectious complications of peripherally inserted central venous catheters in. childrenPediatr Infect Dis J. 2010; 29(5): 426-9.
- KJumani; Si Advani, N G. Reich, L Gosey, A M. Milstone, Risk Factors for Peripherally Inserted Central Venous Catheter Complications in Children. JAMA Pediatr. 2013; 167(5): 429-435.
- L Vicent, R Luna, M Martínez-Sellés. Pediatric Infective Endocarditis: A Literature Review.Journal of Clinical Medicine. 2022.
- Van Dijck I, Budts W, Cools B, Eyskens B, Boshoff D, Heying R, et al. Infective endocarditis of a transcatheter pulmonary valve in comparison with surgical implants. Heart. 2014; 101(10):788-793.
- A A Alhalimi, L T AlShammari, A Kh Al-Qurayn, A S Al Rashed. Infective Endocarditis Caused by Pseudomonas luteola in a Pediatric Patient: A Case Report and Literature Review. Am J Case Rep. 2022; 23: e935743-1-e935743-5.
- U Karuru, J Relan, ShS. Kothari, S K Gupta, and S Talwar. Infective endocarditis-induced complete closure of a ventricular septal defect and complete heart block in a child. Ann Pediatr Cardiol. 2021; 14(4): 527-529.
- Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. ESC Guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015; 36(44): 3075-3128.
- Chambers ST, Murdoch D, Morris A, Holland D, Pappas P, Almela M, et al. American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young and the Council on Cardiovascular and Stroke Nursing (2015) Infective endocarditis in childhood: 2015 update: a scientific statement from the American Heart Association. Circulation. 2015; 132(15): 1487-1515
- L Eleyan,A AKhan, G Musollari, A S Chandiramani, S Shaikh,A Salha, A Tarmahomed et al. Infective endocarditis in paediatric population. European Journal of Pediatrics. 2021; 180: 3089-3100.
- L Vicent, R Luna, M Martínez-Sellés. Pediatric Infective Endocarditis: A Literature Review. 2022; 11(11): 3217.
- Ahmadi A, Daryushi H. Infective endocarditis in children: A 5 year experience from Al-Zahra Hospital, Isfahan, Iran. Adv Biomed Res. 2014; 3: 228
- B Hajihossainlou, MA Heidarnia, B Sharif- Kashani. Changing pattern of infective endocarditis in Iran: A 16 years survey Pak J Med Sci. 2013; 29(1): 85-90
- A Ajam, P Shobeiri, MKeykhaei, S SMoghaddam, S Momtazmanesh, M Masinaei, et al. Epidemiology, burden, and attributable risks of infective endocarditis in Iran and its provinces: From 1990 to 2019. Int J Cardiol. 2022; 363: 202-20.

