Case report - Volume 3 - Issue 3
Ballooning without Compaction- Left Ventricular aneurysms in Noncompaction Cardiomyopathy
Borna Amir-Kabirian12; Fatima Ahmed MD3;Ahmad Elashery3; Bassam MoushMoush3
1Department of Internal Medicine, Charleston Area Medical Center/West Virginia University. Charleston, West Virginia, USA.
2West Virginia School of Osteopathic Medicine, Lewisburg, West Virginia, USA.
3Department of Cardiology, Charleston Area Medical Center. Charleston, West Virginia, USA.
Received Date : April 19, 2023
Accepted Date : May 25, 2023
Published Date: June 01, 2023
Copyright:© Borna Amir-Kabirian 2023
*Corresponding Author : Borna Amir-Kabirian, Department of Internal Medicine, Charleston Area Medical Center/West Virginia University. Charleston, West Virginia, USA.
Email: Borna.Amir-Kabirian@vandaliahealth.org
DOI: Doi.org/10.55920/2771-019X/1451
Abstract
Left ventricular non-compaction cardiomyopathy (LVNC) is a congenital cardiomyopathy that occurs as a result of disruption in the early stages of cardiac development. It can occur in isolation, or in conjunction with other rare congenital disorders such as a congenital left ventricular aneurysm. In the presence of LVNC, left ventircular aneurysms are thought to occur due to lack of capillary formation. Overall, there are very limited cases documenting both together. Both conditions can result in arrhythmias, thromboembolic disease, ventricular dysfunction and sudden cardiac death. Diagnosis can be made with echocardiography, although cardiac magnestic resoncnance imaging has become increasingly used for diagnosis. Treatment involves treating heart failure symptoms, arrhythmias and implantation of cardioverter-defibrillators when appropriate. Despite the few case reports on the presence of both conditions occuring simulatenously, recommedenations on treatment, including the use of therapeutic anticoagulation in this patient population needs to be looked into further.
Keywords: Congenital left ventricular aneurysm, Left ventricular non-compaction cardiomyopathy
Introduction
Left ventricular non-compaction cardiomyopathy is a rare congenital cardiomyopathy that involves prominent trabeculations and deep intertrabecular recesses in the left ventricle [1]. While the etiology of LVNC is not fully understood, it is believed to be due to a failure of the myocardium to compact the epicardium, resulting in the inhibition of the intertrabecular recesses from being compacted into capillaries [1]. Without the aforementioned capillaries, problems can arise in the microcirculation, leading to congenital left ventricular aneurysms [2].
Case
A 51-year-old male with a history of LVNC diagnosed at an outlying facility presented to a cardiology clinic for evaluation of worsening exertional dyspnea. His cardiac history was remarkable for episodes of chest pain in his late 30’s. As a result, he underwent a series of tests including a left heart catheterization (LHC) and transthoracic echocardiogram. The results of his LHC showed minimal coronary artery disease. However, his echocardiogram was concerning for hypokinesis of the mid to distal inferior, inferoseptal and apical lateral walls, along with an aberrant appearing trabeculation originating from the apex of the LV. He was treated symptomatically with instructions to follow up outpatient. The patient returned with symptoms concerning for unstable angina. He underwent a pharmacological stress test with the images revealing a moderate perfusion defect in the basal inferior wall with no significant defect reversibility, along with inferior wall hypokinesis. A repeat transthoracic echocardiogram showed a trabeculated LV, consistent with his diagnosis of LVNC. Interestingly, it also revealed left ventricular apical thinning and aneurysm formation consistent with the same area that was noted on the stress test. A subsequent cardiac MRI supported the earlier findings with a thin and aneurysmal appearing LV in the inferolateral and anterolateral wall portions (figure 1). The non-compacted LV was also noted (figure 1). The absence of left ventricular scarring excluded the possibility of prior myocardial ischemic events, therefore confirming the diagnosis of congenital left ventricular aneurysm.
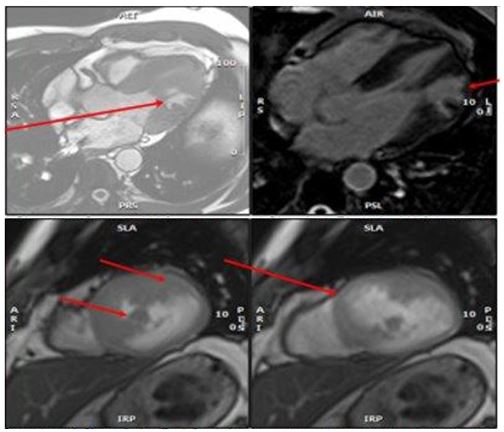
Figure 1: A) 4 Chamber Systole: LV Aneurysm
B) 4 Chamber Diastole: LV Aneurysm
C) Parasternal Short Axis: End Systole, Top arrow: Non-compacted, Bottom arrow: LV Aneurysm
D) Parasternal Short Axis: End Diastole LV Aneurysm
Discussion
LVNC, otherwise known as spongy myocardium or spongiform cardiomyopathy is a rare congenital cardiomyopathy that is believed to be the result of an arrest during normal embryogenesis [3]. Ordinarily, the ventricular walls of the left and right ventricles consist of a compacted layer of myocardial fibers. In LVNC, the left ventricular apex consists of trabeculations and deep intertrabecular recesses [1,3]. These intertrabecular recesses are not compacted into capillaries and lead to a lack of development of the microcirculation [1,4,5].
Overall, LVNC has a prevalence of just under 0.25% in the general population, and has been classified as a primary genetic cardiomyopathy by the American Heart Association in 2006 [3,4]. Cases can be familial or sporadic, and symptoms can arise at any age. Heart failure is the most common complaint at admission [3]. When associated with other congenital heart diseases, studies have shown it to be associated with a mutation in the α-dystrobrevin gene and transcription factor NKX2.5 [4].
Echocardiography has been used as the initial non-invasive diagnostic method of LVNC [6,3]. Chin et al., proposed a diagnostic criteria for LVNC in which the ratio of X/Y <0.5; where X is equal to the distance from the epicardial surface to the trabecular recess trough and Y is equal to the distance from the epicardial surface to the trabeculation peak. This method evaluated the trabeculation size relative to the compacted wall thickness in different echocardiographic views [3]. Contrast echocardiography can improve the sensitivity. Other diagnostic modalities used are cardiac magnetic resonance imaging or computed tomography. Cardiac MRI usage has increased due to its ability to capture images of the compacted and non-compacted layers with clarity; therefore, providing a better ratio of non-compacted to compacted layers [3]. On the other hand, cardiac CT is not used as often due to its limited ability to evaluate the left ventricular function [3]. It is important to distinguish LVNC from dilated cardiomyopathy, hypertrophic cardiomyopathy, acquired changes seen in pulmonary atresia, layered mural thrombus in LV, intramyocardial hematoma, mycotic invasion of the heart, or Fabry’s disease. Symptomatic patients with congestive heart failure should be treated with angiotensin-converting enzyme inhibitors, beta-blockers, diuretics afterload reducing agents or digoxin. Some patients may eventually require cardiac transplantation [3].
By itself, LVNC can predispose patients to arrhythmias, thromboembolic disease, left ventricular dysfunction, congestive heart failure, sepsis, and sudden cardiac death [6,7]. Hypertrabeculation in patients with reduced LV function are at risk of forming clots which might lead to cerebrovascular events; therefore, it is recommended to place these patients on oral anticoagulants once the diagnosis of LVNC is made [7]. Likewise, congenital left ventricular aneurysms can lead to the same disease processes [2]. Congenital LV aneurysms itself has a prevalence of approximately 0.34% [2]. In the setting of LVNC, congenital LV aneurysms are postulated to occur due to the aforementioned lack of capillary formation in LVNC, resulting in ventricular thinning and aneurysmal formation [2]. Literature review reveals only a handful of case reports with both conditions. As a result, there is limited data regarding the treatment. In one study, a patient with LVNC and left ventricular aneurysm suffered from recurring embolisms, with the authors suggesting anticoagulation be considered as an option in patients with LVNC and LV aneurysms [7]. In comparison, our patient did not suffer from thrombi, and was not on anticoagulation.
Conclusion
In conclusion, we present a case of LVNC with a congenital LV aneurysm that was diagnosed in adulthood. This case report reinforces the fact that patients with LVNC should be evaluated closely to determine if there are concurrent congenital disorders, such as a LV aneurysm.
References
- Toader D, Paraschiv A, Tudorașcu P, Tudorașcu D, Bataiosu C, Balșeanu A. Left ventricular noncompaction-a rare cause of triad: Heart failure, ventricular arrhythmias, and systemic embolic events: A case report . Journal of Medical Case Reports. 2021; 15(1).
- Sato Y, Matsumoto N, Yoda S, Inoue F, Kunimoto S, Fukamizu S, et al. Left ventricular aneurysm associated with isolated noncompaction of the ventricular myocardium. Heart and vessels. 2006; 21(3): 192-194.
- Singh DP Patel H. Left Ventricular Non-compaction Cardiomyopathy. 2022.
- Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, et al. American Heart Association, Council on Clinical Cardiology, Heart Failure and Transplantation Committee, Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups, & Council on Epidemiology and Prevention (2006). Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2012; 113(14): 1807-1816.
- Makkuni P, Kotler MN, Figueredo VM. Diverticular and Aneurysmal Structures of the Left Ventricle in Adults. 2010; 37(6): 699-705.
- Wengrofsky P, Armenia C, Oleszak F, Kupferstein E, Rednam C, Mitre CA. Left Ventricular Trabeculation and Noncompaction Cardiomyopathy: A Review. EC clinical and experimental anatomy. 2019; 2(6): 267-283.
- Ahn JH, Koh JS, Park JR, Park MJ, Min JH, Cho SY, et al. Isolated left ventricular noncompaction with a congenital aneurysm presenting with recurrent embolism. Journal of cardiovascular ultrasound. 2012; 20(2): 103-107.

