Case report - Volume 3 - Issue 3
The infective endocarditis: inflammatory markers for earlier diagnosis and corticosteroids for better renal prognosis: Case report and review of literature
Boutaleb Amine Mamoun*; Chbir Nouhaila; Drighil Abdenasser; Rachida Habbal
Cardiology Department, Ibn rochd university hospital, Morocco.
Received Date : April 21, 2023
Accepted Date : May 29, 2023
Published Date: June 05, 2023
Copyright:© Boutaleb Amine Mamoun 2023
*Corresponding Author : Boutaleb Amine Mamoun, Cardiology Department, Ibn rochd university hospital, Morocco.
Email: boutaleb.amine1@gmail.com
DOI: Doi.org/10.55920/2771-019X/1453
Abstract
Infective endocarditis (IE) is a lethal and devastating disease which can affect different cardiac structures and lead to significant morbidity and mortality in undiagnosed cases. The diagnosis is not obvious in cases of sterile blood cultures and inconclusive echocardiography results. Therefore, a profound understanding of the infective and the inflammatory pathophysiology of IE may open new tracks concerning an earlier diagnosis and more appropriate treatment. We report the case of a probable IE in a 50 years old man presenting with dyspnea NYHA III, lower limb edema and feverish feeling. Cardiac auscultation found an IV/VI grade diastolic murmur at the aortic area. Transthoracic echocardiography confirmed a type I left-right bicuspid aortic valve with severe aortic regurgitation and endocardial vegetation image. Biological assessment revealed a frank inflammatory syndrome and negative blood cultures. Despite 2 weeks of intravenous antibiotics, the biological assessment control showed renal function impairment and remaining elevated inflammatory markers. Corticosteroid was initiated with spectacular improvement of biological parameters. Infective endocarditis requires comprehensive assessment of clinical, echocardiographic and laboratory findings. Steroids may allow positive immunomodulation resulting in improved clinical outcomes of patients presenting with IE associated glomerulonephritis and major inflammatory reaction.
Keywords: Infective endocarditis; Corticosteroids; Glomerulonephritis
Introduction
Infective endocarditis (IE) is defined as an infection of the heart endocardial surfaces, usually involving one or more cardiac valves, and, to a lesser degree, the mural endocardium or a septal defect. In the Moroccan context, the incidence is not well known due to the absence of national epidemiological data. Despite major efforts to prevent IE, more than a quarter of these infections are related to healthcare measures. Treatment is based on prolonged intravenous antibiotic therapy and requires surgical intervention in more than half of the cases. The pathophysiology of infective endocarditis is complex. In the first stage, a non-bacterial thrombotic vegetation colonizes the surface of endothelial cells. This process is complicated by the formation of an infected blood vegetation during the spread of bacteremia. The inflammatory system is then activated, leading to either the disappearance or growth of the vegetation. Therefore, some complications of infective endocarditis are related to the systemic reaction. On the other hand, inflammatory markers may be helpful in establishing the diagnosis. Through this case report and review of the literature, we aim to assess the role of anti-inflammatory therapies in the context of infective endocarditis.
Case report
A 50-year-old male patient with no prior medical history presented to the cardiology department at Ibn Rochd University Hospital with dyspnea NYHA III, lower limb edema, and a feverish feeling that had been developing for one month. During physical examination, a normal heart rate and blood pressure were observed at 72 beats/min and 100/54 mmHg, respectively. Slight lower limb edema was noted. Cardiac auscultation revealed a protodiastolic murmur at the aortic area with an increased amplitude of the carotid and peripheral pulses. Pulmonary crackles were heard at the lung bases. Temperature monitoring revealed fever peaks at 38.5°C. Electrocardiogram (EKG) revealed a first-degree atrioventricular block and left ventricular hypertrophy. Transthoracic echocardiography showed a dilated left ventricle with an end-diastolic diameter (LVEDd) of 70 mm and severe aortic regurgitation. A type I left-right bicuspid aortic valve with a suspicious endocardial vegetation was observed (Figure 1,2). Left ventricular ejection fraction was evaluated at 60% using the biplane Simpson’s method.
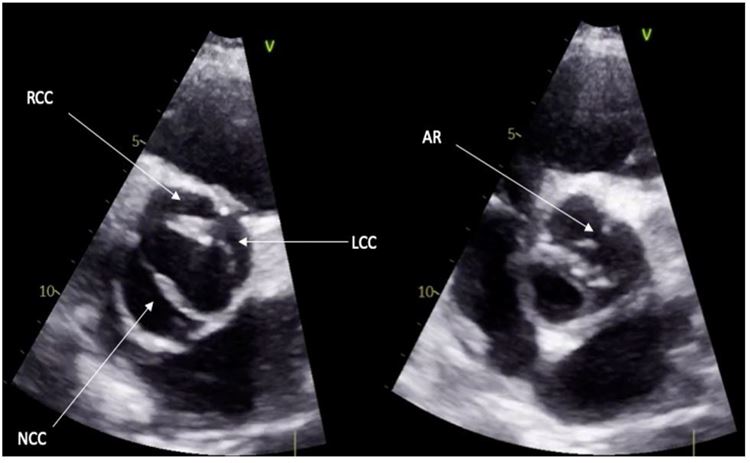
Figure 1: Parasternal short axis view demonstrating the bicuspid aortic valve.
RCC: Right-coronary cusp; LCC: Left-coronary cusp: NCC: Non-coronary cusp; AR: Aortic Raphe
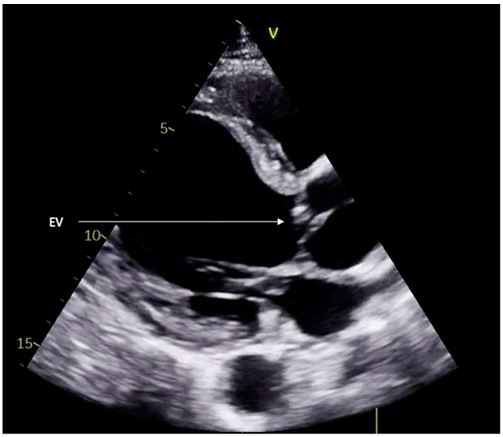
Figure 2: Parasternal long axis view demonstrating right coronary cusp prolapse and endocardial vegetation.
EV: Endocardial vegetation
All biological assessments were indicative of a marked inflammatory syndrome, showing hypochromic microcytic anemia at 10g/dl, C-reactive protein at 40 mg/l, erythrocyte sedimentation rate (ESR) at 100mm, and hyperfibrinogenemia (5.69 g/l). Repeated blood cultures were sterile. Immunological tests revealed C3 hypocomplementemia. Renal tests showed a moderate chronic renal function impairment, estimating a glomerular filtration rate (GFR) of 60 ml/min with positive proteinuria at 0.6g. Empiric intravenous antibiotic treatment was started with ceftriaxone 2g/day, associated with gentamicin 160mg/day, and biological assessment was performed twice a week.
Ten days after admission, the patient experienced acute renal failure with a GFR of 35 ml/min and an increased proteinuria value of 2.4g/24h. Due to high bleeding risk, kidney biopsy puncture was contraindicated, and infective endocarditis associated glomerulonephritis (IEAGN) was presumed based on biological parameters. Corticosteroid treatment was initiated at an initial dose of prednisolone 80mg/day and followed by a gradual decline after 2 weeks of treatment. The patient's condition improved significantly, with renal function and proteinuria improving (GFR=56ml/min vs 35ml/min) (0.42g/24h vs 1.92g/24h) and normalization of inflammatory markers.
After the patient's clinical situation improved, he was transferred to the surgical team for mechanical aortic valve replacement.
Discussion
Clinical presentations of infective endocarditis (IE) are diverse. The Duke criteria are based on pathological criteria for microorganism detection, endocarditis image detection, and clinical features requiring further assessment [3]. These criteria were revised in 2015, redefining some IE stages and adding some imaging items [4]. IE is associated with major morbidity and mortality related to its potential complications. Therefore, monitoring the disease activity should be a priority to prevent and treat these events.
In sterile blood culture IE, the different situations generally reported are related to antibiotic pre-treatment, rare and hard-to-culture bacteria, and non-infectious IE [5]. Our patient did not receive pre-antimicrobial therapy and had a negative systemic lupus erythematosus assessment, which excluded Liebman-Sacks' affection.
Recent studies have shown early elevation of inflammatory markers (especially pro-inflammatory cytokines and complement) compared to bacteriological and clinical markers in infective endocarditis. Some authors have even proposed including them among Duke's criteria [2]. Although the study of Ris et al. was a short cohort of 69 patients, the authors demonstrated that IL-15, IL-6, CCL4, and CRP levels were predictors of IE patient outcomes. The presence of these pro-inflammatory interleukins and chemokines was associated with a complicated course of IE [6].
Regarding the predominant inflammatory pattern of some IE cases, we assume that anti-inflammatory treatment may be beneficial in reducing the impact of the inflammatory system activation. The addition of anti-inflammatory therapy could theoretically lead to symptom improvement and reduction of the inflammatory markers.
Kidney disease in IE can present in various forms, including bacterial infection-related immune complex-mediated glomerulonephritis (GN), renal infarction from septic emboli, and renal cortical necrosis [7]. Acute renal failure is the main clinical feature of infective endocarditis-associated glomerulonephritis (IEAGN) and may result from acute nephritic syndrome, rapidly progressive glomerulonephritis, and nephrotic syndrome. Renal biopsy is essential in differentiating these diverse scenarios.
There is no clear consensus on the role of corticosteroid therapy in the treatment of infective endocarditis. Sporadic cases described in the literature have shown the positive impact of this treatment for disease management, especially in cases of kidney damage, as presented in our case. Through our literature review, the majority of cases were treated with low-dose and short-term steroid therapy [8].
In our case, the attack dose duration of prednisone was two weeks followed by a tapering dose with constant biological assessment every three days during hospitalization. After one month of follow-up, we noticed a spectacular improvement in renal function, normalization of proteinuria, and inflammatory markers.
Therefore, it is important to emphasize that infective endocarditis with a high inflammatory pattern may benefit from corticosteroid therapy. Through immune activity modulation, corticosteroids may contribute to improving the immunological and inflammatory phenomenon related to IE [9].
This case highlights the importance of managing the inflammatory pattern of IE through the immunomodulatory effect of steroid therapy. The perfect duration of therapy remains controversial without randomized trials.
Conclusion
The epidemiological profile and clinical presentation of infective endocarditis are constantly changing. Therefore, more studies are needed to explore the possible role of inflammatory markers and corticosteroids in establishing early diagnosis and improving clinical outcomes. The integration of corticosteroid therapy in the management of IE with a predominant inflammatory pattern is beneficial. However, close follow-up is essential to prevent long-term side effects or inappropriate reactions.
Acknowledgments
My thanks go to Professor Habbal Rachida which have supported us during all our academic formation. The manuscript has been written by Dr Chbir Nouhaila and revised by Dr Boutaleb Amine Mamoun. Pr Drighil has helped with the management of the case.
Conflicts of interest
The authors declare that there is no conflict of interests about this manuscript.
Consent statement
Written informed consent was obtained from the patient(s) for publication of this case report, including accompanying images
References
- Iversen K, Ihlemann N, Gill SU, et al. Partial Oral versus Intravenous Antibiotic Treatment of Endocarditis. N Engl J Med. 2019; 380: 415-424.
- Deviri E, Glenville BE. Review Article Inflammatory Response In Infective Endocarditis.
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994; 96: 200-209.
- Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2000; 30: 633-638.
- Naber CK, Erbel R. Infective endocarditis with negative blood cultures. Int J Antimicrob Agents. 2007; 30 Suppl 1: S32-6.
- Ris T, Teixeira‐Carvalho A, Coelho RMP, et al. Inflammatory biomarkers in infective endocarditis: machine learning to predict mortality. Clin Exp Immunol. 2019; 196: 374-382.
- Majumdar A, Chowdhary S, Ferreira MA, et al. Renal pathological findings in infective endocarditis. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. 2000; 15: 1782-1787.
- Use of Steroids in Penicillin-Sensitive Patients with Bacterial Endocarditis — A Report of Three Cases and Review of the Literature.
- Brown M, Griffin GE. Immune responses in endocarditis. Heart Br Card Soc. 1998; 79: 1-2.

