Research Article - Volume 3 - Issue 3
Otorhinolaryngology Morbidity Pattern among Patients Attending Outpatient Clinic of Suez General Hospital, Egypt
Tarek Fouad Youssef Habib1; Mohamed Rifaat Ahmed1*; Ayman Ekram Fahim2; Maram Salah-Eldin Mohammed Fawzy3
1Professor of Otolaryngology, faculty of medicine, Suez Canal University, Egypt.
2Professor of community medicine, faculty of medicine, Suez Canal University, Egypt.
3Resident of Otorhinolaryngology in Suez General Hospital, Egypt.
Received Date : April 28, 2023
Accepted Date : May 30, 2023
Published Date: June 06, 2023
Copyright:© Mohamed Rifaat Ahmed 2023
*Corresponding Author : Mohamed Rifaat Ahmed, Professor of Otolaryngology, faculty of medicine, Suez Canal University, Egypt. Tel: +20185043825.
Email: M_rifaat@hotmail.com
DOI: Doi.org/10.55920/2771-019X/1456
Abstract
Background: Otorhinolaryngological disorders constitutes to one of the major causes of morbidity in any hilly area. Morbidity pattern has several determining factors like socio-economic status, basic education, occupation of parents, socio-cultural practices, living environment. Ear, nose and throat emergencies are common in all communities. Early diagnosis and management will result in reduction of morbidity and mortality.
Aim: To describe the incidence of otorhinolaryngological disorder in Suez city to help in dealing with them.
Subjects and Methods: A Retrospective record-based study was carried in otorhinolaryngology outpatient clinic of the general hospital of Suez city. Total population was 11890 patients and this study included 4455 patients from January 2019 to December 2019. Full history of the disease and history of any other disease was taken from all patients.
Results: The otorhinolaryngological disorders found to have the highest incidence among >15 age group. Females were more affected than males. Most of patients had acute otitis media. There was predominance of male patients to female patients in age group less than 15 years old and between 25 and 45 years old, while between 15 and 24 old and more than 45 years old females were more predominant than males. The difference was statistically significant. There was predominance of male patients to female patients with ear and throat diseases. While there was predominance of female patients to male patients with nose diseases.
Conclusion: the incidence of otorhinolaryngological disorder highest among females, >15 age group, otitis media is the most common disorder.
Keywords: Allergic rhinitis; Otitis media; Tonsillitis; Sinusitis.
Introduction
Otorhinolaryngological disorders are amongst the common reason for seeking medical advice in health care setup. Otorhinolaryngological disorders constitutes to one of the major causes of morbidity in any hilly area. Poor socio-economic condition of general population and lack of proper medical facilities further aggravate Otorhinolaryngological problems [1].
The burden of disease on health care system and its impact on general wellbeing is very high and the analysis of 2000 for Global Burden of Disease (GBD) study stated that cause of morbidity (excluding injuries) is most commonly due to infectious diseases and common tropical diseases 60%, 27% due to life-style disorders and 13% due to potentially preventable per-natal conditions. It has been stated that non-communicable diseases are leading cause of death globally [5]. It has been implicated that 40% of hospital stay and 35% of outpatient visits are due to NCDs [2].
It has been noted that Otitis Media and its sequelae are the most common cause of preventable hearing loss in children in developing countries. The major burden reports in India & other developing countries by WHO is due to Chronic Suppurative Otitis Media [3].
There is indirect relationship between age of onset and chronicity of the disease, and hence risk factors that can be targeted should be identified. Overcrowding should be reduced. Health-education messages in relation to personal hygiene is developed to target known risk factors. Universal immunization practice is emphasized in view of increased risk with multiple types of H. influenzae and S. pneumoniae and a beneficial effect in reducing the number of recurrent attacks [4].
Allergic rhinitis is showing an upward trend in rural communities due to an increase in pollution, it is associated with significant comorbidities and health care costs and has been identified as one of the top ten reasons for visits to primary care clinics. Nasal polyposis was also seen in 10% of the patients which was related to chronic allergic rhinitis [5].
Oral mucosal ulcers may be related to a temporary weakness in immune system (cold or flu), hormonal changes, mechanical irritation, stress, low levels of vitamin B12, folate, iron, and ferritin [6].
Study showed that ear diseases is the most common in seeking medical advice especially in younger age group. The most common disease was impacted wax 16.51% [7].
In the general hospital of Suez city in past January there were 65% of cases had otitis media aged (20-40) years old, 40% of them had suppurative otitis media aged (1-12) years old. 25% of cases had allergic rhinitis. In past June, there were 58% of cases had suppurative otitis media and 12% of cases had vertigo aged (20-60) years.
Materials and Methods
Study design
A Retrospective record-based study design.
Study setting and Study population
This study was carried out in otorhinolaryngology outpatient clinic of the general hospital of Suez city. All patients who attended or referred to Otorhinolaryngology outpatient clinics of the general hospital of Suez city. Total population was 11890 patients and this study included 4455 patients from January 2019 to December 2019.
Inclusion criteria
- Gender: male or female.
- Age: all age groups.
Exclusion criteria
- Subjects who were unable to ambulate.
- Patients with pharmacological treatment for any other disease.
Sample Size Justification
Based on that the of allergic rhinitis = 19.58% (General Suez Hospital, 2019). The sample size was equal to 4010 subjects. Adding a drop-out proportion of 10% gives a total sample size of 4455 subjects. Patients were included by systematic random method from records.
Data collection tool
All patients were subjected to:-
Full history of the disease and history of any other disease was taken.
Statistical analysis
Using SPSS software - version 22 was used. Tables and graphs were used for data presentation according to need - frequency, percentage, and mean and stander deviation for the results were calculated. Dependent T test was used for comparison of discrete data. Student t test was used to compare continuous data. P value was set at < 0.05 for significant results and 0.005 for highly significant results.
Ethical Considerations
Local ethical committee faculty of medicine approved the study protocol.
Results
Age distribution of patients in the study population:
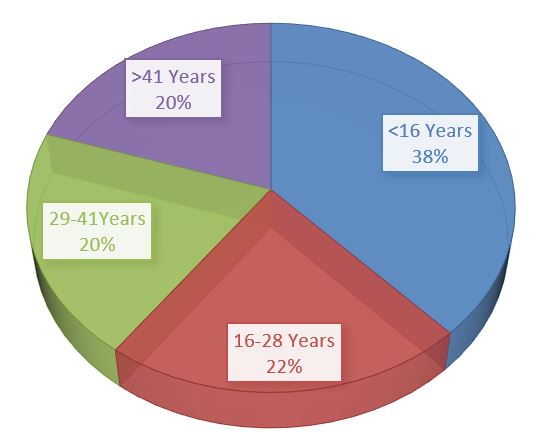
A shown in (figure 1), The department of ENT over one year managed a total number of 4010 patients. Among them, 1524 (38%) were less than 16 years old, 883 (22.02%) were between 16 and 28 years old, 802 (20%) were between 29 and 41 years old & 801 (19.98%) were more than 41 years old.
Figure 1: Age distribution among the study patients.
Gender distribution of patients
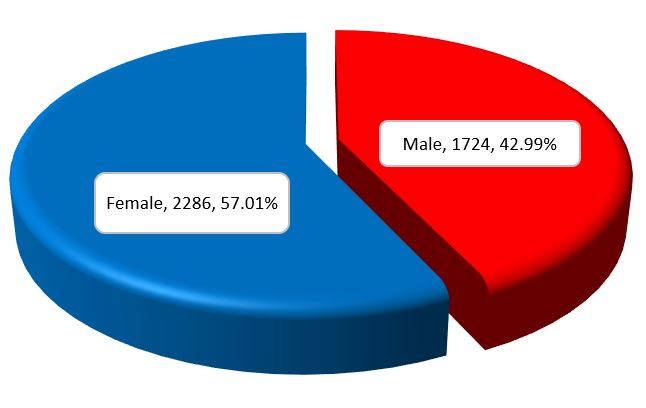
As shown in (figure 2), there was predominance of female patients to males, that 1724(42.99%) of patients were males & 2286(57.01%) of them were females.
Figure 2: Gender distribution of the study patients.
Distribution of manifestations among ENT disorders in the study:
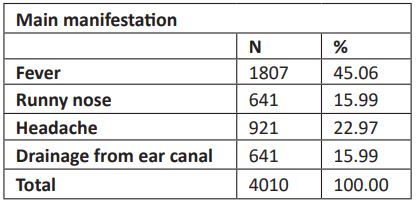
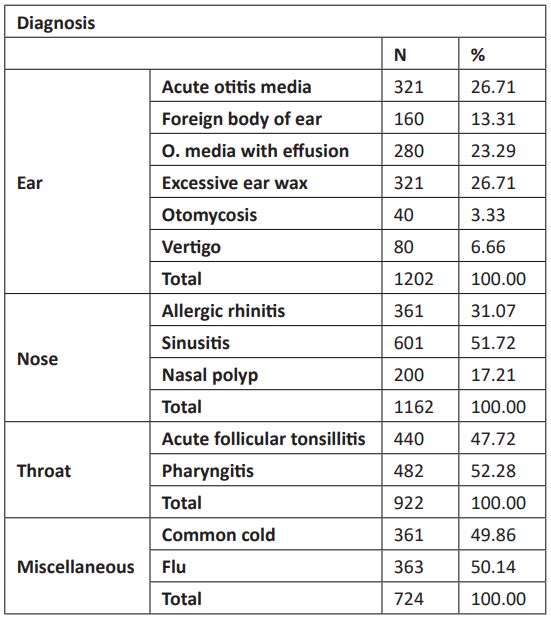
Table 1 showing that, the main symptom was fever in 1807(45.06%), then headache in 921(22.97%) & drainage from ear canal and runny nose in 641(15.99%) equally.
Table 1: Distribution of manifestations among ENT disorders in the study.
Distribution of ear, nose, and throat diseases in the study:
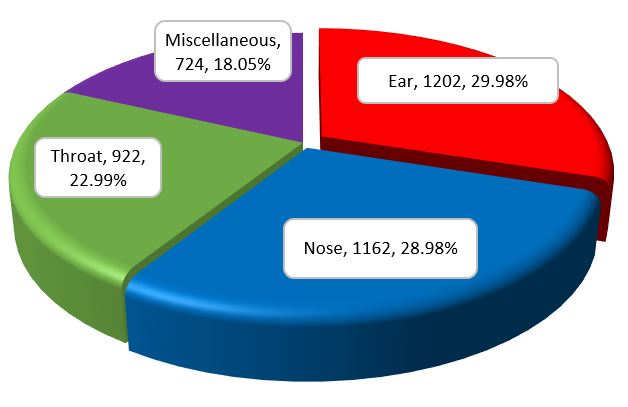
Figure 3 showing that patients with ear diseases were 1202 (29.98%), patients with nose diseases were 1162 (28.98%), patients with throat diseases were 922 (22.99%) and patients with Miscellaneous were 724 (18.05%)
Figure 3: Respiratory distress characteristics in the neonate of both groups.
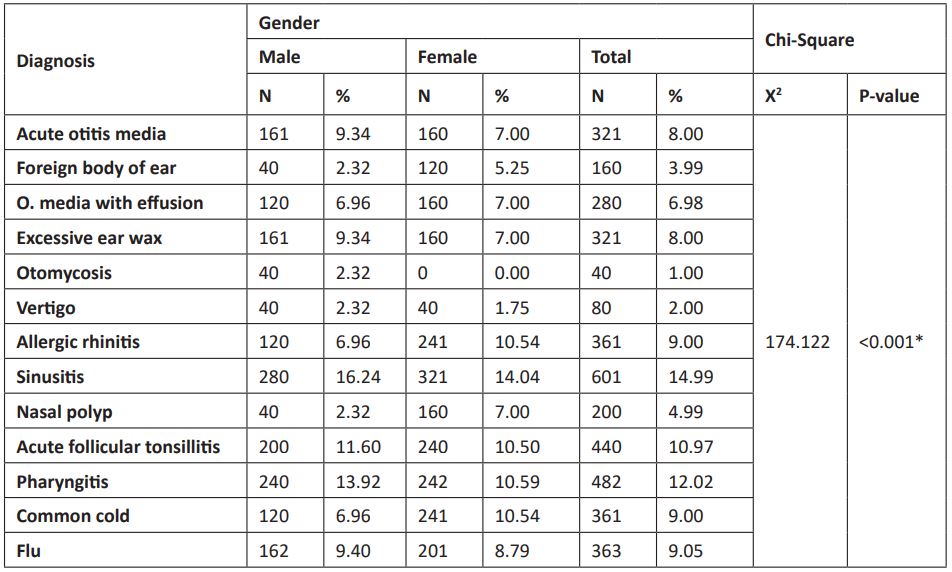
Distribution of diagnosis in the study:
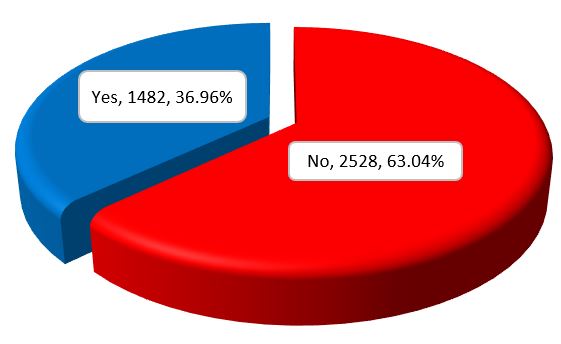
Table 2 shows that according to the study, patients which had acute otitis media were 321(8%), patients which had foreign body in ear were 160(3.99%), patients which had otitis media with effusion were 280(6.98%), patients which had excessive earwax were 321(8%), patients which had otomycosis were 40(1%), patients which had vertigo 80(2%), patients which had allergic rhinitis were 361(9%), patients which had sinusitis were 601(14.99%), patients which had nasal polyps were 200(4.99%), patients which had acute follicular tonsillitis were 440(10.97%), patients which had pharyngitis were 482(12.02), patients which had common cold were 361(9.05) and patients which had flu were 363(9.05).
Table 2: Distribution of diagnosis in the study.
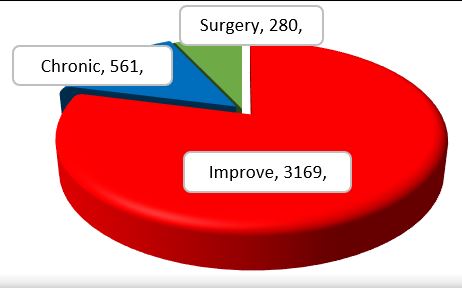
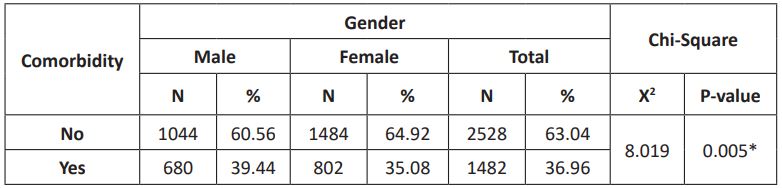
Comorbidity of ENT diseases:
Figure (4) showing that, there were 1482 patients (36.96%), had comorbid diseases.
Figure 4: Comorbidity of ENT diseases.
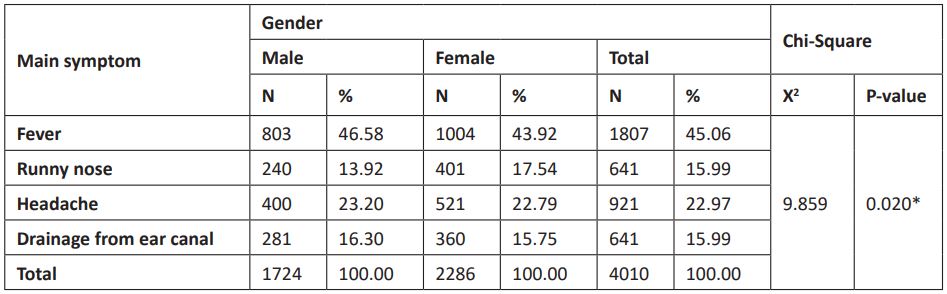
Prognosis of ENT diseases in the study:
Figure 5 demonstrates that according to the study, 3169(79.03%) of patients improved with treatment, 561(13.99%) of patients had chronic diseases and 280(6.98) of them underwent surgical management.
Figure 5: Prognosis of ENT diseases in the study.
Relation between age & gender with ENT diseases:
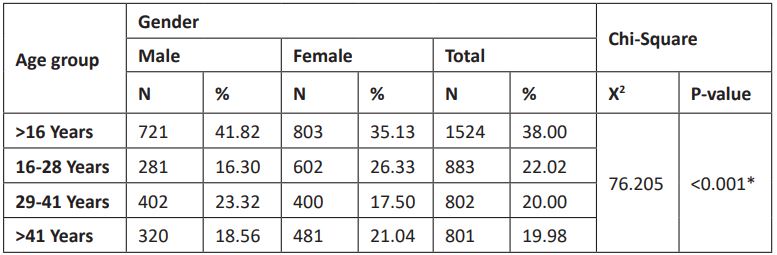
According to the study, there were predominance of male patients to female patients in age group less than 16 years old (41.82: 35.13%). There was predominance of female patients to male patients between 16 and 28 old (26.33: 16.30%). There was predominance of male patients to female patients between 29 and 41 years old (23.32: 17.50%). There was predominance of female patients to male patients more than 41 years old (21.04: 18.56%). The difference was statistically significant (p <0.001)., as shown in (table 3).
Table 3: Relation between age & gender with ENT diseases.
Relation between age & gender with ENT diseases:
Table 4 showing that according to the study, there were predominance of male patients to female patients with fever (46.58: 43.92%). There was predominance of female patients to male patients with runny nose (17.54: 13.92%). there was predominance of male patients to female patients with headache (23.20: 22.79%). there was predominance of male patients to female patients with drainage from ear canal (16.30: 15.75%). The difference was statistically significant (p=0.020).
Table 4: Relation between gender and main symptom in the study.
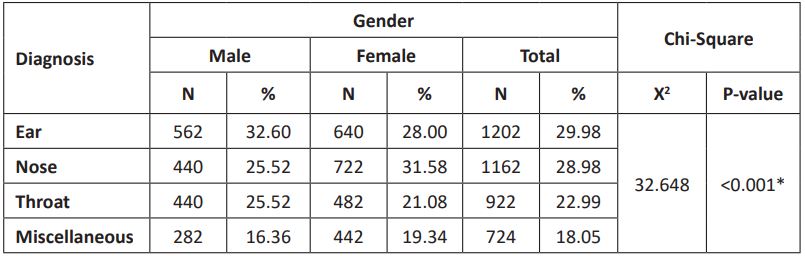
Relation between gender and diagnosis of ENT diseases:
Table 5 showing that according to the study, there were predominance of male patients to female patients with ear diseases (32.60: 28.00%). There was predominance of female patients to male patients with nose diseases (31.58: 25.52%). There was predominance of male patients to female patients with throat diseases (25.52: 21.08%). There was predominance of female patients to male patients with Miscellaneous diseases (19.34: 16.36%). The difference was statistically significant (p <0.001).
Table 5: Relation between gender and diagnosis of ENT diseases.
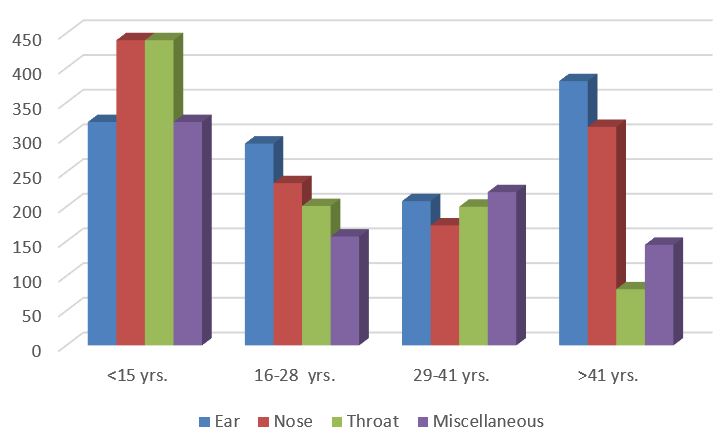
Relation between age and diagnosis of ENT diseases:
Figure 6 shows that, there were predominance of age group < 15 years old with nose and throat diseases. While ear disease was predominant among age >41 years old. The difference was statistically significant (p <0.001).
Figure 6: Relation between gender and diagnosis of ENT diseases.
Relation between gender and each disease among ENT diseases:
Table 6 showing that, there were predominance of male patients to female patients with Acute otitis media (9.34: 7.00%). There was predominance of female patients to male patients with Foreign body of ear (5.25: 2.32%). There was predominance of female patients to male patients with O. media with effusion (7.00: 6.96%). There was predominance of male patients to female patients with Excessive ear wax (9.34: 7.00%). Patients suffer from otomycosis were males (2.32%). There was predominance of male patients to female patients with Vertigo (2.32: 1.75%). There was predominance of female patients to male patients with Allergic rhinitis (10.54: 6.96%). There was predominance of male patients to female patients with Sinusitis (16.24: 14.04%). There was predominance of female patients to male patients with Nasal polyp (7.00: 2.32%). There was predominance of male patients to female patients with Acute follicular tonsillitis (11.60: 10.50%). There was predominance of male patients to female patients with Pharyngitis (13.92: 10.59%). There was predominance of female patients to male patients with Common cold (10.54: 6.96%). There was predominance of male patients to female patients with Flu (9.40: 8.79%). The difference was statistically significant (p <0.001).
Table 6: Relation between gender and each disease among ENT diseases.
Relation between gender and investigations for patients in the study:
Table 7 showing that there were 964 patients had investigated for Complete blood count, 361 (20.94%) were males and 603(26.38%) were females. There were 842 patients had investigated for CT scan of sinuses, 360(20.88%) were males and 482(21.08%) were females. The difference was statistically significant (p <0.001).
Table 7: Relation between gender and comorbidity with other diseases among the study.
Relation between gender and comorbidity with other diseases among the study:
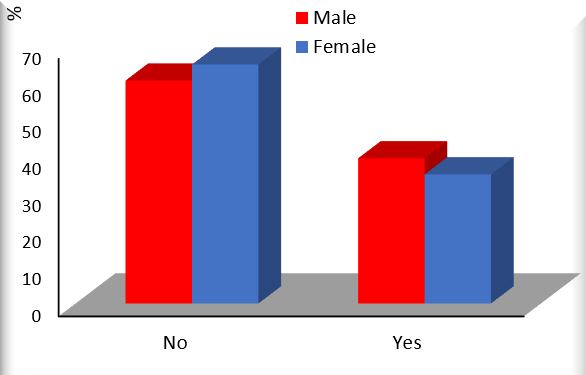
Figure 7 shows that, 680 (39.44%) male patients had comorbid diseases and 802 (35.08%) female patients had comorbid diseases. The difference was statistically significant (p=0.005*).
Figure 7: Relation between gender and comorbidity with other diseases among the study.
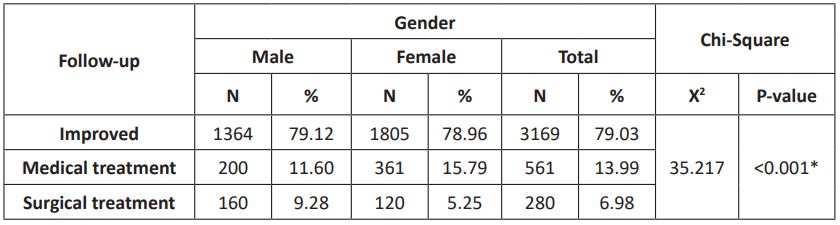
Relation between gender and prognosis among the study:
Table 8 demonstrates that, the improved patients were 1364 (79.12%) males and 1805 (78.96%) females. Patients on medical treatment were 200 (11.60%) males and 361 (15.79%) females. Patients with surgical management were 160 (9.28%) males and 120 (5.25) females, which was statistically significant (p <0.001).
Table 8: Relation between gender and comorbidity with other diseases among the study.
Discussion
Otorhinolaryngological disorders are amongst the common reason for seeking medical advice in health care setup. Otorhinolaryngological disorders constitutes to one of the major causes of morbidity in any hilly area. Morbidity pattern has several determining factors like socio-economic status, basic education, occupation of parents, socio-cultural practices, living environment. Ear, nose and throat emergencies are common in all communities. Early diagnosis and management will result in reduction of morbidity and mortality [1].
The current study was carried in otorhinolaryngology outpatient clinic of the general hospital of Suez city over one year and managed a total number of 4010 patients. Among them, 1524 (38%) were less than 15 years old, 883 (22.02%) were between 15 and 24 years old, 802 (20%) were between 25 and 45 years old & 801 (19.98%) were more than 45 years old.
In agreement with Surapaneni and Sisodia, study about incidence of ear, nose and throat disorders in which more than 45% cases who had disorders were concentrated in the 6-15 years age group [8]. In the same line with Anwar et al. study in which the age wise otorhinolaryngological morbidity among pediatric age group showed that no report of cases in the neonatal period and 1-4 age group was 2.63%, 5-9 age group was 36.26% and 10-14 age group was 61.11% [9].
The current study is supported by other study that there was predominance of female patients to males in ENT diseases as 13,393 (54. 48%) were of female patients, and 11,190 (45. 51%) were of male patients (117). The age groups were 0 to 15 years (22. 71% of cases), 16 to 65 years (71. 96%), and over 66 years (5. 31%) (117).
In agreement with Surapaneni and Sisodia, [8] study in which the predominant gender was females compared to males although this distribution was not significant, though a similar distribution was found in another study by Yeli [10].
Similarly, Anwar et al. study found that the otorhinolaryngological disorder among male children constituted for 29.82% whereas female children accounted for 70.18%. The difference between male and female children was statistically significant (p=0.0001) [9]. Conversely to, a study done in 2009 by Abbas et al., which demonstrated predominance of male patients to females (2.5:1) [11].
In the present study, most of patients suffered from fever, then headache & drainage from ear canal and runny nose.
Conversely, ear pain due to an infection is the most common cause in children and can occur in babies, it may or may not be accompanied by other symptoms such as fever [2], [12]. Such a variation can be accounted for a more liberal and developed social culture and equal work opportunities and exposure for men and women in a developed country like UK.
In the study, patients with ear diseases were 1202(29.98%), patients with nose diseases were 1162(28.98%), patients with throat diseases were 922(22.99%) and patients with Miscellaneous were 724(18.05%).
Similar to another study in India in which a retrospective study was conducted in a rural tertiary care teaching hospital for a period of two years. Otological, nasopharyngeal and oropharyngeal disorders were 73.67%, rhinological 7.31%, oropharhngeal 5.58% and oral cavity was 4.1% morbidity profile [9].
In Dogan et al. study in Nigar, the most common otorhinolaryngological disorders were pharyngitis (n = 2713; 38.6%), followed by tonsillitis (n = 1302; 18.5%) and rhinitis (n = 1161; 16.5%) [13].
An Egyptian study in South Sinai found that ear problems were found in 27.5% of the ears examined. The most common cause was secretory otitis media (10.8%) followed by occluded wax (9.5%). The most common cause of hearing loss in children is otitis media Secretory otitis media was highly prevalent in areas 1 (Abu Redeis) and 3 (Nuweiba) with 18.6% and 13.7% prevalence respectively [14].
In Egypt; the prevalence of hearing loss in schoolchildren (6-12 years) was reported to be 5.3% in Alexandria and 4.5% in rural areas. Another study in Ismailia governorate found hearing loss among 13.7% of schoolchildren, but they only used tympanometry to test for middle ear diseases. Recently, a national household survey reported a prevalence of hearing loss of almost 10% in children aged 5-14 years, 7;9.4% of which was mild, i.e. almost 8% of the study group had mild loss which is similar to our results, although their study was home-based and so did not only involve children in school [15].
The most common morbidity of the ear was due to Otitis media, both CSOM as well as that with effusion both together accounting for about 75% of the ear disorders. Impacted was seen in 18% of the ear disorders [9]. Biswas et al and Morris et al found the prevalence of CSOM to be 12.4% and 15 % respectively [16].
Similar was the case the most common ear disorder was Ear Wax which accounted for over 40% of the cases [10,17,18]. In Khan et al. study Ear wax was the most common ENT disorder
encountered. As in majority of cases it is asymptomatic, so they don’t seek medical attention. Reported the prevalence rates of impacted wax ranging from 8.6% to 28.2% [19,20,21].
Similar study results who found otomycosis to be present in 4.7% in the study population [18]. Presence of foreign bodies, whether animate or inanimate in the auditory canal and nasal cavity is a common feature among the preschoolers and comparatively uncommon in the older age group. This is probably these children tend to insert objects due to boredom or curiosity.
As regards nose disorders in this study, patients which had vertigo, allergic rhinitis, sinusitis and patients' nasal polyps.
Similar to study in which the most common was rhinitis which accounted for 55% of the overall cases and 60.7% of the nasal cases which was corroborated by other studies [8]. Allergic rhinitis was seen to be associated with other conditions like asthma and other allergic conditions. In our study, patients which had acute follicular tonsillitis, pharyngitis, common cold and flu [8]. While study found that pharyngitis was found most common followed by tonsillitis. The same was found in a study, whereas the prevalence of tonsillitis was more in a study [10,18].
In this study, more than third of patients had comorbid diseases with male predominance. The difference was statistically significant (p=0.005*). Similar to study in which 22.1% had comorbid diseases most of them were males [9].
According to the study, there was predominance of male patients to female patients in age group less than 15 years old and between 25 and 45 years old, while between 15 and 24 old and more than 45 years old females were more predominant than males. The difference was statistically significant (p <0.001).
Our study revealed gender variation in the morbidity pattern of otorhinolaryngological disorders. There was predominance of male patients to female patients with ear diseases. The difference was statistically significant (p <0.001). Male patients with acute otitis media, excessive ear wax and otomycosis were significantly higher than females. Meanwhile female patients to with foreign body of ear, O. media with effusion were higher than males. In Assiut during the period from October 2011 to August 2012 a total of 124 patients were clinically examined for mycotic otitis at the outpatient clinic of Otolaryngology Department, Assiut University Hospitals (AUH). 56 were males (60.9%) and 36 were females (39.1%) [22].
In study the otological and combined disorders in male children was 21.56% but in female it was 22.5% but difference between the gender was not statistically significant (p=0.07) [9].
In the present study, there was predominance of female patients to male patients with nose diseases (31.58: 25.52%). There was predominance of male patients to female patients with vertigo, sinusitis, acute follicular tonsillitis, pharyngitis and flu (p<.001). Whereas there was predominance of female patients to male patients with allergic rhinitis, nasal polyp and common cold.
In agreement to study in which nasopharyngeal and oropharyngeal disorders was higher in female (51%) but in male it was only 46% (p=0.57) which was not statistically significant [9]. In this study there was predominance of male patients to female patients with throat diseases. Other studies have found a similar male and female proportion [23]. There was a 1.19 female to male ratio - there were slightly more female patients [24]. According to the study, the improved patients were 1364 (79.12%) males and 1805 (78.96%) females. Chronic patients were 200 (11.60%) males and 361 (15.79%) females. Patients with surgical management were 160 (9.28%) males and 120 (5.25) females, which was statistically significant (p <0.001). Similar to Italian study which found that there was also significant
sex differences in ENT, in terms of epidemiology, anatomy, audiology, inflammation, infectious diseases, pain and cancer. Female showed more chronic course than females, while male had the most ENT emergencies than females [25].
Conclusion
The otorhinolaryngological disorders have the highest incidence among >15 age group. Females were more affected than males. Regarding ear diseases, most of patients had acute otitis media, then foreign body in ear, otitis media with effusion, excessive earwax and then otomycosis. As regards nose disorders in this study, patients had vertigo, allergic rhinitis, sinusitis and nasal polyps. There was predominance of male patients to female patients in age group less than 15 years old and between 25 and 45 years old, while between 15 and 24 old and more than 45 years old females were more predominant than males. The difference was statistically significant. Our study revealed gender variation in the morbidity pattern of otorhinolaryngological disorders. There was predominance of male patients to female patients with ear and throat diseases. While there was predominance of female patients to male patients with nose diseases.
References
- Homoe P, Kvaerner K, Casey JR, Damoiseaux RAMJ, van Dongen TMA, Gunasekera H. Panel 1: Epidemiology and Diagnosis. Otolaryngol Head Neck Surg. 2017; 156(4_suppl): S1-21.
- Graydon K, Waterworth C, Miller H, Gunasekera H. Global burden of hearing impairment and ear disease. J Laryngol Otol. 2019; 133(1): 18-25.
- Chando S, Young C, Craig JC, Gunasekera H, Tong A. Parental views on otitis media: systematic review of qualitative studies. Eur J Pediatr. 2016; 175(10): 1295-305.
- Klein JO. Otitis media. Clin Infect Dis. 1994; 19(5): 823-33.
- Emerson, L. P., Job, A., & Abraham V (2013). A model for provision of ENT health care service at primary and secondary hospital level in a developing country. BioMed Research International, 2013.
- Greenberg MS, Pinto A. Etiology and management of recurrent aphthous stomatitis. Curr Infect Dis Rep [Internet]. 2003; 5(3): 194-8.
- Khanam A, Akhtar G, Hossain F, Chowdhury NN, Rahman MA. Pattern of Otolaryngological Diseases among Paediatric Population Attending ENT OPD in a Tertiary Care Centre, Dhaka. Delta Med Coll J. 2017; 5(1): 30-4.
- Swamy KM, Ganiger A. Incidence of ear, nose and throat disorders in children - A observational study in District Hospital at Koppal. MedPulse Int J ENT. 2019; 11(1): 12-5.
- Anwar MM, Jesudoss A, Gowarthan S, Thirumalaikolundu Subramanian P, Prabhusaran N. Spectrum of otorhinolaryngological disorders among hospitalized adults in a tertiary care teaching hospital. Int J Otorhinolaryngol Head Neck Surg. 2018; 5(1): 36.
- Suman SY. Prevalence of ENT disorders in children : A tertiary medical care study. Online J Otolaryngol [Internet]. 2015; 5(3): 16.
- Abbas I, Fayyaz M, Shah I, Khan MA, Qazi SH, Munir N. Demographic distribution of maxillofacial fractures in Ayub Teaching Hospital: 7-year review. J Ayub Med Coll Abbottabad. 2009; 21(2): 110-2.
- Gupta AK, Garg R, Gupta A, Bajaj K. A retrospective analysis of 189 patients of maxillofacial injuries presenting to a tertiary care hospital in Punjab, India. J Maxillofac Oral Surg. 2009; 8(3): 241-5.
- Dogan M, Duman A. Epidemiological profiles of otorhinolaryngological disorders in adults admitted to the emergency room of a tertiary university hospital. Niger J Clin Pract. 2019; 22(1): 41-5.
- Yamamah G, Mabrouk A, Ghorab E, Ahmady M, Abdulsalam H. Middle ear and hearing disorders of schoolchildren aged 7-10 years in South Sinai, Egypt. East Mediterr Health J. 2012; 18(3): 255-60.
- Abdel-Hamid O, Khatib OMN, Aly A, Morad M, Kamel S. Prevalence and patterns of hearing impairment in Egypt: a national household survey. East Mediterr Health J. 2007; 13(5): 1170-80.
- Biswas AC, Joarder AH, Siddiquee BH. Prevalence of CSOM among rural school going children. Mymensingh Med J. 2005; 14(2): 152-5.
- Valley S. ASSESSMENT OF EPIDEMIOIOGICAL PROFILE OF VARIOUS ENT DISEASES IN ASSESSMENT OF EPIDEMIOIOGICAL PROFILE OF VARIOUS. 2016.
- Nepali R, Sigdel B. Prevalence of ENT Diseases In Children: Hospital Based Study. Internet J Otorhinolaryngol. 2012; 14(2): 2-6.
- Hatcher J, Smith A, Mackenzie I, Thompson S, Bal I, Macharia I. A prevalence study of ear problems in school children in Kiambu district, Kenya, May 1992. Int J Pediatr Otorhinolaryngol. 1995; 33(3): 197-205.
- Elango S, Purohit GN, Hashim M, Hilmi R. Hearing loss and ear disorders in Malaysian school children. Int J Pediatr Otorhinolaryngol. 1991; 22(1): 75-80.
- Minja BM, Machemba A. Prevalence of otitis media, hearing impairment and cerumen impaction among school children in rural and urban Dar es Salaam, Tanzania. Int J Pediatr Otorhinolaryngol. 1996; 37(1): 29-34.
- Moharram AM, Ahmed HE, Nasr SA-M. Otomycosis in Assiut, Egypt. J Basic Appl Mycol [Internet]. 2013; 4: 1-11.
- Gallo A, Moi R, Minni A, Simonelli M, de Vincentiis M. Otorhinolaryngology emergency unit care: the experience of a large university hospital in Italy. Ear Nose Throat J. 2000; 79(3): 155-158,160.
- Furtado PL, Nakanishi M, Rezende GL, Granjeiro RC, Oliveira TS de. Clinic-epidemiological analysis of an otorhinolaryngology emergency unit care in a tertiary hospital. Braz J Otorhinolaryngol. 2011; 77(4): 426-31.
- Zanon A, Martini A. Gender differences in otolaryngology: An overview. Ital J Gender-Specific Med. 2018; 4(3): 101-7.