Case report - Volume 3 - Issue 3
Unmasking the truth: Progressive multifocal leukoencephalopathy – immune reconstitution inflammatory syndrome (PML-IRIS) in a 36-year old male with HIV, A case report
Jon Stewart H. Dy1*; Samantha Anne S. Gutierrez1; Ryan M. Llorin2; Mercedes De Leon Dizon3; Eric Gerard Maglaya3; Hans Ludwig F. Damian1
1Institute for Neurosciences, St. Luke’s Medical Center, Quezon City, Philippines
2Department of Medicine, St. Luke’s Medical Center, Quezon City, Philippines
3Institute of Radiology, St. Luke’s Medical Center, Quezon City, Philippines
Received Date : May 01, 2023
Accepted Date : June 05, 2023
Published Date: June 12, 2023
Copyright:© Jon Stewart Dy 2023
*Corresponding Author : Jon Stewart. Dy, Samantha Anne S. Gutierrez, Institute for Neurosciences, St. Luke’s Medical Center, Quezon City, Philippines
Email: jonjondy@gmail.com
DOI: Doi.org/10.55920/2771-019X/1459
Abstract
Progressive Multifocal Leukoencephalopathy – Immune Reconstitution Inflammatory Syndrome (PMLIRIS) is the subacute onset of neurological deficits that appeared or was exacerbated after initiation antiretroviral therapy (ART) for treatment of PML. It is due to severe neuroinflammation with re-establishment of immuncompetence. Approximately 25% of patients with HIV and PML develop IRIS. Clinical trials on the treatment of PML-IRIS is lacking with only limited evidence supporting the use of investigative therapies such as corticosteroids and Maraviroc. We report a case of a 36-year old Filipino male, known hypertensive and diagnosed with HIV, who presented with memory problems. He was eventually treated as a case of PML-IRIS on the 3rd week after initiation of ART. He was treated with a course of intravenous Dexamethasone, oral Mefloquine and intravenous immunoglobulin, and ART was continued. Clinical outcome in our patient shows an overall improvement of symptoms and no deterioration of neurologic deficits.
Introduction
Progressive multifocal leukoencephalopathy (PML) is a rare, serious and often fatal demyelinating disease caused by the JC (John Cunningham) virus characterized by subacute progressive neurologic deficits. Motor, speech and cognitive impairments are the most frequent initial presentations [1]. It most commonly occurs in the setting of immunosuppression, and the most commonly underlying illness is HIV/AIDS, accounting for more than 80% of cases. [2] In about 5% of patients with HIV-associated PML, it is the heralding manifestation of AIDS that occur in patients with CD4 count of <200 cells/ul. Because of the widespread use of ART, the prevalence of PML has declined over the past two decades. [3] There is currently no established antiviral treatment effective against the JC virus. Hence, the goal is re-institution of immunocompetence to control JC virus replication. In HIV-infected patients, Antiretroviral therapy (ART) is the only therapy with a proven benefit on PML outcome. Over the years, anecdotal reports regarding effective use of various agents such as Mefloquine, Mirtazapine, Cytarabine, Cidofovir and Maraviroc have been published but these are yet to be proven by larger clinical trials. The challenge in developing an effective antiviral agent is the absence of an animal model since the JC virus is exclusive to humans [2].
Progressive Multifocal Leukoencephalopathy Immune Reconstitution Inflammatory Syndrome (PMLIRIS) is characterized by neurologic worsening after reestablishment of immunocompetence with ART. IRIS can unmask PML or paradoxically worsen a preexisting PML. Investigational studies have studied the use of corticosteroids and Maraviroc but studies have not shown a consistent benefit and there is lack of evidence on its efficacy for HIV-related PML-IRIS. We present a case of PML-IRIS in a 36-year old male who was treated with intravenous dexamethasone, Mefloquine, intravenous immunoglobulin with continuation of ART.
Case report
The patient is DC, a 36-year old male, right-handed, known hypertensive from the Philippines. He presented with a chief complaint of memory problems. He is a mechanical engineer now managing a business. At baseline the patient was cheerful, sociable and optimistic. Starting September 2019, the patient was noted to be withdrawn, less engaged in conversations and easily irritated. He would lock himself in the room most of the day. These changes in mood and behavior persisted and were not associated with other symptoms until first week of October 2019 when he was reported to have periods of disorientation and memory lapses. He also had difficulty recalling recent events and names of friends. Despite these, he remained independent in all activities of daily living (ADLs). There was no sleep disturbance, fatigue, loss of appetite, expression of fear or grief, violent behavior or suicidal ideations. No illusions, hallucinations, delusions, hypersexuality, excessive eating or apathy. There was no fever, headache, vision changes, weakness, numbness, incontinence, change in sensorium or seizures. On October 30, 2019, he consulted with a general practitioner in China. Cranial CT and blood tests were done but the results were unrecalled. No medications were given but he was advised an MRI and neurology consult. He then flew back to the Philippines and consulted at Philippine Heart Center where he was seen by an internist. He underwent and Cranial MRI with Contrast and was advised to transfer to our institution for further tests.
Neurologic examination showed a patient who appeared to be calm, well-kempt and in a good mood but with blunt facial expression, low voice volume. There were no facial or body gestures. He was fluent with some word-finding difficulty. There was impaired naming, intact comprehension and repetition, and no apraxia. There was impaired calculation. There was no agraphia, finger agnosia, and right-left disorientation. No agraphesthesia, astereognosis, and visual or tactile neglect were noted. The patient’s MOCA-E score was 22/30 and MMSE score was 23/30. The rest of the eurologic examination was unremarkable.
Clinical Course
The patient had a total of four hospital admissions for the succeeding four months.
First hospital admission
During the first admission (October 2019), CSF analysis showed a normal opening pressure with normal glucose and protein, no cells, negative cytology and absence of oligoclonal bands. Work-up for infection was also negative. MRI findings showed T2/FLAIR hyperintensities in the splenium, right frontal lobe and the subcortical U-fibers (Figure 1A). Patient initially refused HIV screening and immunodeficiency panel. Primary impression during this time was Acute Demyelinating Disease, to consider Acute Disseminated Encephalomyelitis vs. PML. He was given Methylprednisolone 500mg/day for 3 days then shifted to tapering doses of oral Prednisone on discharge. There was noted improvement in thepatient’s attention. The rest of cognitive domains remained the same.
Second hospital admission
Prior to the second admission (November 2019), patient progressively became more withdrawn, irritable and less coherent, affecting his activities of daily living, now with associated right-sided weakness. During the second admission, neurologic exam showed a worse MOCA-E score of 5/30 points. Patient was abulic, slow to respond, incoherent with impaired comprehension, naming and repetition, with right central facial palsy and weakness of the right upper (4/5) and lower extremities (4/5) with hyperreflexia and a positive toe extensor reflex. During this admission, it was eventually revealed that the patient had multiple unprotected sexual encounters during past travels. HIV screening was positive, initial CD4 count was 39 and initial viral load was 169 copies/ml. MRI showed interval progression T2/FLAIR hyperintensities in the bilateral frontoparietal and right temporal lobes (Figure 1B and 1C). Repeat CSF analysis done showed normal results with negative findings for CSF JC virus DNA. Serum JC virus was also negative. Primary impression during this time was progressive multifocal leukoencephalopathy. ART was started using Tenofovir 300mg once daily, Lamivudine 300mg once daily and Efavirenz 600mg once daily. Mirtazapine 15mg twice daily was also started. In the course of the admission, the patient had an episode of generalized tonic-clonic seizure for which Valproic Acid was started. There was no deterioration of neurologic status and the patient was eventually discharged stable.
Third hospital admission
Prior to the third admission (December 2019), the patient was re-admitted due to progressive right-sided weakness and decrease in verbal output. He was now unable to attend to all ADLs. Neurologic examination showed global aphasia with weakness of the right lower extremity (1-2/5) more than the right upper extremity (3/5). Patient was on the third week of ART, CD4 count increased to 145 while viral load increased to 2079 copies/ml. Repeat MRI showed stable but more confluent T2/FLAIR hyperintensities in the same areas as previously stated (Figure 1D). Repeat CSF analysis or brain biopsy could not be done due to cost concerns and refusal by the patient’s siblings. Primary impression during this time was PML-IRIS. Patient was started on intravenous Dexamethasone 8mg for fivedays then shifted to tapering doses of oral prednisone, Mefloquine 250mg once daily for three days then maintained on once a week, and ART was continued. There was noted improved attention, verbal output and improved motor strength. The patient was eventually discharged stable.
Fourth hospital admission
Prior to the fourth admission, follow-up MRI (January 2019, Figure 1E) showed progression in the extent and degree of confluence of the white matter lesions in the bilateral frontoparietal and right temporal lobes. CD4 count decreased to 127 and viral load decreased to 408 copies/ml. Oral prednisone was tapered while ART, Mefloquine and Mirtazipine were continued. During the fourth admission (February 2020), there was noted progressive right-sided weakness and recurrence of seizures. Viral load decreased to 266 copies/ml. MRI (Figure 1F) showed further confluence of T2/FLAIR hyperintensities in left posterior parietal lobe. Intravenous immunoglobulin 30mg/day for 3 days was given while steroid doses were adjusted. Antiepileptics were also continued.
Clinical Outcome
Since the patient’s last admission (February to May 2020), he is now reported to have improved mood and can now engage in conversations by responding with phrases. The same degree of right-sided weakness still persists. There were no seizure recurrences. He is currently on ART, Mrtazipine, Mefloquine and oral Prednisone.
Discussion
Distinguishing between PML and PML-IRIS is difficult, as was observed in our patient’s case. Definite diagnosis of PML is made by correlating clinical and MRI findings with a confirmatory test, either a positive CSF JC virus DNA by PCR or typical histopathology on brain biopsy. Lesions in PML seen on MRI are ill defined with T2/FLAIR hyperintensity and T1 hypointensity and restricted diffusion found at the gray– white matter interface and subcortical white matter [4].
In as much as 20% of cases of confirmed PML, the CSF is negative for JCV DNA or brain biopsy is nondiagnostic. [5]. In our patient’s case, clinical and MRI findings were consistent with PML, CSF JC virus DNA was negative and brain biopsy was not done. The diagnosis of PML-IRIS requires demonstration of HIV replication control by decrease in viral load by ≥1 log10 copies/ml with or without an increase in CD4 count and with evidence of inflammatory reaction in the brain demonstrated by MRI and/or CNS histopathology (T cell infiltration) [6]. In our patient’s third admission, there was noted increase in viral load (2079 from 169), increase in CD4 count (145 from 39), and MRI showing evident and confluent inflammatory reaction in the bilateral frontoparietal lobes and right temporal lobes. Although the increase in viral load points against PMLIRIS, the progression of deficits and the significant increase in CD4 count could be considered as worsening PML secondary to immune reconstitution.
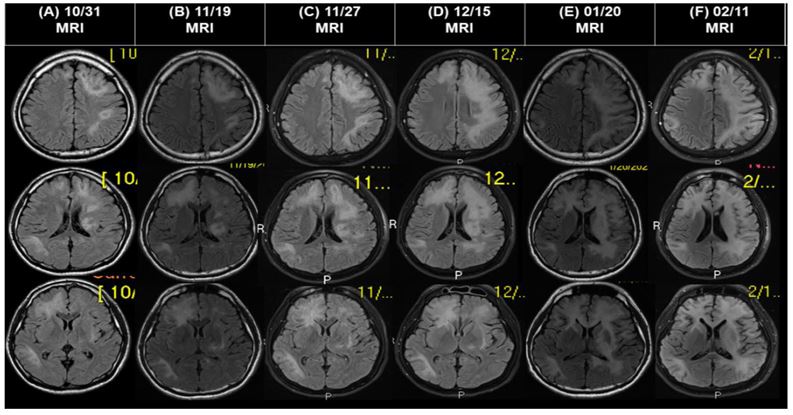
Figure 1: MRI images for patient DC. (A) MRI done last 10/31/2019 showing T2-FLAIR hyperintensities in the right frontal lobe, splenium and subcortical U-fibers, (B) MRI done last 11/19/2019 and (C) 11/27/2019 showing interval progression of confluent T2/FLAIR hyperintensities in both fronto-parietal and right temporal lobes involving the subcortical U fibers. (D) MRI done last 12/15/2019 showing stable but more confluent T2/FLAIR hyperintensities in the bilateral frontoparietal lobes and right temporal lobes. (E) MRI done last 01/20/2020 showing progression in the extent and degree of confluence of the white matter lesions in the bilateral frontoparietal and right temporal lobes. (F)
MRI done 02/11/2020 showing further confluence of T2/FLAIR hyperintensities over the left posterior parietal lobe.
PML-IRIS develops between 1 week and 26 months after initiation ART. The only identified risk factor for IRIS is a baseline CD4 cell count of < 50 cells. IRIS can unmask PML or it can paradoxically worsen a preexisting PML. Patients with pre-existing PML are observed to develop IRIS earlier with higher lesion loads on MRI and higher mortality compared with those who did not start ART. On MRI, contrast enhancement is absent in PML but it serves as a surrogate marker for IRIS since it is suggestive of development of an inflammatory response with breakdown of the bloodbrain barrier. However, this can be negative in 44% of cases of PML-MRI [6]. In our patient’s case, he was treated as PML-IRIS on the 3rd week after initiation ART and lesions seen on MRI did not show contrast enhancement.
Management of patients with PML-IRIS include use of corticosteroids and maraviroc, but evidence remains anecdotal and clinical trials are lacking [2,6]. Corticosteroids decreases the inflammation but it can also increase the reservoir of HIV-infected cells and thereby decrease JC virus clearance. Patients who have been previously given intravenous dexamethasone (32 mg daily given in four divided doses) and intravenous methylprednisolone (1g daily for five days) followed by tapering doses without interruption of ART have shown no difference in survival despite clinical responses observed in patients [6]. Maraviroc is a chemokine receptor inhibitor which is suggested to reduce the severity of neuroinflammation by targeting CCR leukocyte recruitment to the CNS. In several cases of patients with PML, the addition of maraviroc was associated with clinical improvement but no benefit was found in other cases. It was also not effective for IRIS after initiation ART. Therefore, because of the absence of randomized clinical trials, no recommendations have been made on the use of corticosteroids and/or maraviroc in the management of PML-IRIS [7,8]. In our patient’s third admission, intravenous Dexamethasone for 5 days was started and shifted to tapering doses of oral prednisone. Mefloquine was started, Mirtazipine and ART was continued. However, prior to the discontinuation of oral steroids, due to progression of neurologic symptoms and increased lesion burden on MRI, intravenous immunologlobulin was given for 3 days during the patient’s fourth admission and doses of oral prednisone were adjusted. Antiepileptics were added. No further deterioration of neurologic status was noted.
PML has the worst prognosis of any AIDS-related cerebral disorder. Survival of patients has improved markedly due to widespread use of ART with 1-year survival of patients PML increased from 10 to 50% with ART. Medial survival was reported to be more than 16 months with ART compared to 6 months if ART was not initiated. Survival is also correlated with reduced JC viral load in the CSF and improved CD4 lymphocyte counts (>100 cells/mm3). Several retrospective observational studies have demonstrated the absence of any significant difference in survival between PML with and without IRIS. These studies suggest that the outcome of PML is not worsened by IRIS which emphasizes the protective immune response that is instrumental in the long-term control of JC virus replication [9,10].
Conclusion
We present the case of a 36-year old Filipino male known to have HIV-PML and treated as a case of PMLIRIS. Because of its low incidence, there exists no consensus guideline on the management of patients with HIV and PML-IRIS. Despite the difficulties encountered in the management of patients with PMLIRIS, the use of intravenous corticosteroids has shown efficacy and should be considered as a therapeutic option.
References
- Berger J. The clinical features of PML. Cleveland Clinic Journal of Medicine. 2011; 78: S8-S12.
- Fournier A. IRIS: Unmasking or Worsening AIDSRelated PML: A Literature Review. Front Immunol. 2017; 8: 577.
- Engsing FN, et al. Incidence, clinical presentation,and outcome of PML in HIV-infected patients during the HAART era: a nationwide cohort study. J Infect Dis. 2009; 199(1): 77.
- Berger JR, Aksamit AJ, Clifford DB, et al. PML diagnostic criteria: consensus statement from the AAN Neuroinfectious Disease Section. Neurology. 2013; 80: 1430.
- Adcock J, et al. Progressive multifocal leukoencephalopathy: A retrospective study of 30 cases. J. Clin. Neurosci. 197; 4: 463-468.
- Tan K, et al. PML-IRIS in patients with HIV infection: clinical manifestations and treatment with steroids. Neurology. 2009; 72(17): 1458-64.
- Sierra-Madero JG, Ellenberg SS, Rassool MS, Tierney A, Belaunzaran-Zamudio PF, Lopez-Martinez A, et al. Effect of the CCR5 antagonist maraviroc on the occurrence of immune reconstitution inflammatory syndrome in HIV (CADIRIS): a double-blind, randomised, placebocontrolled trial. The Lancet HIV. 2014; 1(2): 60-67.
- Middel A, Arends JE, Van Lelyveld SF, Otto S, Schuurman R, et al. Clinical and immunologic effects of maraviroc in progressive multifocal leukoencephalopathy. Neurology. 2015; 85(1): 104-106.
- De Luca, et al. The effect of potent ART and JC virus load in CSF on clinical outcome of patients with AIDSassociated PML. J Infect Dis. 2000; 182: 1077-1083.
- Berenguer J, et al. Clinical course and prognostic factors of PML in patients treated with highly active antiretroviral therapy. Clin Infect Dis. 2003; 36: 1047-1052.

