Case report - Volume 3 - Issue 3
Surgical Management of Craniocervical Junction Tuberculosis: report of two cases
Amin Md Rezaul1*; Rahman Md Tauhidur2; Hossain ABM Manwar2; Quader Tahsina3; Islam KM Tarikul4
1Associate Professor, Department of Spinal Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
2Resident, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University.
3Consultant, OGSB Hospital, Bangladesh.
4Associate Professor, Department of Neurosurgery, BSM Medical University, Bangladesh.
Received Date : May 04, 2023
Accepted Date : June 09, 2023
Published Date: June 16, 2023
Copyright:© Rezaul Amin 2023
*Corresponding Author : Rezaul Amin, Associate Professor, Spinal Neurosurgery Department, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
Email: rezaul_amin@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1462
Abstract
Background: CVJ tuberculosis is a rare entity that requires urgent management. Symptoms and signs may vary such as mild neck pain, torticollis, and partial to complete paralysis of all four limbs. Timely tissue diagnosis, immobilization of neck, decompression of CVJ and stabilization are the mainstay in the management of TB in this area.
Case Description: Two patients with CVJ tuberculosis are reported in this paper. Both had painful neck movement, progressive weakness of all 4 limbs and complete paralysis in the second patient. Detailed investigations including blood profile, X-ray cervical spine, CT scan and MRI of cervical spine with contrast were done and described accordingly. The diagnosis was confirmed by tissue sample obtained during surgery. Both patients were managed by surgical intervention, antitubercular drugs and showed clinical and radiological recovery.
Conclusion: Early diagnosis, proper instrumentation and appropriate dosages of anti TB drugs are the keys in the management of CVJ TB.
Key Word: Craniovertebral junction. Tuberculosis, Torticolis, Kyphotic Deformity, Anti-tubercular therapy
Abbreviations:
CVJ: Craniovertebral Junction
TB: Tuberculosis
CSF: Cerebrospinal fluid
Introduction
The incidence of tuberculosis (TB) in spine is <1% [1]. Isolated involvement of the craniovertebral junction (CVJ) comprising the atlas, axis, and basiocciput is even rarer. Tuberculosis in this area is a rare clinical entity and involves 0.3% to 1% of spondylodiscitis [2,3].There is scarce information on CVJ tuberculosis even in developing countries. While this infection mainly involves the atlas and the axis, it can also involve the lower end of the clivus and occipital condyles. The CVJ is the most mobile segment of the cervical spine and extensive osteocartilaginous destruction can lead to atlantoaxial instability. Besides, epidural abscess or granulation tissue may compress cervicomedullary cord and produces quadriplegia, bulbar dysfunction, respiratory suppression, and even death. To prevent long term neurological deficit early diagnosis and treatment are essential. Anti-tubercular therapy, decompression of neural elements and stabilization all plays critical role in the management of CVJ TB [3-6].
Case: 1
History and presentation
A 16-year female presented with severe neck pain during movement for one month, low grade fever and progressive weakness of all four limbs for two weeks. She did not give any history of bladder-bowel involvement.
Physical examination
She had local tenderness in upper cervical region, spastic quadriparesis, muscle power MRC 4, all jerks were exaggerated and planter extensor, sensory modalities were diminished from C2, 3, 4 dermatomes. There was no palpable lymphadenopathy.
Investigations
X-ray cervical spine and CT cervical spine showed osteolytic lesion at C2 body with local kyphosis. In CT CVJ with cervical spine showing lateral mass of C1 was well delineated and C2 pedicle and body was destructed by the lesion. MRI showed an extradural mass in front of C1/2 Level causing obliteration of anterior CSF column and kinking of spinal cord at CVJ with extension into retropharyngeal space. Regarding blood picture her ESR was 90 mm in 1st hr and CRP was 65. Chest X-ray was normal. The Tuberculin test was not positive.
Operation procedure
As the lesion extend into the retropharyngeal space and causing destruction of C2 vertebral body we decided to go two staged surgery. In first stage, transoral decompression with tissue diagnosis was confirmed. And in second stage, we went through posterior stabilization. In the transoral procedure, the patient was kept in supine position with neck extension. Retraction of oral cavity and tongue were done by Dingdong retractor. Under microscopic guidance, we made incision in the upper part of anterior pharyngeal wall and pus was coming out through the incision. We did surgical toileting and there was granulation tissue noted over the C2 body. Biopsy was taken and pus was collected for Culture and Gram’s and AFB staining. Wound was closed in layers. After 5 days biopsy result confirmed the lesion was caseating granulomatous inflammation and AFB staining was for TB.
After confirming the diagnosis, we planned to do the second stage surgery. Patient was positioned in prone with tong traction. After dissection of the muscle C1,C2,C3 and C4 were identified clinically and radiologically. C1, C2 lateral zygapophyseal joints were destructed, and bony chips harvested from iliac crest were impacted in that joint. C1 lateral mass screw (28mm in length and 4mm in diameter) and C3, C4 lateral mass screws (14mm in length and 4mm in diameter) were inserted. Wound was closed in layers.

Figure 1: (A) X-ray cervical spine lateral view showing increase atlanto dental interval (16mm) with radio dense shadow in between, CT cervical spine lateral (B), cornal (C) view showing osteolytic lesion at C2 body, MRI cervical spine in sagittal T2WI (D) and T1WI (E) showing prevertebral retro-oropharyngeal abscess. Post-operative cervical X-ray (F+G) after 15 days, CT cervical spine sagittal (H) after one month and MRI of cervical spine in sagittal T2WI (I) after 3 months showed complete resolution of abscess, correction of kyphotic deformity, patient picture after 15 days (J) and 3 months (K).
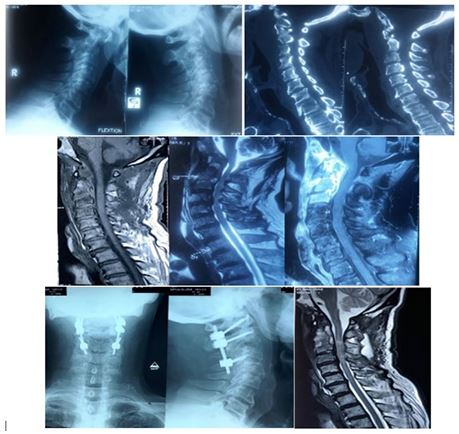
Figure 2: X-ray cervical spine dynamic view (A) showing C1/2 instability, CT cervical spine in sagittal view (B) showing partial erosion of C1 lateral mass and C2 body, MRI of cervical spine (C,D,E) contrast enhancing extradural mass at C1-3 level causing obliteration of anterior CSF column and prevertebral collection of abscess. Post operative X-ray of cervical spine at one month (F) showing spinal fixation between C1 lateral mass, C2 pedicle and C3 lateral mass with screws and rods, MRI of cervical spine at 6 month complete resolution of abscess and significant decompression of cord (G).

Postoperative Course
The immediate post-operative period was uneventful. Neck pain subsided gradually, limb spasticity reduced within 15 days and muscle power was improved within 10 days after operation. Histopathology and gene xpert were suggestive of granulomatous lesion by mycobacterium tuberculosis. Total 18 months of anti-tubercular therapy was given as 3 months of 4 drugs intensive course followed by 15 months of 2 drugs continuous. She was advised to use rigid cervical collar for one month and then soft collar for another 2 months. Tablet pyridoxine was also advised during antitubercular therapy.
Follow up
X-ray was done immediately after operation, after 7 days, 15 days, one month and 3 months interval. CT scan was done after 15 days, and MRI was done after one month of the operation. Her CBC and CRP were done after 7 days of the operation and monthly after the operation for first 3 months. Then her CBC, CRP and X-ray cervical spine were done in every 3 months. Another MRI was done after one year of the operation. Her blood picture returns to normal level within 3 months of operation. Her power became normal after one month of the operation. No antitubercular drugs related complications were developed.
Case:2
History and presentation
A 68-year male presented with severe neck pain and quadriplegia with bladder-bowel involvement. He had respiratory distress during the admission. We gave immediate skeletal (tong) traction. After traction his respiratory pattern was improved, and his power became MRC grade 2.
Physical examination
During the admission his power was MRC grade 0 and urinary catheter was given at that time due to retention of urine. Sensory was diminished below C2 level and all jerks were exaggerated, Hoffmans’ was positive, and planter was extensor, patellar clonus was absent, but ankle clonus was present. Local examination of spine was noted tender. No gibbus was seen.
Investigations
X-ray cervical spine dynamic view showed atlanto-axial instability, posterior interspinous space was increased during flexion which indicates reducible variety of AAD and CT cervical spine showed destruction of C2 dense without any local kyphosis. MRI showed involvement of C2, 3 intervertebral disc, vertebral body with extradural mass in front of C1 to C3 Level causing obstruction of CSF column along with collections in retropharyngeal space.
Operation procedure
After 2 days of skeletal (tong) traction patient underwent surgery. He was positioned in prone with tong traction to keep the neck in anatomical position. During the opening of C1/2 lateral joint space pus was coming out from anteriorly. Granulation tissue was found alongside the lateral mass of C1,C2 which was debrided. Pus was drained with proper irrigation. C1 lateral mass screw (28mm in length and 4mm in diameter), C2 pedicle screw (26mm in length and 4mm in diameter) and C3 lateral mass screws (14mm in length and 4mm in diameter) were inserted. The wound was closed in layers after proper hemostasis.
Postoperative Course
The immediate post-operative period was uneventful. After 2 days of operation muscle power became MRC grade 3 and after15 days he could walk with support. Histopathology was suggestive of caseating granulomatous lesion and gene xpert confirm TB.
Total 18 months of anti-tubercular therapy was given as 3 months of 4 drugs intensive course followed by 15 months of 2 drugs continuous. She was advised to use rigid cervical collar for one month and then soft collar for another 2 months. Tablet pyridoxine was also advised during antitubercular therapy.
He was followed as in the previous case. His CBC, CRP returned to normal limit after 2 months. At 3 months he could walk independently. No antitubercular drug related complication was observed.
Discussion
The CVJ TB is rare entity. Cervical spine involvement among spinal tuberculosis is 3% to 5% [7]. Any disease in this area may cause secondary instability and severe neuroaxis compression. This may manifest as painful torticollis, dysphagia and quadriparesis [1,8]. So, early diagnosis is a crucial part in managing such disease. Neurological deficits are more likely with the involvement of ligaments and the bone. The deficits may be due to mechanical compression of neural structures (cranial nerves and spinomedullary junction) from tubercular abscess, granulation tissue, dislocation of the atlantoaxial joint, or basilar invagination. Sometimes vascular compromise due to endarteritis resulting from associated local meningitis may complicate the neurological picture. During our daily practice we also encountered with CVJ tuberculosis less frequently. Most authors recommend CT-scan and/or MRI for the craniovertebral junction as initial tools for diagnosis followed by the histology and bacteriology of the specimen gained usually through transoral biopsy of the retropharyngeal abscess for the confirmation [9,10]. While others suggest open posterior biopsy and decompression through the C2 pedicle [11]. After physical assessment X-ray cervical spine dynamic view, CT cervical spine in bone window with CT angiogram and MRI of cervical spine with contrast are the usual tools for radiological evaluation for both diagnostic and treatment purpose. Image guided needle biopsy usually not done as most patient attend the physician with Literature is quite divided on management protocol in patients with tuberculosis in CVJ [2,3,9,11,12]. Some authors recommend conservative treatment only [1,8,13], while others recommend surgery [4,14,15].
We report two cases of CVJ TB, which we did early management with confirmation of the diagnosis by tissue biopsy and gene xpert. In both cases we decompress the neuroaxis and stabilize with proper instruments. We gave 18 months anti TB drugs, where first 3 months of 4 drugs regimen and 15 months of 2 drugs regimen. We found improvement of the patients was satisfactory
Conclusion
Though TB in CVJ is a dangerous disease by location, with prompt histological diagnosis with appropriate medical and surgical treatment, the prognosis is good. Early surgical intervention to overcome the neurological deterioration with proper instrumentation and proper anti TB therapy are keys for the management of CVJ TB.
Declarations
Authors Contributions:
Conception, Diagnosis and Design, Radiological Diagnosis and Final approval of manuscript:
Dr. Md. Rezaul Amin, Dr. Md. Tauhidur Rahman, Dr ABM Manwar Hossain, Dr. Tahsina Quader , Dr. KM Tarikul Islam
Manuscript Preparation, Technical Revision, and Manuscript editing and revision:
Dr. Md. Rezaul Amin, Dr. Md. Tauhidur Rahman
Literature Review: Dr. Md. Rezaul Amin, Dr. Md. Tauhidur Rahman
References
- Arora S, Sabat D, Maini L, Sural S, Kumar V, Gautam VK, Gupta A, Dhal A. The results of nonoperative treatment of craniovertebral junction tuberculosis: a review of twenty-six cases. JBJS. 2011; 93(6): 540-7.
- Gupta SK, Mohindra S, Sharma BS, Gupta R, Chhabra R, Mukherjee KK, Tewari MK, Pathak A, Khandelwal N, Suresh NM, Khosla VK. Tuberculosis of the craniovertebral junction: is surgery necessary?. Neurosurgery. 2006; 58(6): 1144-50.
- Behari S, Nayak SR, Bhargava V, Banerji D, Chhabra DK, Jain VK. Craniocervical Tuberculosis: Protocol of Surgical Management: In Reply. Neurosurgery. 2003; 53(4): 1010.
- Arunkumar MJ, Rajshekher V. Outcome in neurologically impaired patients with craniovertebral junction tuberculosis: results of combined anteroposterior surgery. J Neurosurg 2002; 97(spine 2): 166 - 71.
- Edwards RJ, David KM, Crockard HA. Management of tuberculomas of craniovertebral junction. Br J Neurosurg 2000; 14: 19- 22.
- Shukla D, Mongia S, Devi BI, Chandramouli BA, Das BS. Management of craniovertebral junction tuberculosis. Surgical neurology. 2005; 63(2): 101-6.
- Mohindra S, Gupta SK, Mohindra S, Gupta R. Unusual presentations of craniovertebral junction tuberculosis: a report of 2 cases and literature review. Surgical neurology. 2006; 66(1): 94-9.
- Akhaddar A, Chakir N, El Hassani MY, El Quessar A, Jiddane M, Boukhrissi N. Sub-occipital Pott's disease. Diagnostic imaging in 2 cases. Journal of Neuroradiology= Journal de Neuroradiologie. 2000; 27(2): 144-9.
- Allali N, El-Quessar A, Melhaoui A, El-Hassani MR, Chakir N, Jiddane M. Sub occipital Pott's disease: report of 8 cases. Journal of Neuroradiology= Journal de Neuroradiologie. 2004; 31(1): 72-3.
- Augier A, Zrig H, Roqueplan F, Brauner M, Dumas JL. MR and CT features of craniocervical junction tuberculosis: a report of 5 cases. Journal de Radiologie. 2008; 89(5 Pt 1): 585-9.
- Belanger E, Levi AD. Tuberculosis of the axis in a patient with systemic sarcoidosis: technique of posterior open biopsy of the dens: case report. Neurosurgery. 2000; 47(4): 969-72.
- Dhaon BK, Jaiswal A, Nigam V, Jain V. Atlantoaxial rotatory fixation secondary to tuberculosis of occiput: a case report. Spine. 2003; 28(11): E203-5.
- Shukla D, Mongia S, Devi BI, Chandramouli BA, Das BS. Management of craniovertebral junction tuberculosis. Surgical neurology. 2005; 63(2): 101-6.
- Bapat MR, Lahiri VJ, Harshavardhan NS, Metkar US, Chaudhary KC. Role of transarticular screw fixation in tuberculous atlanto-axial instability. European Spine Journal. 2007; 16: 187-97.
- Sinha S, Singh AK, Gupta V, Singh D, Takayasu M, Yoshida J. Surgical management and outcome of tuberculous atlantoaxial dislocation: a 15-year experience. Neurosurgery. 2003; 52(2): 331-9.

