Research Article - Volume 3 - Issue 3
Emphysematous pyelonephritis: Case series
Atanu Pal*1,Anirban Sen2, Saugat Dasgupta3, Koushik Bhattacharjee1, Sanjoy Dasgupta4
1Assistant Professor, Department of Nephrology, Institute of Post Graduate Medical Education and Research, Kolkata, India.
2Post Doctoral Trainee, Department of Nephrology, Institute of Post Graduate Medical Education and Research, Kolkata, India.
3Senior Resident, Department of Nephrology, Institute of Post Graduate Medical Education and Research, Kolkata, India.
4Professor, Department of Nephrology, Institute of Post Graduate Medical Education and Research, Kolkata, India.
Received Date : May 09, 2023
Accepted Date : June 15, 2023
Published Date: June 22, 2023
Copyright:© Atanu Pal 2023
*Corresponding Author : Dr Atanu Pal, Assistant Professor, Department of Nephrology, Department of Nephrology, Institute of Post Graduate Medical Education and Research, Kolkata, India, 700020.
Email: projectdratanu@gmail.com
DOI: Doi.org/10.55920/2771-019X/1466
Abstract
Backgroundː EPN is a rare and severe necrotizing infection of the kidney and its surroundings which is characterized by intraparenchymal gas, seen mostly in diabetics, and critically ill patients and has a high mortality if early therapy is not initiated.
Methodsː This was an observational study conducted at IPGME&R, SSKM hospital between December 2020 and August 2022. 15 patients were selected and followed up.
Resultsː the most common clinical finding in our study population were fever and nausea-vomiting, while raised HbA1C, leucocytosis and pyuria were the most common laboratory finding. E. Coli was the most common organism detected from urine and blood culture both. Majority of the patients were EPN stage 1 and 2. 47% of the patients were treated successfully using antibiotics alone.
Conclusionsː Although EPN is a life threatening disease, prompt detection and early initiation of antibiotic therapy can salvage most patients successfully.
Keywords: Emphysematous pyelonephritis, uncontrolled diabetes, urological interventions
Introduction
EPN is a rare and severe necrotizing infection of the kidney and its surroundings which is characterized by intraparenchymal gas [1]. Most of the cases are reported in diabetics, about 90% reported according to different series; obstructive uropathy is the other contributing factor in other cases. Patients are usually critically ill, with a high mortality rate ranging from 18% to 90% according to various case series. Escherichia coli is the most common causative pathogen isolated on urine or pus culture in nearly 70% of the reported cases [2]. In addition, Klebsiella, Clostridium, Candida, Aspergillus, Cryptococcus, and Amoeba also has been reported from the culture. EPN is more prevalent in women, and in diabetic populations. Other susceptible groups include patients with renal calculi, structural abnormalities of the urinary tract, and impaired immune regulation. Although a high tissue glucose level could provide a favorable environment for the growth of gas-producing bacteria in patients with diabetes, this was not associated with increased mortality or need for the dialysis, even in patients with poorly controlled diabetes mellitus (glycosylated hemoglobin [HbA1c] >8%) [3].
The important factors implicated in the pathogenesis of EPN are presence of gas-forming bacteria, a high tissue glucose level, impaired tissue perfusion, a defective immune response due to an impaired vascular supply, and Ureteral obstruction causes local tissue ischemia that provokes infection. Poorly controlled diabetes leads to high tissue level glucose, impaired oxygen delivery due to diabetic vasculopathy and nephropathy, altered immune response and functional statis due to autonomic neuropathy. Thus, it contributes in all the pathogenic factors and causes rapid growth of gas forming bacteria and ultimately tissue ischaemia and necrosis. Presence of Calculi act as a nidus for infection, and also causes stagnation and reflux of urine [4].
Earlier the diagnosis of EPN was difficult due to absence of any specific signs and symptoms and non-detection of intraparenchymal gas by ultrasound in the early stages. Poor response to antibiotic treatment in patients with diabetes mellitus or rapid worsening of clinical condition in patients of acute pyelonephritis should immediately arouse suspicion of this life-threatening infection. With the more widespread use of CT scan and introduction of CT based criteria of diagnosing EPN by Huang and Tseng et al, more cases of EPN are being diagnosed now in the early stages, thus improving their outcome [5].
The treatment of EPN has changed over the years from radical nephrectomy to more conservative approaches, such as antibiotics and percutaneous drainage techniques, due to the availability of better imaging modalities and early detection
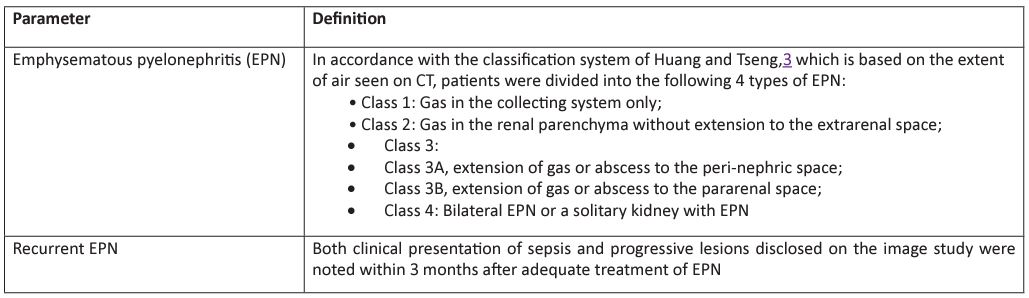
Table 1: Definitions.
Materials and methods
This was an observational study conducted at IPGME&R, SSKM hospital between December 2020 and August 2022. All patients who were admitted to the Department of Nephrology for management of EPN were chosen for the study after fulfilling the study criteria. We collected various variables from our chosen subjects that were suspected to have any effect on clinical outcomes, based on our knowledge of similar studies. We collected demographic characteristics and clinical information, underlying medical conditions, laboratory findings, imaging findings, types of management, and patient outcomes. The clinical features included signs and symptoms at presentation, and the hemodynamic and mental status of the patients. The laboratory variables included hemoglobin, white blood cell count, platelet count, albumin, sodium, HbA1c, serum creatinine levels, serum electrolytes, and the results of urinalysis, blood, and urine cultures.
Results
We followed up 15 patients who had a diagnosis of EPN. We divided the entire cohort of our patients into 2 broad categories; 1 group of patients was managed conservatively without any need for hemodialysis or any urological procedure, and the other group required hemodialysis and/or urological intervention along with other standard medical treatment for EPN. Overall, 7 patients in were managed conservatively, and 8 patient required hemodialysis/urological intervention. The age of patient in the dialysis group was higher than those in the conservative group (60 years vs. 45 ± 10 years); Depressed level of consciousness, shock, thrombocytopenia, and hypoalbuminemia all had a numerically higher incidence among the hemodialysis group of our study population, although these failed to achieve statistical significance. Mean serum creatinine was higher and statistically significant in the hemodialysis group (6.1 mg/dl) versus the conservatively managed group (2.5 mg/dl). The overall prevalence of diabetes in our study was 100%, with a median duration of 10 years (range: 4 yrs to 10 years).
The clinical symptoms observed in our cohort is described in Table 2. The 2 most common symptoms reported in the overall cohort of our study were fever (100%), and nausea, vomiting (100%). Other frequently reported symptoms were frequency of micturition, oliguria, generalized weakness. Thrombocytopenia (53%) and shock (27%) were considered to be features of a more severe form of the disease. One patient in our cohort had carcinoma urinary bladder. None of the patients were on immunosuppressive therapy that could predispose them to infection. Two patients had recurrent pyelonephritis.
The most common organism to be cultured from urine was Escherichia coli (40%). The other organisms included Klebsiella pneumoniae: Urine culture was negative in 53% of patients (Table 3). Bacteremia occurred in 7 patients (47%), with E. Coli in 3 patients and Enterococcus in 2 patients, Staphylococcus and Klebsiella in 1 patient each (Table 4).
Radiological findings showed that 33% of our patients had EPN stage 1 and 2 each. 47% of the patients had left sided, 40% had right sided, and 13% had bilateral lesion. 2 out of 15 patients had features of urinary tract obstruction, and 1 patient had renal calculus (Table 5).
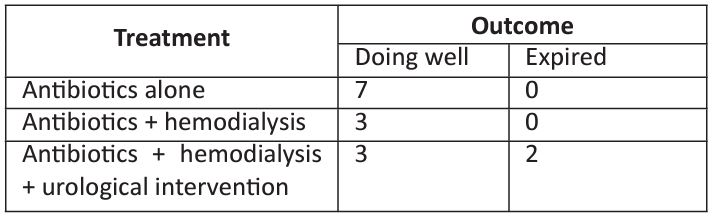
All the patients in our study were started on antibiotics intravenous meropenem and oral levofloxacin as per institutional antibiotic protocol. Antibiotic at admission were later modified depending upon the culture sensitivity report and clinical condition of the patient (worsening of symptoms, shock, dialysis requirement). Blood and urine cultures were taken before initiating antimicrobials for all our patients. We observed that antibiotics alone were successful in treating EPN in 7 out of 15 patients (47%). Urological interventions were needed in 5(33%) patients - in one patient bilateral DJ stenting was done while in 4 other patients unilateral DJ stenting with pig tail insertion were performed (Table 6). Two patients were planned for nephrectomy but could not be done due to poor general condition (shock with thrombocytopenia) and they expired, while two patients improved and did not require nephrectomy.
Table 1: Clinical and laboratory parameters of the patients.
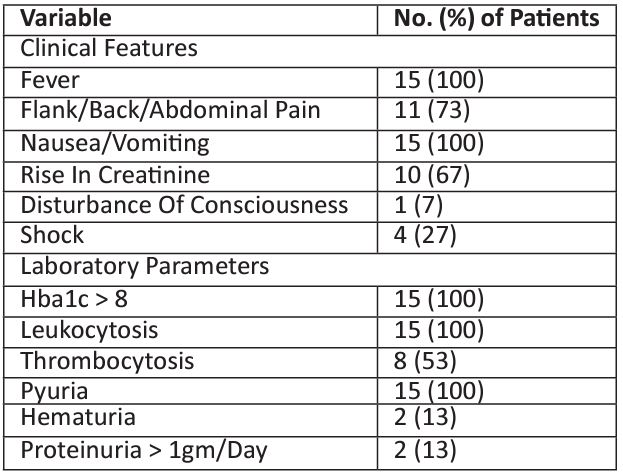
Table 2: Types Of Organism From Urine Culture.
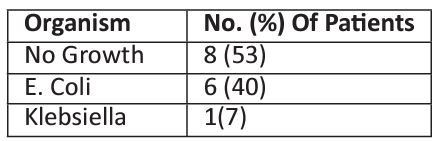
Table 3: Types of organism from blood culture.
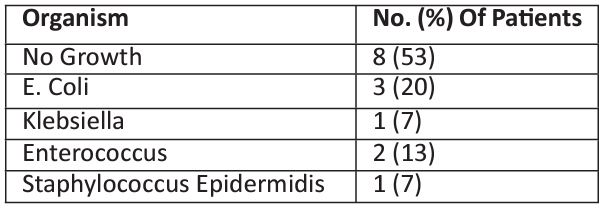
Table 4: Radiological findings in the patients.
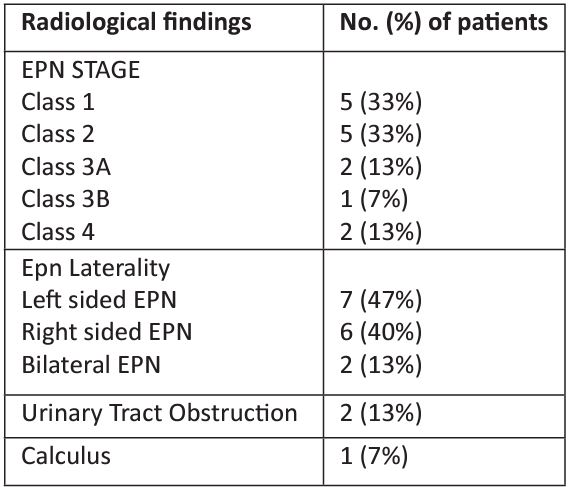
Table 5: Summary of treatment and outcome in the patients.
Discussion
EPN is a rare, life-threatening necrotizing infection of the renal parenchyma that is characterized by an accumulation of gas in the renal parenchyma, peri-renal tissues, and/or in the collecting system.
Previous studies have showed that EPN is a disease that occurs more commonly in women. In most of the studies there was female predominance and the female to male ratio varied from 12:1 to 1.3: 1 [4,6,7]. In our study the female to male ratio was 1.5: 1. The female predominance is attributed to increased susceptibility of females to urinary tract infection due to their short length of urethra, proximity of urethral orifice to anus, absence of prostate and poor hygiene.
The major risk factors of EPN are uncontrolled diabetes mellitus, renal calculi disease, structural abnormalities of the urinary tract (unilateral or bilateral), and impaired host immune mechanisms. In their study, Huang and Tseng reported that 96% of the patients had diabetes mellitus, and 22% had urinary tract obstruction [5]. Similarly prevalence of diabetes and renal calculi was 98% and 7.84%, respectively in the study by Eswarappa et al [4]. In our study, the prevalence of diabetes, renal calculi and urinary tract obstruction was 100%, 8% and 15% respectively. Lu et al proposed that high tissue glucose levels could cause a fulminant course in patients with diabetes mellitus, because such high levels might provide gas-forming microbes in a microenvironment that is more favorable for growth and catabolism, however this had no prognostic significance and there was no corelation between increased HbA1C level and increased mortality [7]. In our study all the patients had poorly controlled diabetes (HbA1C > 8) and mortality was 15%.
In the study by Huang and Tseng fever (79%) and abdominal or back pain (71%) were the major presenting symptoms followed by, nausea and vomiting (17%), lethargy and confusion (19%), dyspnea (13%) [5]. 29% of patients presented with severe complications like shock. In another study by Eswarappa et al, abdominal pain (94.11%) was the most common symptom, followed by fever (82.3%), dysuria (74.5%), vomiting (72.54%), frequency of micturition (68.62%), oliguria (66.67%), generalized weakness (66.67%), and shortness of breath (49.01%) [4]. In our study, we found that the 2 most common symptoms reported in the overall cohort of our study were fever (100%), and nausea, vomiting (100%). Other frequently reported symptoms were frequency of micturition, oliguria, generalized weakness.
In their studies, Huang and Sheng, Eswarappa et al, Kapoor et al and Khaira et al, have shown thrombocytopenia, uremia, altered mental status and shock at presentation were poor prognostic features of EPN [3,4,5,8]. Hyperglycemia and elevated leucocyte count were also shown to be poor prognostic markers by the study of Olvera-Posada et al [9]. Lu et al. reported that need for emergency hemodialysis, severe hypoalbuminemia (serum albumin <3 g/dl), and polymicrobial infections were poor prognostic factors for patients with EPN [7]. In our study Thrombocytopenia, uremia and shock were present at initial presentation in 53%, 67% and 27% of the patients respectively, however any statistically significant corelation with outcome could be not be made.
In their studies, Huang and Tseng, Wan et al. and Pontin et al. showed that E coli was the most common causative organism for EPN, which was isolated in 47% to 90% of their patients; the other commonly involved organisms included P. mirabilis, Klebsiella, pneumoniae, Enterococcus species, and Pseudomonas aeruginosa [5,6,10]. In our study urine and blood culture was positive in 47% of the patients. E. Coli (40%) was the predominant organism identified in the cultures. In addition, klebsiella, staphylococcus epidermides and enterococcus were also found. No corelation was established between the type of organism and mortality.
Different studies have shown slightly higher prevalence of left sided EPN, from 50.9% to 67%, than right sided or bilateral EPN [1,4,5]. In our study, 47% of patients had left-sided EPN, 40% had right-sided EPN, while 13% had bilateral EPN. Also, according to CT grading of EPN, class 1 and class 2 (33% each) were most common type in our study. However, no statistically significant association between side or class of EPN and prognosis or mortality was established.
The recent years have witnessed a change in the approach of treatment of EPN. Earlier studies by Huang and Tseng, Dunn et al and Cook et al have shown nephrectomy as the main modality of treatment of EPN [5,11,12]. Prompt nephrectomy was associated with better outcome as compared to conservative medical management. However other studies done recently by Misgar et al., Nagappan and Kletchko, Grozel et al., and Tahir et al have shown successful conservative management of EPN with limited surgical intervention [13,14,15,16]. In our study 47% of the patients were treated by antibiotics alone, while 53% of the patients required dialysis support. 33% (5 out of 15) patients required urological intervention. Two of the four patients who underwent urological intervention, were planned for nephrectomy, but they succumbed prior to the procedure.
Conclusion
EPN is a serious renal necrotizing infection, causing rapid worsening of clinical condition in immunocompromised patients and in presence of urinary tract obstruction. Clinicians must be aware of this condition and EPN should be suspected in any patient with pyelonephritis who fail to improve or show clinical deterioration despite adequate antibiotic treatment. Early detection is the key to better outcome. Despite early diagnosis and prompt management, mortality is still high.
References
- Falagas ME, Alexiou VG, Giannopoulou KP. Siempos Risk factors for mortality in patients with emphysematous pyelonephritis: a metaanalysis. J Urol. 2007; 178: 880-885.
- Ubee SS, McGlynn L, Fordham M. Emphysematous pyelonephritis. BJU Int. 2011; 107(9): 1474-8.
- Khaira A, Gupta A, Rana DS, Gupta A, Bhalla A, Khullar D. Retrospective analysis of clinical profile prognostic factors and outcomes of 19 patients of emphysematous pyelonephritis. Int Urol Nephrol. 2009; 41: 959-966.
- Eswarappa M, Suryadevara S, John MM, Kumar M, Reddy SB, Suhail M. Emphysematous Pyelonephritis Case Series From South India. Kidney Int Rep. 2017; 3(4): 950-955.
- Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000; 160: 797-805
- Wan YL, Lo SK, Bullard MJ, Chang PL, Lee TY. Predictors of outcome in emphysematous pyelonephritis. J Urol. 1998; 159: 369373.
- Lu YC, Chiang BJ, Pong Y.H. Emphysematous pyelonephritis: clinical characteristics and prognostic factors. Int J Urol. 2014; 21: 277-282.
- Kapoor R, Muruganandham K, Gulia AK. Predictive factors for mortality and need for nephrectomy in patients with emphysematous pyelonephritis. BJU Int. 2010; 105: 986-989
- Olvera-Posada D, García-Mora A, Culebro-García C. Prognostic factors in emphysematous pyelonephritis. Actas Urol Esp. 2013; 37: 228-232.
- Pontin AR, Barnes RD, Joffe J, Kahn D. Emphysematous pyelonephritis in diabetic patients. Br J Urol. 1995; 75: 71-74
- Dunn SR, Dewolf WC, Gonzalez R. Emphysematous pyelonephritis: report of 3 cases treated by nephrectomy. J Urol. 1975; 114: 348-350.
- Cook DJ, Achong MR, Dobranowski J. Emphysematous pyelonephritis. Complicated urinary tract infection in diabetes. Diabetes Care. 1989; 12: 229-232.
- Misgar RA, Wani AI, Bashir MI. Successful medical management of severe bilateral emphysematous pyelonephritis: case studies. Clin Diabetes. 2015; 33: 76-79.
- Nagappan R, Kletchko S. Bilateral emphysematous pyelonephritis resolving to medical therapy. J Intern Med. 1992; 232: 77-80.
- Grozel F, Berthezène Y, Guérin C, Tran-Minh VA, Croisille M. Bilateral emphysematous pyelonephritis resolving to medical therapy: demonstration by US and CT. Eur Radiol. 1997; 7: 844-846.
- Tahir H, Thomas G, Sheerin N, Bettington H, Pattison JM, Goldsmith DJ. Successful medical treatment of acute bilateral emphysematous pyelonephritis. Am J Kidney Dis. 2000; 36: 12671270.

