Case Report - Volume 3 - Issue 3
Diffuse Large B-cell Lymphoma of the Broca Area presented as a Rare Cause of Progressive Cognitive Impairment in a Middle-Aged Woman uncovered with DTI, Fiber tracking and Spectroscopy: A Case Report
Walter M. Wallner*; Jochen Grimm; Johannes A. R. Pfaff
Department of Neuroradiology, Christian Doppler Medical Center, Paracelsus Medical University, Salzburg, Austria.
Received Date : May 09, 2023
Accepted Date : June 16, 2023
Published Date: June 23, 2023
Copyright:© Walter M. Wallner 2023
*Corresponding Author : Walter M. Wallner, Department of Neuroradiology, Christian Doppler Medical Center, Paracelsus Medical University, Ignaz-Harrer-Straße 79, A-5020 Salzburg, Austria.
Email: w.wallner@salk.at
DOI: Doi.org/10.55920/2771-019X/1467
Abstract
We present the case of a female patient in her 50s who presented with progressive language and cognitive impairments. The patient had a history of ocular vitreoretinal lymphoma, diagnosed three years prior to admission. Radiological investigations, including diffusion tensor imaging, fibertracking, dynamic contrast-enhanced MRI and spectroscopy were performed to establish a differential diagnosis for a relapsing lymphoma. CT and MRI scans revealed two cerebral lesions, and a stereotactic biopsy confirmed the diagnosis of diffuse large B-cell. Treatment with dexamethasone was initiated, resulting in a partial improvement of symptoms. Further management decisions were made in the oncology clinic and during a tumor board review.
Keywords: Diffusion tensor imaging; Fibertracking; Dynamic contrast-enhanced MRI; Spectroscopy; Ocular vitreoretinal lymphoma; Diffuse large B-cell lymphoma.
Abbreviations: DTI (diffusion tensor imaging), PCNSL (primary central nervous system lymphoma), DLBCL (diffuse large B-cell lymphoma), MRI (magnetic resonance imaging), CT (computed tomography), and SWI (susceptibility-weighted imaging). CNS (central nervous system), Dynamic Contrast-enhanced MRI (DCE-MRI), Diffusion Tensor Imaging (DTI), Magnetic Resonance Spectroscopy (MRS).
Introduction
Lymphomas are a group of hematologic malignancies that can involve various organs, including the brain. Primary central nervous system lymphoma (PCNSL) is a rare subtype of non-Hodgkin lymphoma that originates in the brain or spinal cord. PCNSL accounts for less than 5% of all primary brain tumors, and its diagnosis can be challenging due to its nonspecific symptoms and radiological findings. Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of PCNSL and has a poor prognosis [1]. The use of advanced imaging techniques, such as diffusion tensor imaging (DTI), fibertracking, dynamic contrast-enhanced MRI and spectroscopy can aid in the diagnosis and management of PCNSL [2].
Case Report
A female patient in her 50s presented to our neurology emergency department with slowly progressive language and cognitive impairments, including a moderate motor aphasia, semantic paraphasias, dysarthria, and psychomotor slowing. Neurological examination revealed a mild facial palsy on the right side, a discrete deviation of the tongue to the right, mild fine motor impairment of the right hand, and gait instability. The patient had a history of ocular vitreoretinal lymphoma, diagnosed three years ago, with no evidence of extracranial involvement on staging CT. A follow-up MRI one month after the staging-CT showed multiple cerebral lesions, but the patient declined further investigations or treatment at that time.
During investigation of the current neurological symptoms a non contrast-enhanced CT scan of the brain revealed two hyperdense intracerebral lesions with extensive perilesional edema in the left frontal lobe and right frontal/precentral region (Figure 1). A subsequent MRI showed lesions in the left frontal lobe, affecting the Broca's area and the corpus callosum, with midline shift, but without cerebrospinal fluid circulation impairment. Contrast enhanced cerebral MRI, DTI, fibertracking, dynamic contrast-enhanced MRI and spectroscopy were performed to establish a differential diagnosis for the cerebral lesions.
The main finding is a diffusion-restricted, sharply demarcated, strongly homogeneously enhancing lesion measuring approximately 38 x 27 mm in the left frontal subcortical white matter respectively Broca-Area, which serves as a reference lesion. There is an extensive perifocal edema zone shifting the midline structures approximately 4mm to the right, markedly impresses the left lateral ventricle, and affects the left basal ganglia (putamen, globus pallidus, and head of the caudate nucleus). Another lesion measuring approximately 13 x 15 mm with similar imaging characteristics is located in the corpus callosum, extending into the bilateral subcortical white matter, with moderate perifocal edema zone and midline crossing over the corpus callosum to the contralateral left side. There is highly suspicious striated contrast enhancement in the ventral aspect of the left frontal edema zone measuring approximately 19 mm. In the SWI (susceptibility-weighted imaging) sequence, there are discrete dot-like signal alterations in the ventrocranial aspect of the left frontal reference lesion, suggesting a discrete hemorrhage. Further striated SWI signal alterations are seen in the lateral aspect of the reference lesion, suggesting vascularization. The reference lesion as well as the midline-crossing lesion show strong, homogenous hyperperfusion. There is currently no evidence of cerebrospinal fluid circulation disorder. Spectroscopically, there is a choline as well as a lipid peak in the reference lesion and a cholin/creatin ratio of 5,62. There is DTI involvement of the left Broca's area. DTI revealed reduced fractional anisotropy and increased mean diffusivity in the lesion regions, consistent with disrupted white matter tracts. Fibertracking showed disrupted fibers in the lesion regions, consistent with the diagnosis of CNS-Lymphoma. (Figure 2-6).
A stereotactic biopsy performed afterwards confirmed the diagnosis of diffuse large B-cell lymphoma.
Treatment with dexamethasone, along with gastric protection and osteoporosis prophylaxis, was initiated, resulting in a partial improvement of the patient's symptoms. Electroencephalography revealed a moderate local functional impairment over the left fronto-temporal area, with occasional signs of increased cerebral excitability. The patient received regular logopedic therapy during her hospital stay. She was discharged in a stable and significantly improved condition, and further management decisions were made in the oncology clinic and during a tumor board review.
Discussion
The differential diagnosis of contrast enhancing cerebral mass lesions is broad and includes various primary and secondary neoplasms, infections, inflammatory and demyelinating diseases, and vascular lesions. The radiological features of PCNSL may vary depending on the location and extent of the lesions, but they typically present as homogenously contrast-enhancing lesions with surrounding edema. Tumour necrosis is not a common feature of CNS-lymphoma and was not noted in this case. The role of advanced imaging techniques such as diffusion tensor imaging, fibertracking, and spectroscopy in the diagnosis and management of PCNSL is not yet fully established, but these techniques may provide valuable information on the microstructural integrity, fiber orientation, and metabolic activity of the lesions [3].
Disorders or imaging changes that may resemble diffuse large B-cell lymphoma include glioblastoma, metastases or infections. One differential diagnosis to consider is glioblastoma, a highly malignant brain tumor that can also present with contrast-enhancing lesions on imaging. However, glioblastoma typically has a more infiltrative pattern and can involve multiple lobes of the brain. Furthermore, glioblastoma is commonly associated with necrotic tissue. Metastatic tumors to the brain, particularly from lung or breast cancer, can also mimic PCNSL on imaging. These tumors typically have a more irregular shape and may show calcifications or hemorrhage.
Infectious etiologies, such as toxoplasmosis or fungal infections, can also present with similar radiological features as PCNSL. However, these lesions may have a more ring-enhancing appearance and may be accompanied by clinical symptoms such as fever or headache.
Dynamic Contrast-enhanced MRI (DCE-MRI) is a type of magnetic resonance imaging that uses a contrast agent to evaluate the vascular properties of tissues. During a DCE-MRI scan, a contrast agent is injected into the patient's bloodstream, and rapid series of MRI images are acquired over time as the contrast agent moves through the vasculature and diffuses into the surrounding tissue. The resulting images can provide information about the blood flow and permeability of the tissue, which can be useful in the diagnosis and monitoring of certain types of cancer, as well as other vascular and inflammatory conditions. DCE-MRI is commonly used in oncology for assessing the response to treatment and monitoring disease progression [4].
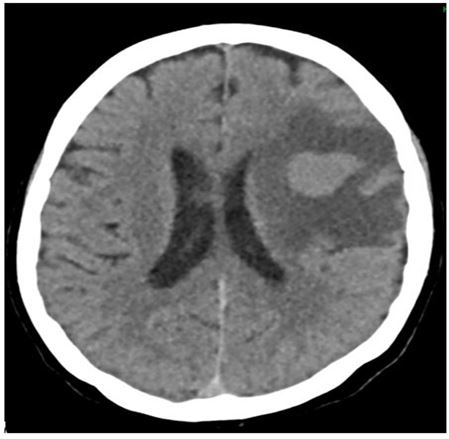
Figure 1: Hyperdense tumorous lesion on the frontal left with extensive perifocal edema.
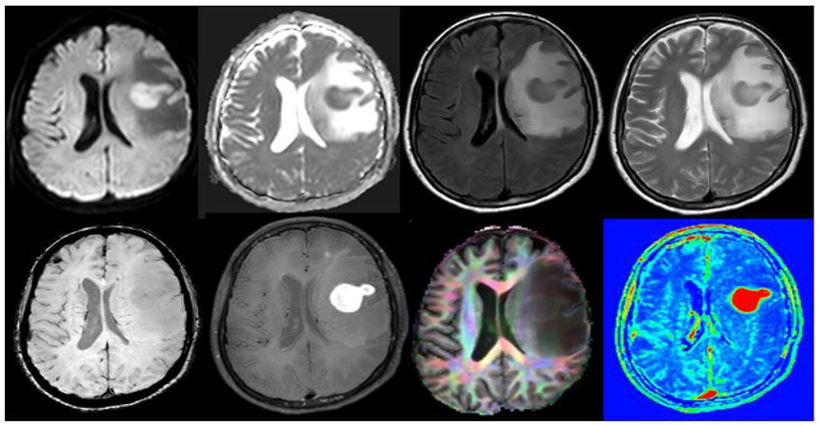
Figure 2: Diffusion-restricted, sharply demarcated, strongly homogeneously enhancing lesion in the left frontal subcortical white matter respectively Broca-Area. There is an extensive perifocal edema zone that shifts the midline structures approximately 4mm to the right. Rarification of the fibers can be clearly noted
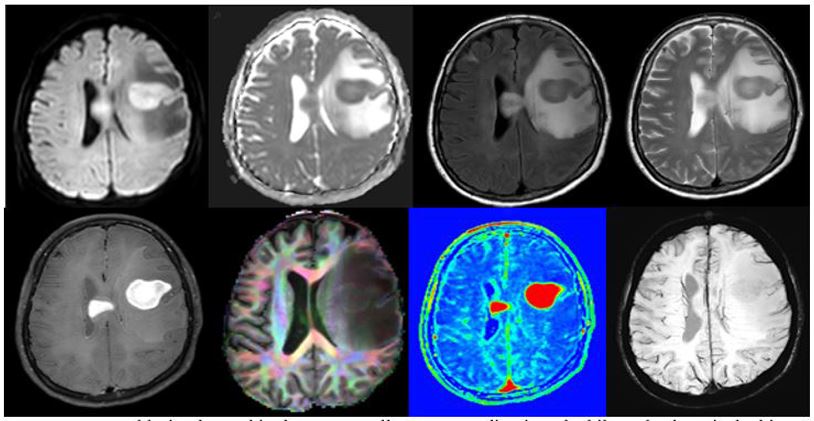
Figure 3: Second lesion located in the corpus callosum, extending into the bilateral subcortical white matter, with moderate perifocal edema zone and midline crossing via the corpus callosum to the contralateral left side. Rarification of the fibers can be clearly noted.
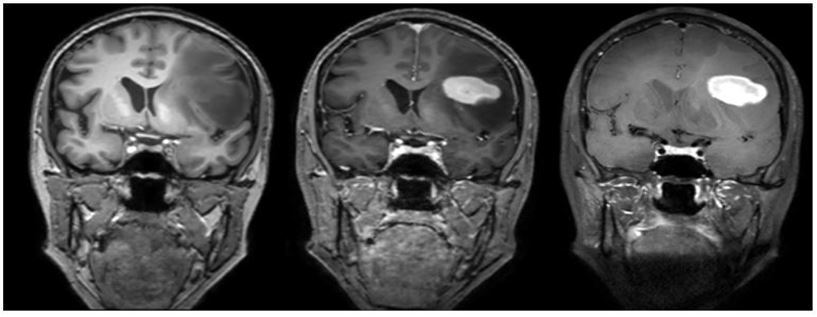
Figure 4: Coronal depiction of the lymphoma affecting the Broca-Area.
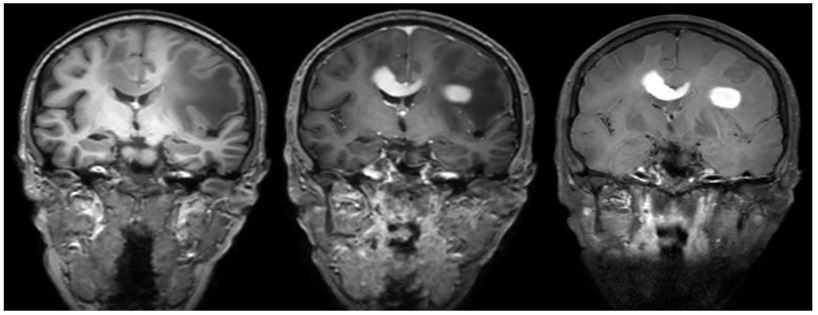
Figure 5: Coronal depiction of the second lymphoma lesion of the corpus callosum.
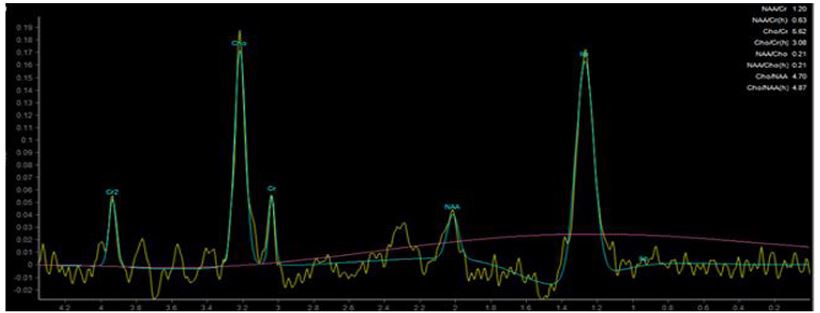
Figure 6: Spectroscopy showing high Cholin and Lipid peak.
Diffusion Tensor Imaging (DTI) is a magnetic resonance imaging (MRI) technique that allows for the visualization and quantification of the diffusion of water molecules in biological tissues. DTI is based on the principle that water molecules diffuse more easily along the direction of axonal fibers than perpendicular to them, due to the barriers created by the cell membranes. By measuring the direction and magnitude of this diffusion, DTI can provide information about the organization and integrity of white matter tracts in the brain.
DTI has been used to study a variety of neurological conditions, including stroke, traumatic brain injury, and neurodegenerative diseases. It has also shown promising results in the evaluation of brain tumors, including lymphomas. DTI can help differentiate lymphoma from other types of brain tumors by demonstrating disrupted white matter tracts in the affected area. In addition, DTI can provide valuable information about the extent and location of the tumor and help guide treatment planning.
Fractional anisotropy (FA) is a scalar value that is derived from Diffusion Tensor Imaging (DTI), a specialized MRI technique that is used to visualize the movement of water molecules in the brain. FA reflects the degree of directional preference of water diffusion within white matter tracts, where a value of 0 represents complete isotropy (random diffusion in all directions) and a value of 1 represents complete anisotropy (diffusion in a single direction). In general, FA is used as a measure of the microstructural integrity and organization of white matter, where higher FA values indicate greater structural coherence and integrity of the axonal fiber bundles. FA has been used in a wide range of clinical applications, including the diagnosis and monitoring of neurological disorders such as stroke, traumatic brain injury, and multiple sclerosis, as well as in research investigating the structural and functional connectivity of the brain [5].
Magnetic Resonance Spectroscopy (MRS) is a non-invasive imaging technique that provides information about the biochemical composition of tissues. MRS uses the same principles as MRI, but instead of imaging anatomy, it detects the chemical composition of tissues by measuring the signals emitted by specific chemical compounds, such as metabolites, neurotransmitters, and other molecules.
MRS can be useful in the diagnostic work-up of intracranial lymphoma, as it can provide information about the metabolic activity of the tumor, which can be different from that of normal brain tissue. For example, MRS can detect elevated levels of choline-containing compounds, which are often present in rapidly dividing cancer cells. Additionally, MRS can detect changes in the levels of other metabolites, such as N-acetyl aspartate (NAA) and lactate, which can also be indicative of tumor growth and metabolism [6,7].
Overall, MRS can provide valuable information about the biochemical composition of tissues, which can be used to complement other imaging modalities in the diagnosis and management of intracranial lymphoma.
Thus, the combination of the aspects described in this case report, diffuse large B-cell lymphoma remains the most probable diagnosis based only on advanced neuroimaging.
Conclusion
PCNSL and its subtype of DLBCL is a rare and challenging malignancy that requires a multidisciplinary approach for optimal diagnosis and treatment. Advanced neuroimaging techniques such as diffusion tensor imaging, fibertracking, and spectroscopy may provide valuable information on the microstructural integrity, fiber orientation, and metabolic activity of the lesions. Individualized therapeutic strategies are necessary to improve patient outcomes.
In conclusion, this case report highlights the importance of utilizing higher-level MR sequences in the diagnostic work-up of intracranial lymphoma. The initial CT imaging did not provide sufficient information to diagnose the patient's condition, while the subsequent MR imaging using advanced sequences such as Diffusion Tensor Imaging, Fibertracking, Dynamic Contrast-enhanced Perfusion and Spectroscopy, enabled a more accurate diagnosis. This enables clinicians to tailor the treatment plan and initiate appropriate therapy for the patient. These advanced MR techniques have shown great potential in improving the accuracy of diagnosis and treatment of intracranial lymphomas, particularly in cases where conventional imaging methods fail to provide sufficient information. Hence, incorporating advanced MR sequences in the diagnostic work-up can be considered a valuable tool for accurate diagnosis and management of intracranial lymphomas as demonstrated in this case.
Declarations
Conflict of interest: W. Wallner and J. Grimm declare that they have no competing interests. J. Pfaff reports personal fees from Boehringer Ingelheim AG & Co. KG, other from CERENOVUS (Johnson & Johnson Medical Products GmbH) outside the submitted work.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
Ethical standards: Informed consent was obtained from the patient for the publication of this case report and any accompanying data.
Availability of data and material: All data generated or analyzed during this study are included in this published article.
Author contributions: All authors contributed to this case report. Material preparation, data collection and analysis were performed by W. Wallner, J. Grimm and J. Pfaff. The first draft of the manuscript was written by W. Wallner and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- Sehn LH, Salles G. Diffuse Large B-Cell Lymphoma. N Engl J Med. 2021; 384(9): 842-58.
- Ly KI, Gerstner ER. The Role of Advanced Brain Tumor Imaging in the Care of Patients with Central Nervous System Malignancies. Curr Treat Options Oncol. 2018; 19(8): 40.
- Barkhof F, Jäger H, Thurnher M, Rovira À. Clinical Neuroradiology - The ESNR Textbook. 2019.
- Knopp MV, Giesel FL, Marcos H, von Tengg-Kobligk H, Choyke P. Dynamic contrast-enhanced magnetic resonance imaging in oncology. Top Magn Reson Imaging. 2001; 12(4): 301-8.
- Jones DK, Knosche TR, Turner R. White matter integrity, fiber count, and other fallacies: the do's and don'ts of diffusion MRI. Neuroimage. 2013; 73: 239-54.
- Govindaraju V, Young K, Maudsley AA. Proton NMR chemical shifts and coupling constants for brain metabolites. NMR Biomed. 2000; 13(3): 129-53.
- Govind V, Young K, Maudsley AA. Corrigendum: proton NMR chemical shifts and coupling constants for brain metabolites. Govindaraju V, Young K, Maudsley AA, NMR Biomed. 2000; 13: 129-153. NMR Biomed. 2015; 28(7): 923-4.

