Clinical Image - Volume 3 - Issue 4
Worm or wool? That is the question?
Sarishna Singh1,2; Christoffel J. Opperman1,2,3
1National Health Laboratory Service, Green Point TB Laboratory, Cape Town, South Africa.
2SAMRC Centre for Tuberculosis Research, Division of Molecular Biology and Human Genetics, Faculty of Medicine and Health Sciences, Stellenbosch University, South Africa.
3Division Microbiology, Department of Pathology, Honorary lecture, University of Cape Town, Groote Schuur Hospital.
Received Date : May 11, 2023
Accepted Date : June 26, 2023
Published Date: July 03, 2023
Copyright:© Sarishna Singh 2023
*Corresponding Author : Sarishna Singh, SAMRC Centre for Tuberculosis Research, Division of Molecular Biology and Human Genetics, Faculty of Medicine and Health Sciences, Stellenbosch University, South Africa.
Email: sarishna.singh@nhls.ac.za
DOI: Doi.org/10.55920/2771-019X/1474
Keywords: Parasite; False-positive; Microscopy
Clinical Image
With an increase in migration and travel, physicians should have an index of suspicion for parasitic infection. Parasitic worms that can affect the lung include trematodes, protozoa and nematodes [1]. Diagnostic investigations such as serology are prone to cross-reactions [2]. Blood eosinophilia may be absent in immunocompromised patients with Strongyloides hyperinfection syndrome [3]. In addition, Ascaris eggs are only passed in the stool following pulmonary symptom resolution, and many non-infectious causes of pulmonary eosinophilia have been described [1]. Therefore, direct microscopy is a valuable option to identify the parasite when larvae migrate to the lungs, which is common for many parasitic infections.
However, one should be cautious not to over-diagnose parasitic infections in sputum samples. For example, these "worm" structures, lacking internal organs, are artefacts in the images provided (Figure 1 and 2). From a parasitologist's experience, false-positive causes might include plastic remnants from when the grooves were made for the container lid, fibers if cotton wool swabs were used during sample collection or processing and organic material in stool samples. In conclusion, false positive identification can occur if a trained microbiologist does not view the slides.
Conflict of interest statement
The authors have declared that no competing interest exists.
Author contributions
SS conceptualized the manuscript. SS and CO wrote the first draft. All authors reviewed, edited and approved the final manuscript.
Funding
The research received no specific grant from any funding agent in the public, commercial or not for profit sectors.
Ethical approval
Patient data was anonymized for the publication of these laboratory image(s)
Data sharing
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Acknowledgement
We want to thank Professor John Frean, from the Parasitology Lab, Centre for Emerging Zoonotic and Parasitic Diseases at the National Institute for Communicable Diseases, Johannesburg, South Africa, for sharing his insight and experience dealing with false-positive parasitic specimens.
We would also like to thank Mogamad Davids from the Green Point Haematology Lab for assisting with the performance of Wrights stains and the TB technologists at Green Point TB lab for the performance of auramine and Ziehl Neelsen stains.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect official policy or position of any affiliated agency of the authors.
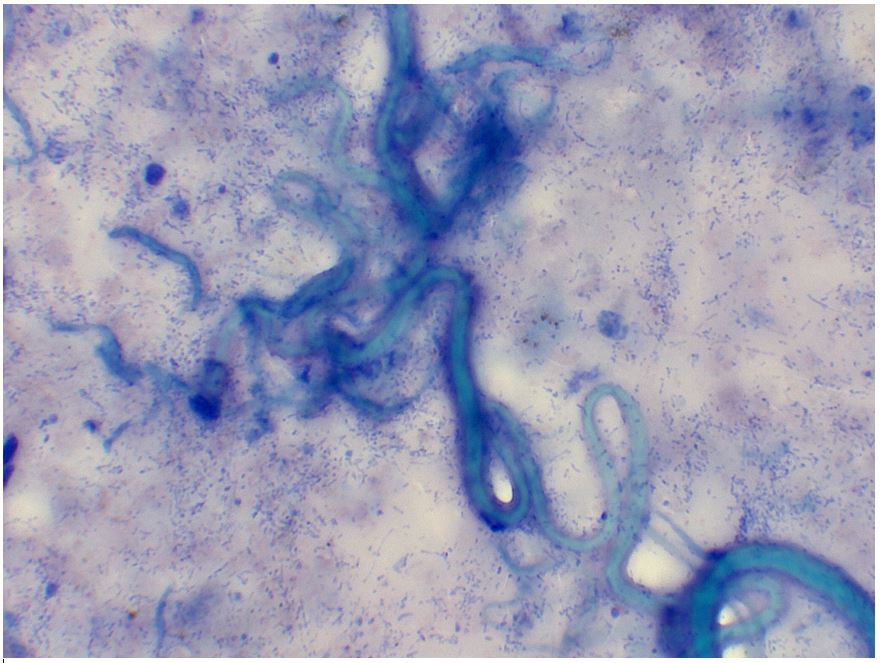
Figure 1: Wrights stain. No internal structures seen.
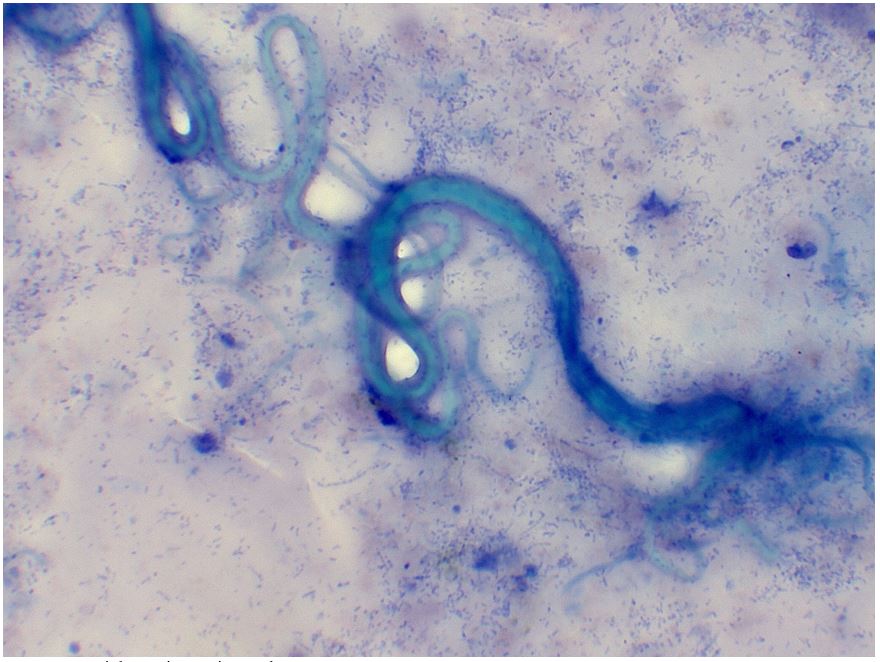
Figure 2: Wrights stain. No internal structures seen.
References
- Kunst H, Mack D, Kon OM, Banerjee AK, Chiodini P, Grant A. Parasitic infections of the lung: a guide for the respiratory physician. Thorax. 2011; 66(6): 528-36.
- Jin Y, Kim EM, Choi MH, Oh MD, Hong ST. Significance of serology by multi-antigen ELISA for tissue helminthiases in Korea. J Korean Med Sci. 2017; 32(7): 1118-1123.
- Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev. 2004; 17(1): 208-217.

