Case report - Volume 3 - Issue 4
Toxocariasis, as a cause of multiple pulmonary and liver nodules in an immunocompetent adult
Guesmi Z1,4*; Hannachi S1,4; Mtibaa L2,4; Jemli B2; Msolli AS3; Arous Y3,4; Abid R1,4; Battikh R1,4
1Department of Infectious Disease, Military Hospital of Tunis, Tunisia
2Laboratory of Mycology, Parasitology. Military Hospital of Tunis, Tunisia
3Department of Radiology. Military Hospital of Tunis, Tunisia
4Faculty of Medicine of Tunis, University Tunis El Manar, Tunisia.
Received Date : May 14, 2023
Accepted Date : June 28, 2023
Published Date: July 05, 2023
Copyright:© Guesmi Z 2023
*Corresponding Author : Guesmi Z, Department of Infectious Disease, Military Hospital of Tunis, Faculty of Medicine of Tunis, University Tunis El Manar, Tunisia.
Email: zeinebguesmi92@gmail.com
DOI: Doi.org/10.55920/2771-019X/1479
Abstract
Introduction: Human toxocariasis is a cosmopolite parasitic infection due to an helminth Toxocara canis (T.canis) and Toxocara catis(T.catis). Visceral larva migrans constitutes a rare and doubtful form. We reported the case of a visceral larva migrans with a concomitant localization in lung and liver.
Case: A 59-year-old male, who presented with fever, myalgia and dry cough evolving for two weeks. He has no medical or travel history. The clinical examination was unremarkable. Chest and abdominal computed tomography (CT) showed multiple parenchymal condensations in both lungs and a normal size liver with multiple subcentimetric hypodense nodular lesions. A serologic diagnosis of Toxocara infection (ELISA and Western blot) was positive. The diagnosis of pulmonary and hepatic toxocariasis was established. He was treated with albendazole for one month. The outcome was favorable
Conclusion: Toxocariasis is a diagnosis to be considered in many situations. It is curable under well conducted treatment. Preventive measures are also important which are based especially on the rules of hygiene.
Introduction
Human toxocariasisis a cosmopolite parasitic infection due to an helminth Toxocara canis (T.canis) and Toxocara catis (T.catis) transmitted by dogs and cats, respectively. It represents one of the main causes of hypereosinophilia but it is misdiagnosed. It can affect all sites. It’s often an asymptomatic and benign infection and can be recovered without treatment. But some forms are serious and can be life-threatening. Visceral larva migrans constitutes a rare and doubtful form. Clinical signs and radiologic features are not specific, which can mislead the positive diagnosis. In order to consider this diagnosis, although a non-specific presentation, we reported the case of a visceral larva migrans with a concomitant localization in lung and liver.
Case report
We report the case of a 59-year-old male, who presented with fever, myalgia and dry cough evolving for two weeks. He has no medical or travel history. The clinical examination was unremarkable unless a fever of 38,5°C. Laboratory findings showed, CBC by 21.2 × 109/L, eosinophils by 10 × 109/L. Serum C-reactive protein was by 14 mg/L (N <5 mg/l) and LDH count was by 560 U/L (N = 190-400 UI/L). Results of other routine biochemistry investigations were within normal limits. IgE levels were high. Tuberculosis tests and HIV serology were negatives. The serum tumor markers are at normal levels. Chest and abdominal computed tomography (CT) showed multiple parenchymal condensations surrounded by a peripheral halo in both lungs (Fig.1A) and a normal size liver with multiple subcentimetric hypodense nodular lesions (Fig.2A). A serologic diagnosis of Toxocara infection (ELISA and Western blot) was positive. The serology of other helminthiases such as hydatic kyst, anguillulosis, bilharziosis and distomatosis were negative as well as urine and stool parasite test. The diagnosis of pulmonary and hepatic toxocariasis was established. No evidence of other visceral localization was proved (brain MRI and ocular examination were normal).
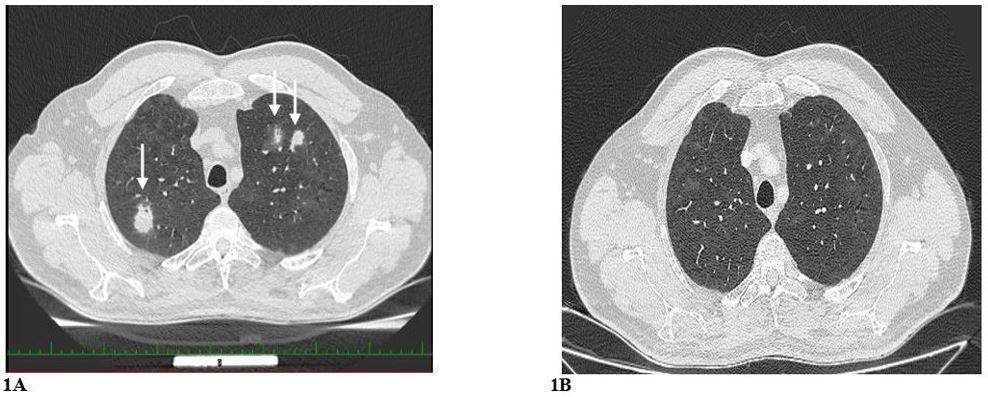
Figure 1A: Chest CT scan showed multiple parenchymal condensations surrounded by a peripheral halo in both lungs (arrows).
1B: Chest CT scan showed regression of the pulmonary nodules after the course of albendazole.
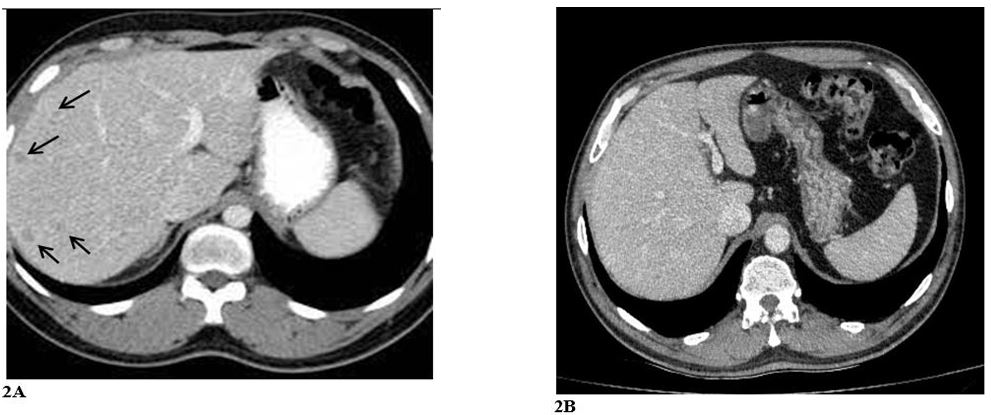
Figure 2A: Abdominal CT scan showed multiple liver subcentimetric hypodense nodular lesions (arrows).
2B: Abdominal CT scan showed disappearance of the liver nodules after the course of albendazole.
An eventual heart toxicity du to eosinophilia was eliminated: cardiac enzymes and the cardiac ultrasound were normal. The interrogation revealed the history of forest herbs consumption and the presence of dogs and cats since childhood. He was treated with albendazole (400 mg x2 orally per day) for one month. The outcome was favorable, with disappearance of the cough and decline of hypereosinophilia. The follow-up CT scan showed disappearance of the liver nodules and regression of the pulmonary nodules after the course of albendazole (Fig.1B; 2B). At 6 months the serological control in ELISA had objectified a drop in the level of antibodies.
Discussion
Humans are accidental hosts of toxacarosis. They are contaminated by ingesting embryonated eggs present on the ground, in water or in foods oiled by cat or dog faeces, or by ingesting the larvae that reside in the intestines of paratenic hosts (rabbits, chickens, etc.) (Fig 3) [1,2]. For our patient, he reported the consumption of forest plants and the presence of dogs in the area, which could be the source of contamination. After ingestion, the eggs arrive in the intestines in the larvae stage to reach the portal veins and then the liver, the right heart circulation, the lungs and all the other organs [3,4]. There are different forms and presentations of this infection depending on the organ affected: neurotoxocariasis, ocular toxocariasis, visceral larva migrans and common larva migrans.
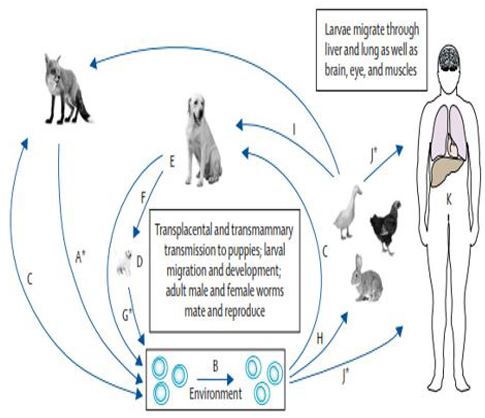
Figure 3: The routes of human contamination by toxocariasis [1].
Our patient presented with a visceral larva migrans. The liver is the most affected organ in this form. Our patient has a hepatic localization but also a much rarer localization which is the pulmonary involvement. This form of the disease is more common in children aged between 2 and 7 years [2]. Cases in adults have been reported [5]. Affected individuals are often asymptomatic. Nevertheless, non-specific signs may appear: fever, asthenia, abdominal pain [5], hepatosplenomegaly may also be noted. For pulmonary involvement, cough, dyspnea, wheezing may occur. In this location the parenchymal involvement is due to a local allergic reaction to toxocariasis larvae. In some cases, it may be responsible for chronic eosinophilic pneumonia. Investigation by bronchoalveolar lavage and/or bronchial biopsy revealed the presence of predominantly eosinophilic hypercellularity [6]. In biology, hypereosinophilia is the most reliable sign that guides the diagnosis. On the other hand, at very high levels, it is a criteria of severity that can be life-threatening, especially with the cardiactoxicity of eosinophils. Our patient had no cardiac involvement.
The radiological signs are also non-specific and can be confused with many infectious, inflammatory and tumor diseases. Most commonly, they are pulmonary nodules surrounded by a peripheral halo or ground glass nodules. Their size varies from 4 to 40 mm. Their distribution is diffuse or predominantly in subpleural areas. Condensations are usually associated with the most severe clinical presentations. Finally, eosinophilic pleurisy, pneumothorax and cavities are rare [7-9].
For liver involvement, our patient had a normal liver size with multiple subcentimetric hypodense nodular lesions. On CT or MR imaging, hepatic lesions are seen as multiple, ill-defined, oval lesions that measure 1.0–1.5 cm in diameter. Sometimes, the lesion may be angular or trapezoidal. On sonography, the lesions appear as multiple, small, oval hypoechoic lesions in the liver parenchyma. The lesions differ from metastatic nodules is as much as they have fuzzy margins, are uniform in size, non-spherical in shape and are best seen on portal venous phase[7]. A migratory character of the lesions can be noted which supports the diagnosis of larva migrans [4,10].
Diagnostic confirmation was based on serology using both ELISA and Western blot methods. In fact, several false positives have been reported with the ELISA method. The combination of ELISA and BLOT has shown a better sensitivity and specificity [2]. However, it does not distinguish between asymptomatic carriage and progressive infection. Other diagnostic methods can be used, notably histological studies and molecular biology. The latter allows a more rapid and specific analysis. PCR of toxocariasis is based on several genetic markers, notably the ITS 1 and ITS2 regions of the rDNA [2].
Recovery can be spontaneous and without sequelae. But in the case of severe infections, treatment is mandatory. Two molecules have shown their effectiveness: albendazole and mebendazole. Albendazole has a better tissue diffusion, hence its wider use. The recommended dose is 400 mg twice a day. A duration of at least one month is recommended in order to avoid relapses [11].The combination of corticosteroids has been used in several cases, especially with ocular and pulmonary involvement. In our patient, no corticosteroid was used
Conclusion
Toxocariasis is a diagnosis to be considered in many situations. It constitutes, by its different forms, a public health challenge. Its diagnosis is easy and is based on serology and molecular biology, which must be developed in our country. It is curable under well conducted treatment. Preventive measures are also important which are based especially on the rules of hygiene.
References
- Ma G, Holland CV, Wang T, Hofmann A, Fan C-K, Maizels RM, et al. Human toxocariasis. The Lancet Infectious Diseases. 2018; 18: e14–24.
- Chen J, Liu Q, Liu G-H, Zheng W-B, Hong S-J, Sugiyama H, et al. Toxocariasis: a silent threat with a progressive public health impact. Infect Dis Poverty. 2018; 7: 59.
- Gakosso C, Baadi F, Abakka FZ, Basraoui D, Jalal H. The visceral larva migrans caused by Toxocara canis: a case report. Pan Afr Med J. 2020; 36.
- Gemmell A. Toxocariasis as a cause of multiple pulmonary nodules in a paediatric patient. Case Reports 2015; 2015: bcr2014207073–bcr2014207073.
- Choi SJ, Kim JE, Park CH, Yang DM. Pulmonary and Hepatic Involvement of Toxocariasis in an Adult: Case Report. J Korean Radiol Soc. 2004; 51: 205.
- Inoue K, Inoue Y, Nawa Y, Mitsunori SY. Eosinophilic Pneumonia Due to Visceral Larva Migrans. 2002; 41: 5.
- Dietrich CF, Cretu C, Dong Y. Imaging of toxocariasis. Advances in Parasitology. Elsevier. 2020; 109: 165–87.
- Jorge D, Strady C, Guy B, Deslée G, Lebargy F, Dury S. Opacités pulmonaires multiples révélant une toxocarose. Revue de Pneumologie Clinique 2016; 72: 273-6.
- Sakai S, Shida Y, Takahashi N, Yabuuchi H, Soeda H, Okafuji T, et al. Pulmonary Lesions Associated With Visceral Larva Migrans Due to Ascaris suum or Toxocara canis : Imaging of Six Cases. American Journal of Roentgenology. 2006;186:1697–702.
- Kang YR, Kim S-A, Jeon K, Koh W-J, Suh GY, Chung MP, et al. Toxocariasis as a cause of new pulmonary infiltrates. Int j Tuberc Lung Dis. 2013; 17: 412–7.
- Park EJ, Song JY, Choi MJ, Jeon JH, Choi J, Yang TU, et al. Pulmonary Toxocariasis Mimicking Invasive Aspergillosis in a Patient with Ulcerative Colitis. Korean J Parasitol. 2014; 52: 425-8.

