Case report - Volume 3 - Issue 4
A uniportal video-assisted thoracic surgery approach for lung cancer with silicosis and highly inflammatory lymph nodes
Takuya Watanabe; Eriko Suzuki; Naoko Yoshii; Takuya Kohama; Kensuke Iguchi; Minori Nakamura; Takumi Endo; Masayuki Tanahashi
Division of Thoracic Surgery, Respiratory Disease Center, Seirei Mikatahara General Hospital, 3453, Mikatahara-cho, Kita-ku Hamamatsu, Shizuoka, Japan.
Received Date : May 18, 2023
Accepted Date : June 29, 2023
Published Date: July 06, 2023
Copyright:© Takuya Watanabe 2023
*Corresponding Author : Takuya Watanabe, MD, PhD, Division of Thoracic Surgery, Respiratory Disease Center, Seirei Mikatahara General Hospital, 3453, Mikatahara-cho, Kita-ku Hamamatsu, Shizuoka 4338558, Japan.
Email: takuya.watanabe@sis.seirei.or.jp
DOI: Doi.org/10.55920/2771-019X/1480
Abstract
While uniportal video-assisted thoracic surgery (U-VATS) is a viable minimally invasive surgical approach, it may restrict the control of surgical instruments. Furthermore, whether or not U-VATS is well-indicated for lung cancer with silicosis and inflammatory lymph nodes is unclear. We herein report a case of resection performed by U-VATS for lung cancer with silicosis and highly inflammatory lymph nodes and describe the procedures and techniques used. The vessels and bronchus cannot be dissected easily in the hilum due to the presence of several extremely inflamed lymph nodes, and these structures had to be exposed while avoiding inflammatory lymph nodes #10 and #12u in this case. Curved instruments and hooked electrocautery proved useful for these procedures. In addition, the grasping technique using the curved forceps was useful for achieving sufficient tension to expose the vessels. Bulk dissection of the pulmonary artery and bronchus with a stapler may be useful when these structures cannot be isolated, such as with B1 and A2a in the present case. The postoperative course was good, and the patient was discharged on postoperative day 6. Substantial experience and knowledge as well as proficiency with the associated techniques will make difficult surgeries such as this case possible by U-VATS.
Keywords: Uniportal video-assisted thoracoscopic surgery (U-VATS); Uniport; Single port surgery; Silicosis; Lymph node; Lung cancer
Introduction
While uniportal video-assisted thoracic surgery (U-VATS) is a viable minimally invasive surgical approach [1], it may restrict the control of surgical instruments. Surgery for lung cancer with silicosis and inflammatory lymph nodes is always difficult, and U-VATS is not considered to be a good indication for such cases. In general, inflammatory lymph nodes cannot be dissected easily, so the vessels and bronchi are cut at the periphery while avoiding these lymph nodes via approaches such as open thoracotomy or multiport VATS. We herein report a case of resection performed by U-VATS for lung cancer with silicosis and highly inflammatory lymph nodes and describe the procedures and techniques used.
Case presentation
A 79-year-old man had worked in the stone industry for over 60 years. Chest computed tomography (CT) at a medical checkup revealed a 2.8-cm nodule in the right upper lobe (Fig. 1A). Adenocarcinoma was detected via a bronchoscopic biopsy, and he was diagnosed with resectable stage IA3 lung cancer. Enhanced CT showed silicosis in the whole lobes as well as multiple highly inflammatory lymph nodes with calcification (Fig. 1B). In addition, a high accumulation on 18F-fluorodeoxyglucose-positron emission tomography in these lymph nodes was found (Fig. 1C). Conventionally, surgery in such cases is performed by open thoracotomy in our institution; however, due to recent advances in the U-VATS technique, U-VATS was selected for this patient.
Surgical techniques
The surgeon (the first author) stood on the right side of the patient, and a 4-cm wound was made at the 4th intercostal space (ICS), middle axillary line. While the 5th ICS is generally selected for right upper lobectomy, the 4th ICS was selected in this case to prepare for conversion to open thoracotomy depending on the intra-operative findings. There was no extensive adhesion in the thoracic cavity, but several highly inflammatory lymph nodes were found in the hilum and around the vessels. The interlobar fissure of the lung was insufficient, so a fissure-less procedure, from the anterior to the posterior direction, was selected.
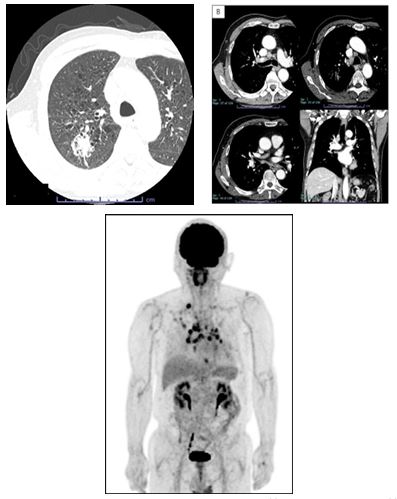
Figure 1: Chest computed tomography shown a 2.8-cm nodule in the right upper lobe (A), silicotic nodules in the whole lobes (A), and multiple highly inflammatory lymph nodes with calcification (B). A strong accumulation on 18F-fluorodeoxyglucose-positron emission tomography in these lymph nodes was found (C).
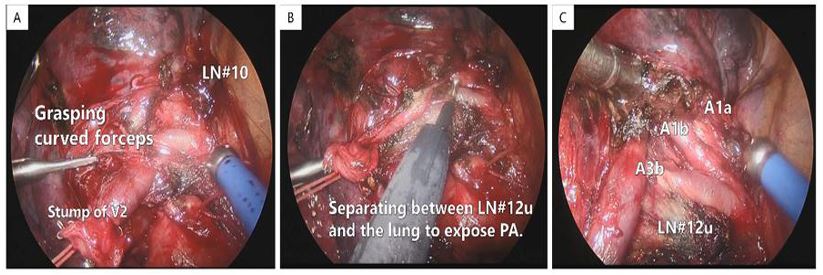
Figure 2: The inflammatory lymph nodes #10 and #12u were strongly attached to the pulmonary arteries in the hilum (A, B). The PAs were exposed while avoiding the inflammatory lymph nodes using hooked electrocautery to separate the lung and lymph nodes (B). A1a, A1b, and A3b were exposed at the periphery and dissected with an ultrasonic cutting coagulation device (C).
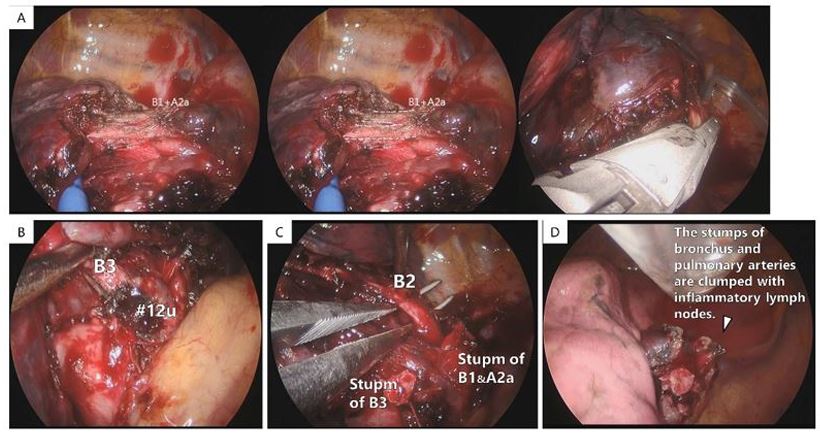
Figure 3: Bronchus B1 and PA recurrent A2a could not be isolated due to the presence of inflammatory lymph node #12u (A). B1 and A2a were dissected by a stapler (SigniaTM 45-mm purple curved cartridge; Medtronic Company) at the same time (A). B3 and B2 were also exposed at the periphery while avoiding the inflammatory lymph node #12u (B, C). After lobectomy, the stumps of the bronchus and PAs were seen clumping with the inflammatory lymph nodes in the hilum (D).
Parts of the inflammatory lymph nodes in the hilum were sampled were confirmed to be free from metastasis based on an intraoperative pathological diagnosis. Pulmonary vein (PV) V1-3 was then cut with the stapler. The stump of the PV was ligated and lifted up, and pulmonary artery (PA) A3b was dissected with ligation and an ultrasonic cutting coagulation device (Harmonic®1100 shears ETHICON ENDO-SURGERY, INC., Cincinnati, OH, USA). The pleura of the hilum was then dissected, and inflammatory lymph nodes #10 and #12u were identified (Fig. 2A). The lymph nodes were strongly attached to the PAs around the hilum, so dissection of those PAs would require cutting at the periphery. The PAs were exposed while avoiding the inflammatory lymph nodes using hooked electrocautery to separate the lung and lymph nodes (Fig. 2B). The grasping technique using the curved forceps proved particularly useful for achieving sufficient tension to expose the vessels (Fig. 2A). A1a, A1b, and A3b were exposed, and dissected with an ultrasonic cutting coagulation device (Fig. 2C).
Bronchus B1 and recurrent A2a were exposed under the azygos vein, but the two could not be isolated due to the presence of inflammatory lymph node #12u. Therefore, B1 and A2a were dissected with a stapler (Endo GIA™ 45 mm Curved Tip Articulating Medium/Thick Reload with Tri-Staple™ Technology; Medtronic plc. Dublin, Ireland.) (Fig. 3A). B3 was dissected after ligation, and B2 was exposed in the lung (Fig. 3B, 3C). V4x from V2 was found and dissected, and A2b was exposed. Lymph node #12u was strongly attached to the vessel, and A2b was dissected at the root of the vessel with ligation and an ultrasonic cutting coagulation device. Finally, the interlobar fissure, upper-middle and upper-lower, was dissected from the anterior to the posterior direction with the stapler, and the procedure was completed by U-VATS (Fig. 3D).
Mediastinal lymph node dissection was not performed because no metastasis had been found. There was no air leakage from the lungs. A single thoracic drainage tube was placed, and the surgery was completed. The surgical video is available online.
After the surgery, the patient had no complications, the drainage tube was removed on postoperative day 2, and he was discharged on postoperative day 6. The pathological diagnosis was invasive adenocarcinoma without lymph node metastasis, stage IA2, with pneumoconiosis and nodular silicosis. No recurrence has been seen in one year since the surgery.
Discussion
U-VATS is accepted for the performance of all kinds of anatomical lung resection procedures worldwide [2]. Standard lobectomy has been generally reported to be safe and reliable for advanced lung cancer [3]. However, there are few reports concerning the indication of U-VATS for cases with silicosis and/or inflammatory lymph nodes.
Aragón et al. reported on the influence of silicosis in U-VATS, wherein silicosis was described as a risk factor for postoperative complications [4]. This is considered to be because the surgical process is necessarily complicated due to silicotic changes, and the presence of inflammatory lymph nodes makes dissection of the vessels difficult. Dr. Diego Gonzalez-Rivas, the authority of U-VATS, has described that U-VATS should be indicated for intractable cases when the surgeon has accumulated the experiences and matured the techniques [3, 5]. This means that it is indeed possible to perform surgery via a U-VATS approach for cases with silicosis and inflamed lymph nodes provided the surgeon has sufficient skill and experience to perform the procedure safely and reliably.
Simultaneous stapling of the lobar bronchus and pulmonary artery is sometimes performed when the bronchus and pulmonary artery cannot be isolated due to the presence of inflammatory lymph nodes between them [6]. Our case underwent this procedure with dissection of B1 and A2a. The simultaneous stapling method is useful also in U-VATS, and the authors used three-line stapling in the present case. Notably, no intraoperative issues or postoperative complications were noted.
In the present case, the inflammatory lymph nodes were not metastatic nodes, so they were not dissected. However, if metastatic nodes are found, these lymph nodes must be dissected with the plasty technique of pulmonary and bronchus. The authors consider that such surgeries should be performed via thoracotomy to ensure safety except for the surgeon having special skills.
Conclusion
The indication of U-VATS in thoracic surgery is widening day-by-day, and remarkable advances in the technique have been made. Hopefully this paper and surgical video will help U-VATS surgeons achieve difficult lung cancer surgery in cases with silicosis and highly inflammatory lymph nodes.
Conflicts of interest: The authors declare no conflicts of interest.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from the patient for the publication of this article and accompanying images.
References
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis. 2014; 6: S650-S655.
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections-A clear advance. J Thorac Cardiovasc Surg. 2012; 144: S27-31.
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis. 2014; 6: 641-648.
- Aragón J, Méndez IP. Four years' experience in uniportal video-assisted thoracoscopic surgery for major lung resections: influence of silicosis in clinical outcomes. J Vis Surg. 2016; 2: 95.
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. Sci. World J. 2012; 2012: 780842.
- Murakami J, Ueda K, Hayashi M, et al. Simultaneous stapling of the lobar bronchus and pulmonary artery: is it actually dangerous? Interact Cardiovasc Thorac Surg. 2016; 22: 671-673.

