Clinical Image - Volume 3 - Issue 4
Prescription audit in an outpatient department of a Tertiary Care Teaching Hospital
Neha Fatima1*; Rani Indira Sinha2; Md. Ejaz Alam3
1Resident, Department of Pharmacology, Patna Medical College, Bihar, India.
2Professor and Head of the Department, Department of Pharmacology, PMCH, Bihar, India.
3Senior Resident, Department of Endocrinology, Government Medical college, Srinagar, India.
Received Date : May 17, 2023
Accepted Date : June 30, 2023
Published Date: July 07, 2023
Copyright:© Neha Fatima 2023
*Corresponding Author : Neha Fatima, Department of Pharmacology, Patna Medical College, Bihar, India.
Email: ejaz2k6@gmail.com
DOI: Doi.org/10.55920/2771-019X/1482
Introduction
An ‘audit’ is defined as ‘the review and the evaluation of the health care procedures and documentation for the purpose of comparing the quality of care which is provided, with the accepted standards’. Studying the prescribing audit is that part of the audit which seeks to monitor, evaluate and if necessary, suggest modifications in the prescribing practices of medical practitioners. Prescription Audit offers the most comprehensive overview of performance, detailing parameters as per the check list of prescription audit. Prescription writing is an important means of therapeutic intervention by the doctor and reflects his approach towards safe prescribing.
Aims and objective
To perform prescription audit for assessment of :-
i) General details of the patient.
ii) Medical component of prescription
iii) Prescribing indicators
Methodology
The study was designed and conducted as a prospective observational study at PMCH, Bihar, India after taking clearance from the Institutional Ethical Committee. The OPD based study was carried over a period of One month from 15th August to 15th September 2021.A total of 150 out-patient prescriptions were randomly sampled irrespective of department and disease of patient. Prescriptions were analysed for:- General details of patient on prescription Medical component Of prescription Prescribing indicators. The data obtained were summed up and presented as descriptive statistics using Microsoft Excel.
Inclusion criteria
Outdoor patients' prescriptions were reviewed. Prescriptions were reviewed irrespective of patient characteristics, diagnosis and hospital department.
Exclusion criteria
Patients admitted in emergency
Newborn patient admitted in nursery area.
Results
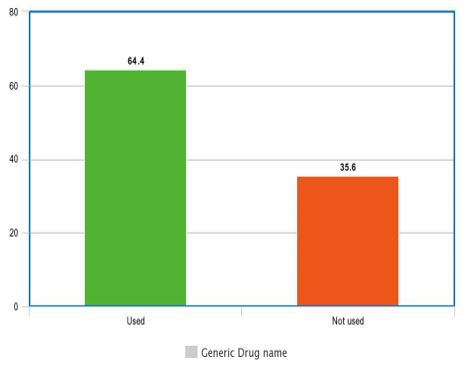
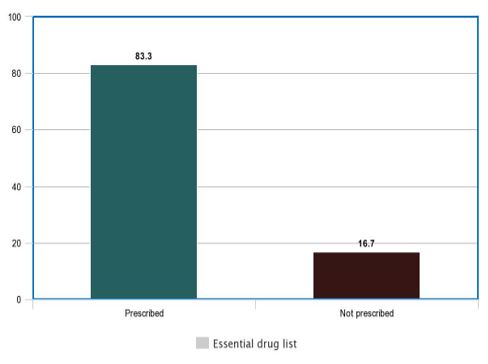
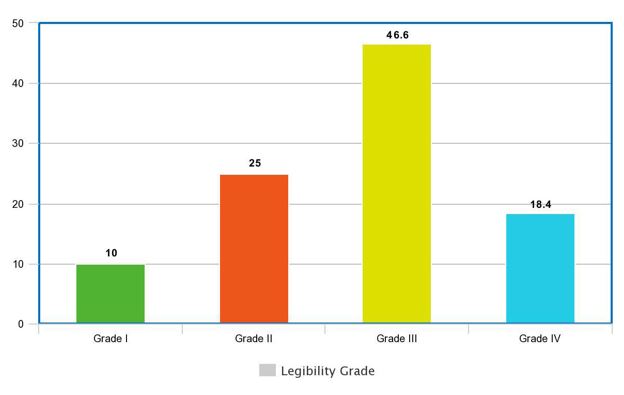
Among the 150 prescriptions analyzed, all (100%) of them had the general details, i.e. name, age, sex, and OPD registration number. In medical component: diagnosis was written in 53.3%, follow up advice was only in 16.6%Doctor's signature was found in 100% of prescriptions, but doctor's registration number was mentioned in none of them.46.6% of prescriptions was of grade III legibility. Around 90% of prescriptions had polypharmacy, EDL was 83.3% and generic drug used was 64.4%.
Discussion
Prescription is an important intervention by the physician and it is the ethical and legal duty of the practitioner to write complete and legible prescriptions. In my study I found that the date of prescription and patient’s details (name, age, sex, and address) were complete in all the prescriptions, while weight was not mentioned in any prescription. Patient details are important for ensuring that the correct patient receives the medicines and also for medico-legal and record-keeping purposes. Though the department and unit details were printed on all the prescriptions, doctors signature was present in all, the registration number of the doctors was not mentioned on any of the prescriptions. On analyzing the prescriptions I found that the prescriptions were incomplete with regards to mention of allergy status and follow-up advice was seen only in 16.6% . A large number of medication errors have been blamed on illegible writing of the prescriber. Illegible writing creates ambiguity and can potentially lead to dispensing of wrong drugs which can result in serious adverse events and even death. In my study, 10 % of the prescriptions were illegible and 46.6% were legible only with some difficulty. The percentage of antibiotics prescribed in my audit was 50% which is higher than the limits set by WHO (20-25.4%). 83.3% of the drugs were prescribed from the EDL or hospital formulary, whereas generic drug used in about 64.4%, it should have been 100% EDL and generic drug according to WHO.
Conclusion
Prescribing error may be considered one of the pathways to medical error that may lead to severe safety issues to the patients. The results of the present study show that it is necessary to critically address the completeness and legibility of the prescriptions in a continuous and frequent manner. To avoid confusion of legibility of prescription regulatory bodies in India advocates the use of capital letters while prescribing drugs. Further, this is the time to change handwritten prescription into electronic prescriptions to reduce medication errors.
References
- Rodríguez‑VeraFJ, Marín Y, Sánchez A, BorracheroC, PujolE. Illegible handwriting in medical records. JR Soc Med 2002; 95: 545‑6.
- Tulika Singh, Bratati Banerjee, Suneela Garg, Sanju Sharma. A prescription audit using the World Health Organization-recommended core drug use indicators in a rural hospital of Delhi, J Educ Health Promot. 2019; 8: 37

