Case report - Volume 3 - Issue 4
Embolization Using the Novel Menox Liquid Embolic System for Arteriovenous Fistulas: A Case Report
Audrius Sirvinskas*; Anrej Afanasjev
Interventional Radiology Department, Republican Vilnius University Hospital, Siltnamiu St. 29, 04130 Vilnius, Lithuania.
Received Date : May 20, 2023
Accepted Date : June 30, 2023
Published Date: July 10, 2023
Copyright:© Audrius Širvinskas 2023
*Corresponding Author : Audrius Širvinskas, Department of Interventional Radiology, Republican Vilnius University Hospital, Siltnamiu St. 29, 04130 Vilnius, Lithuania.
Email: audrius.sirvinskas@rvul.lt
DOI: Doi.org/10.55920/2771-019X/1484
Abstract
Thrombosis in the brain venous network may be one of the reasons for cerebral infarction related to arterial disease, which becomes a cause of concern as many cases of cerebral venous thrombosis (CVT) lead to mortality. Timely diagnosis and intervention lead to almost 80% of patient recovery, still about 15% of patients lead a disabled life. We present a case of a 62-year-old male, with no known comorbidity, admitted to the hospital with complaints of heaviness in his head and prominent pulsation in his left ear for 2 weeks. Magnetic resonance imaging showed a thinner left transversal sinus with thromboses or arteriovenous fistula (AVF). Cerebral angiography, performed for differentiation, showed occluded left sigmoidal sinus and fistula which was fed from the occipital, meningeal, and other arteries. The embolization was performed using the novel Menox 18 liquid embolic system (LES). The microcatheter was flushed with 0.5 mL of dimethyl sulfoxide and in total 9 ml of Menox 18 (ethylene vinyl alcohol) LES was injected from the downside via the left jugular vein under fluoroscopic guidance. Complete embolization of AVF was observed. Post-embolization cerebral angiography showed no AVF, filling arteries, or drainage veins. Other cerebral arteries and veins were totally compensated. No procedural complications were observed during embolization. The case emphasizes the effectiveness of the novel Menox LES in the successful treatment of severe CVT and AVF.
Keywords: Arteriovenous fistula, Cerebral venous thrombosis, Embolization, Menox liquid embolic system.
Abbreviations:
AVF: arteriovenous fistula
bAVM: brain arteriovenous malformation
CVST: cerebral venous sinus thrombosis
CVT: cerebral venous thrombosis
DMSO: dimethyl-sulfoxide
EVOH: ethylene vinyl alcohol copolymer
LES: liquid embolic system
MRI: magnetic resonance imaging
Introduction
The formation of blood clots in the brain’s venous sinuses leads to a condition known as cerebral venous sinus thrombosis (CVST). CVST, also known as cerebral venous thrombosis (CVT), results in the breaking of the blood cells causing blood leakage into the brain tissues, thereby resulting in hemorrhage [1]. Symptoms of CVT are nonspecific, which makes the diagnosis difficult [2,3]. The symptoms include focal neurological disturbances/loss, headaches, nausea, vomiting, altered consciousness, dizziness developing over days to weeks, cranial nerve palsies, papilledema, and seizures resulting in coma in some patients [4-6]. Deep venous thrombosis in patients leads to increased intracranial pressure, with an estimated mortality due to CVT of 5%-30%. However, early diagnosis and treatment can lead to favorable recovery, with about 80% of patients leading a normal life [7].
One of the well-established treatments is therapeutic embolization with embolic devices, which include coils, balloons, and particles/gelatin [8, 9]. The availability of a wide variety of commercial embolic devices shows the extent of therapeutic embolization performance and also represents manipulation in procedures on a case basis, depending upon the kind, place and severity [8-11]. Menox liquid embolic system (LES) (Meril Life Sciences Pvt. Ltd., India) is intended for pre-surgical embolization of brain arteriovenous malformation (bAVM). The liquid Menox comprises a mixture of ethylene vinyl alcohol copolymer (EVOH) dissolved in dimethyl-sulfoxide (DMSO) [12]. Micronized tantalum powder suspended in the liquid polymer/DMSO mixture provides fluoroscopic visualization [12]. It has shown satisfactory clinical outcomes as published earlier [12-14].
Here, we present a case study that highlights the successful application of the novel Menox LES in a patient treated for CVT and arteriovenous fistula (AVF).
Case description
A 62-year-old patient visited the hospital with complaints of heaviness in his head and prominent pulsation in his left ear for 2 weeks. The patient’s medical history did not show any known comorbidities or allergies. Once the written informed consent was obtained from the patient, magnetic resonance imaging (MRI) was performed, which showed a thinner left transversal sinus with thrombosis or an AVF. For performing cerebral angiography, a volume of 150 ml of Ultravist (contrast medium) 300 mg was used via right femoral artery and an Angio Seal (Terumo Corp., Somerset, NJ, USA) closure device was used for the closure of the puncture site. Angiogram revealed occluded left sigmoidal sinus and fistula that received feeding from various arteries such as occipital, meningeal, and others as shown in Figure 1 (A and B).
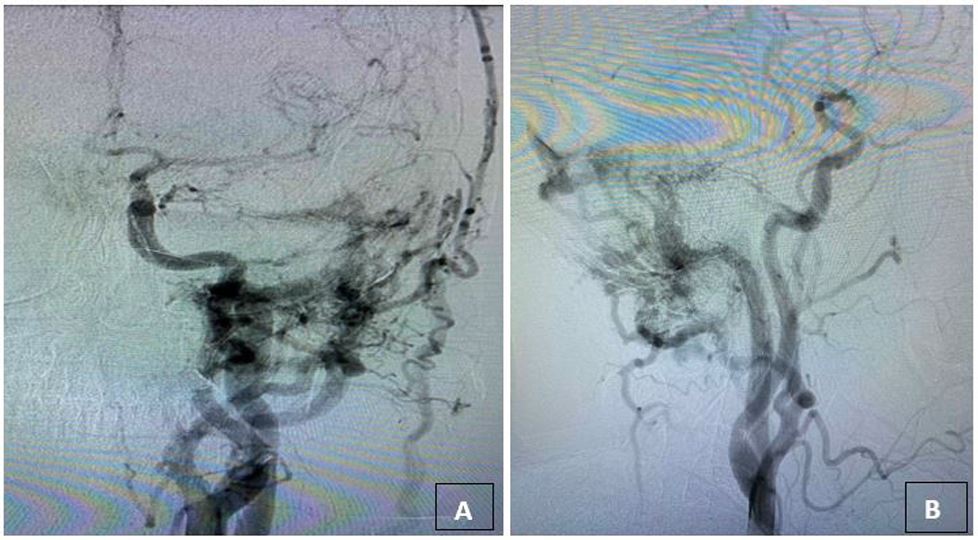
Figure 1: Pre-embolization direct left sigmoid sinus Fistula: A. Anteroposterior view and B. Lateral view.
The embolization was performed via two venous routes (upside and downside). The right jugular vein, right sigmoidal sinus, right and left transversal sinuses were utilized for upper venous side, wherein, Lantern microcatheter (Penumbra, Inc., USA) on Chikai 0.010” wire (Asahi Intecc., Japan) was inserted via retrograde venous way to reach the venous (ectatic) part of the AVF. Ectatic part was embolized with coils from the upside. The microcatheter was flushed with 0.5 ml of DMSO and in total 9 ml of Menox 18 LES was injected from the downside via the left jugular vein under fluoroscopic guidance. AVF was completely embolized, and AVF, filling arteries, or drainage veins were not seen in post-embolization cerebral angiography (Figure 2 [A-D]).
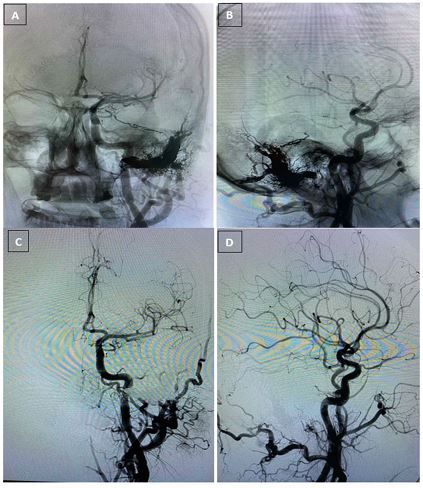
Figure 2: A. Cerebral angiography after the embolization – occluded left sigmoidal sinus and fistula. Feeding-from various arteries–occipital, meningeal, and others A. Anteroposterior view (unsubtracted image); B. Lateral view (nicely visible distribution of the LES within the tiny vessels); C. Anteroposterior view (subtracted image)-Cerebral angiography shows Menox 18 LES as seen forming a cohesive embolus (nicely cast): Cerebral angiography after the embolization – occluded left sigmoidal sinus and fistula. Feeding-from various arteries–occipital, meningeal, and others; D. Lateral view (subtracted image)-Cerebral angiography shows absence of AVF, no feeding arteries, and vein drainage is not seen (nicely visible distribution of the LES).
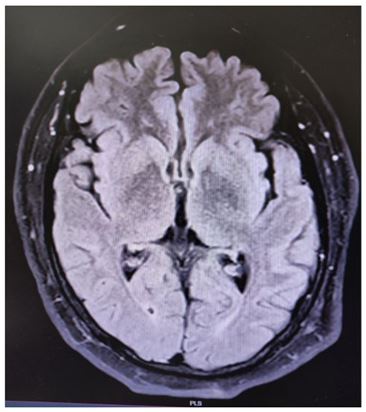
Figure 3: Magnetic Resonance Imaging image taken 48 hours after the embolization (post-procedure) No new ischemic events, or any other findings were noted. Fistula was observed to be non-functional.
Other cerebral arteries and veins were totally compensated. No complications during the embolization procedure were observed. The patient was extubated in the ICU for one night and later shifted to the neurosurgery department for two days under medical supervision. During this whole course, no adverse events occurred; Glasgow Coma Scale was 15, indicating healing of a traumatic head injury. MRI was repeated 48 hours after the embolization and no new ischemic events or any other findings were noted. As seen in figure 3, the fistula was not functioning.
The patient was discharged 4 days after embolization on therapeutic doses of fraxiparine as an anticoagulant, advised against strenuous activity for 2 months, and suggested angiographic monitoring after 6 months. A brain MRI was recommended during the 6 months follow-up for deep vein status, oedema, hemisphere venous infarcts, AVF venous component occlusion and possible hemorrhage.
Discussion
Generally, complete functional recovery in 75% to 80% of CVT patients has been reported when timely intervened. However, about 15% mortality and/or disability have been noted [10]. Risk factors like infections, malignancy, confusion or coma, intracranial hemorrhage, deep vein involvement, age, and gender (male) influence the outcomes of the treatment [10, 11]. Predominantly, anticoagulation is the first choice of treatment in CVT patients to prevent thrombus progression, thereby reducing the further complications of pulmonary embolus [15]. In severe cases or in cases where anticoagulation does not produce positive results, endovascular thrombolysis or mechanical thrombectomy become the choice of treatment [15].
A standard embolic agent is characterized or defined by its versatility of use, controllable chemical and physical properties for simplicity of application, ability to be monitored via X-ray fluoroscopy imaging, and predictability and assurance in terms of embolization rate and delivery distance [16]. The most commonly used agents are ethanol based (e.g., Ethibloc) or absolute ethanol, which can be used percutaneously or via catheter delivery system [8]. The drawback of ethanol is its anesthetic effect and pain for patients. The second most common agent is Lipiodol (Guerbet LLC, France), which is a mixture of iodinated poppy seed ethyl esters generally used for imaging of hepatocarcinomas [8]. Due to its high viscosity and prolonged vasculature clearance, its suitability for the treatment, as transarterial chemoembolization is preferred. Of late, the novel non-adhesive liquid embolic agent Menox LES, comprised of EVOH copolymer dissolved in DMSO has demonstrated its feasibility in the treatment of cerebral AVMs [12]. Menox LES has been presented in 3 different viscosities, Menox LES 18 (18 cSt viscosity) (5% EVOH), Menox LES 20 (20 cSt viscosity) (6% EVOH) and Menox LES (34 cSt viscosity) (7% EVOH) [17]. The initial study report of Menox LES by Sirakov S et al. in 2019 [12] established Menox LES as having comparable results with well-established products Onyx (eV3-Covedien, Irvine, California, USA), Squid (Balt Extrusion, Montmorency, France) and PHIL (Microvention Inc, California, USA) [12]. In the reported study, 58.3% of the treated patients demonstrated curative embolization and partial embolization was reported in 42.6% of the patients. [12]. Another study was conducted to investigate the efficacy of using Menox LES in conjunction with PHIL through the same microcatheter for the endovascular embolization of cerebral AVMs. The average reduction in treated AVM size was 85%, ranging from 50%-100% while achieving 62.5% (10/16) complete embolization. There was no mortality or clinical follow-up worsening in the cases [14]. In the present case report, a similar outcome was observed where no procedural complications were seen and ease of use of Menox LES was also demonstrated. Slow infusion was achieved due to its lower viscosity and successful embolization of CVT was achieved.
Conclusion
Effective management of AVF was achieved using novel Menox LES 18 with no drainage in veins, absence of filling arteries and no embolization procedural complications. The patient was successfully discharged from the hospital with medical advice. Our case emphasizes the effectiveness of the Menox LES in the successful treatment of severe CVT. However, a large cohort, prospective study is required to prove the safety and efficacy of novel Menox LES.
Conflict of interest
Declarations of interest: The authors declare no potential conflicts of interest for this article.
Acknowledgment
We would like to acknowledge Dr. Dolly Singh for her significant contribution in drafting and finalization of the case report.
References
- Gokey R and M Das J. Venous Sinus Thrombosis. [Updated 2022 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560598/
- Karthikeyan D, Vijay S, Kumar T and Kanth L. Cerebral venous thrombosis-spectrum of CT findings. Neuroradiol. 2004; 14: 129-37.
- Chiewvit P, Piyapittayanan S and Poungvarin N. Cerebral venous thrombosis: diagnosis dilemma. Neurol Int. 2011; 3: e13.
- Ragurajaprakash K, Senthilkumar R, Prabu SS, Madeswaran K and Kiruthika P. Post-traumatic cerebral venous sinus thrombosis – Institutional study and literature review. Interdiscip Neurosurg. 2022; 27: 101398.
- Poon, CS, Chang JK, Swarnkar A, Johnson MH and Wasenko J. Radiologic diagnosis of cerebral venous thrombosis: pictorial review. AJR Am J Roentgenol. 2007; 189(6): S64-S75.
- Rodallec MH, KrainikA, Feydy A, Hélias A, Colombani JM, Jullès MC, Marteau V, Zins M. Cerebral venous thrombosis and multidetector CT angiography: tips and tricks. RadioGraphics. 2006; 26: S5-S18.
- Crombe D, Haven Fr and Gille M. Isolated deep cerebral venous thrombosis diagnosed on CT and MR imaging. a case study and review literature review. JBR–BTR 2003; 86: 257-61.
- Patel S and Ratnam LA. Liquid Embolics: Emerging Options and Applications. A review of current liquid embolic agents and future prospects. Endovasc today. 2022; 21(4): 58-63.
- Jasmine Lord J, Hugh Britton H, Sebastian G. and Lewis LA. Advancements in the development on new liquid embolic agents for use in therapeutic embolization. J Mater Chem B. 2020; 8: 8207-8218.
- Ulivi L, Squitieri M, Cohen H, Cowley P and Werring JD. Cerebral venous thrombosis: a practical guide. Pract Neurol. 2020; 20: 356-367.
- Ferro JM, Canhao P, Stam J, Bousser, MG, Barinagarrementeria, F and ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004; 35: 664-70.
- Sirakov S, Sirakov A, Minkin K, Penkov M, Ninov K, Hristov H, Karakostav V, Orlov K et al. Initial experience with the new ethylene vinyl alcohol copolymer based liquid embolic agent Menox in the endovascular treatment of cerebral arteriovenous malformations. J Neurointerv Surg. 2019; 11(10): 1040-1044.
- Aslanidi C, Sofia Athanasiou S, Charalambous C, Mamalis V, Papadopoulos C, Arhontakis E, Tsanis A. Endovascular treatment of a post-traumatic pseudoaneurysm arising from a ruptured posterior tibial artery with Menox. A case report. Radiol Case Rep. 2021; 16(11): 3231-3236.
- Sirakov A, Minkin K and Sirakov S. Intermixed Dimethyl-Sulfoxide-Based Nonadhesive Liquid Embolic Agents Delivered Serially via the Same Microcatheter for Cerebral AVM Treatment. AJNR Am J Neuroradiol. 2020; 41(4): 681-686.
- Behrouzi R and Punter M. Diagnosis and management of cerebral venous thrombosis. Clin Med (Lond). 2018; 18 (1): 75-79.
- Ko G, Choi JW, Lee N, Kim D, Hyeon T and Kim HC. Recent progress in liquid embolic agents. Biomater. 2022; 287: 121634. ISSN 0142-9612.
- https://www.merillife.com/medical-devices/vascular-intervention/peripheral-vascular/menox.

