Case report - Volume 3 - Issue 4
Uveitis in with Juvenile Idiopathic Arthritis (JIA): Study of 12 cases
Yahya Saoiabi*; Meryem Sefrioui; Lazaar Hamza; Hala EL belidi; Noureddine Boutimzine; LO. Cherkaoui
Service d’ophtalmologie A de l’hopital des spécialités, Mohammed-V-Souissi University, center hospitalier universitaire, Rabat, Morocco.
Received Date : May 22, 2023
Accepted Date : July 06, 2023
Published Date: July 13, 2023
Copyright:© Yahya Saoiabi 2023
*Corresponding Author : Yahya Saoiabi, Service d’ophtalmologie A del’hopital des spécialités, Mohammed-V-Souissi University, center hospitalier universitaire, Rabat, Morocco.
Email: Saoiabi.yahya@gmail.com
DOI: Doi.org/10.55920/2771-019X/1491
Introduction
Uveitis is a serious complication of Juvenile Idiopathic Arthritis (JIA) that can lead to significant visual impairment or even blindness. It is the most common cause of uveitis in children and differs from uveitis associated with spondyloarthropathies by the paucity of its functional signs, resulting in diagnostic and therapeutic delays and affecting visual prognosis. The aim of our study was to identify the epidemiological, diagnostic and prognostic features of patients with uveitis associated with Juvenile Idiopathic Arthritis (JIA), as well as to discuss the complications and best therapeutic alternatives and prognostic data on these cases, shedding light on the challenges of managing this complex condition.
Materials and methods
We conducted a retrospective descriptive study covering a period of 10 years from 2009 to 2019, focusing on 12 children’s case with uveitis associated with juvenile idiopathic arthritis (JIA), within the Ophthalmology Department A at the Specialties Hospital of Rabat.
The following information was recorded: Age of onset of JIA, gender, number of arthritic joints and their progression, date of last examination, presence of Antinuclear Antibodies (AAN) and/or HLA-B27 antigen. The characteristics of uveitis were also noted, including the date of onset relative to the onset of joint involvement, unilateral or bilateral presentation (at onset or later), circumstances of diagnosis, and progression pattern (acute exacerbation or chronic course). Complications and finally the treatment proposed and response to treatment were also noted.
Inclusion criteria: This study included all patients under the age of 16 who were admitted and followed up in our department for uveitis associated with JIA with a follow-up period of at least 12 months.
Exclusion criteria: Patients with incomplete medical records and/or follow-up of less than 12 months were excluded from this study.
Limitations of the study: The available records in ophthalmology included only patients followed up for uveitis, which did not allow for a proper estimation of the percentage of uveitis occurring during the course of JIA.
Result: Our series, we have 12 patient files of patients with uveitis associated with Juvenile Idiopathic Arthritis (JIA).
Age: In these 12 children, the age of onset of JIA is on average 7 years old (4 to 11 years old), with 2 before the age of 6. Uveitis is diagnosed on average at the age of 9 (5 to 12 years old).
Gender: In this study, there is a clear female predominance (9F to 3M, or 75%).
History: 10 patients were followed up in pediatrics for juvenile idiopathic arthritis (83%).
Reason for consultation: 10 patients were referred for their complementary assessment of JIA as part of a systematic screening for uveitis. 2 patients consulted for functional signs (ocular pain and redness, photophobia, visual acuity reduction).
Clinical manifestations: Regarding JIA, 9 children have oligoarticular form, 2 child has polyarticular form, and 1 child has Enthesitis-Related Arthritis (ERA).
The discovery of arthritis preceded that of uveitis, with a diagnostic delay of 7 children: < 1 year, 4 children: <3 years. 1 children, the discovery of uveitis preceded that of arthritis.
Ophthalmologic examination: All our patients present anterior uveitis. Uveitis is bilateral in 8 children (66%).
Complementary assessment: ANA is positive in 9 of our patients (75%).
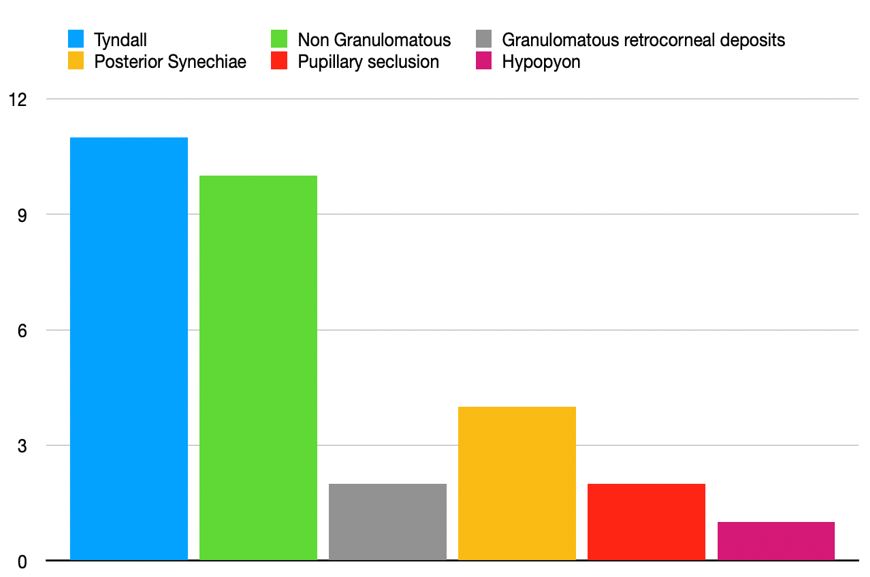
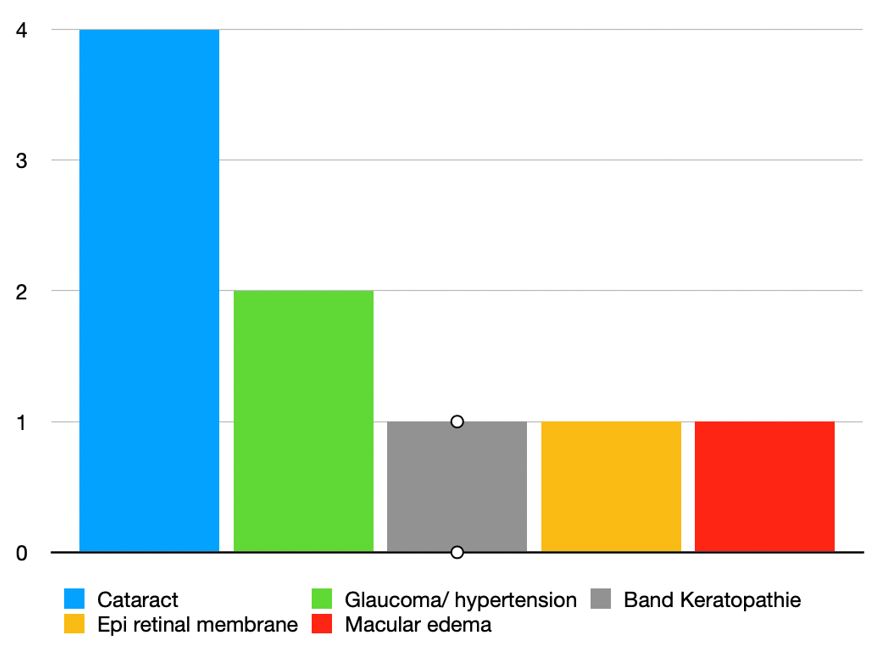
Complications: The evolution was marked by the development of several complications, which can coexist in the same patient:
4 Cases of cataracts, with surgical management
2 Cases of glaucoma
1 Case of band keratopathy
1 Macular edema
1 EPI retinal membrane
Treatment: All our patients received topical local corticosteroid therapy. 2 of our patients were put on methotrexate by their pediatrician.
Discussion
Epidemiology
The prevalence of uveitis in JIA varies between 4 and 24% depending on medical centers [3,1] and geographic origin. For example, the risk of uveitis in children with JIA is higher in Northern Europe than in individuals of Asian origin [3,1]. According to a meta-analysis of 26 different series, the worldwide incidence is estimated at 8.3% [5].
Risk Factors: The mean age at initial manifestation of JIA is between six and seven years.
Age: Regarding age, intraocular inflammation is mainly diagnosed between 4 and 6 years in the literature [1,5,19,4,23], compared to a mean age of diagnosis of 9 years in our series.
Sex: the literature results [1,5,19,4,23] are comparable to ours: 75-80% versus 75 %, respectively.
Clinical forms: The oligoarticular form is associated with uveitis in 75% of cases. In contrast, systemic juvenile idiopathic arthritis or rheumatoid factor-positive polyarthritis is rarely accompanied by uveitis (<1%) [1,5, ,4,]. In our series, 9 patients had oligoarticular form, 1 patient had rheumatoid arthritis with negative rheumatoid factor, and 1 patient had enthesitis.
Antinuclear antibodies (ANA): Antinuclear antibodies (ANA) are more frequently observed in JIA with uveitis (70-90%) than in JIA without uveitis (30-42%) (7,4,23). Therefore, the risk of developing uveitis is significantly higher in ANA-positive patients than in ANA-negative patients [1]. In our study, 75% of our patients had positive ANA.
Diagnostic circumstances: In the literature, ocular involvement precedes arthritis in 3-7% of cases [2], or is concomitant with arthritis in 25-33% of cases (3), suggesting the anteriority of ocular involvement over arthritis.
In our series,11 patients were diagnosed after being referred for complementary testing in the context of arthralgia, and 1 patient was diagnosed after consulting for ocular symptoms.
Clinical signs: The onset of uveitis is asymptomatic in 77% of cases (3). Most often, it is a chronic, asymptomatic, non-granulomatous anterior uveitis that evolves insidiously.
Even severe intraocular inflammation can remain asymptomatic, without any signs/ This was the case for 6 of our patients, who were diagnosed during complementary testing prescribed by their pediatrician as part of screening for their JIA.
When attention is drawn to ocular functional manifestations, most often there are already complications of unrecognized uveitis, with posterior involvement and macular edema. This chronic insidious form is more frequently found in the oligoarticular form of JIA [5,1,2].
On the other hand, during ERA [5,1,2 ,4], uveitis is acute and manifests with loud signs of pain, ocular redness, photophobia, and decreased visual acuity, leading the patient and parents to quickly seek an ophthalmologist, as was the case for 1 of our patients.
To make an early diagnosis of uveitis, all patients suspected of JIA or with confirmed JIA diagnosis should be systematically examined by an ophthalmologist, and parents should be sensitized to the occurrence of any symptoms. This requires close collaboration between pediatric rheumatologists and ophthalmologists.
Complication: JIA can lead to pupil seclusion and ocular hypertension. This is a common complication that is associated with a high risk of cataract and ocular hypertension [1,4,19] in our series 2 pupil seclusion were reported.
Cataract is the most frequent complication of JIA. It is secondary to the chronicity of intraocular inflammation and worsened by prolonged local and systemic corticosteroid treatment. Clinically, it begins with posterior subcapsular opacities, progressing in severe and prolonged forms to obstructive cataract. The risk of developing cataract early increases if there are posterior synechiae at the time of diagnosis (27). Within seven to ten years, about 30% of initially unaffected eyes with synechiae will also have cataracts. In cases of initial posterior synechiae, studies show an 80% incidence of cataract [4].
Glaucoma is a serious complication that appears in about 38% of cases. Ocular hypertension occurs in two-thirds of cases within two years of diagnosis. The risk of glaucoma is more common in AAN-positive forms (42%) than in AAN-negative forms (6%). Ocular hypertension can be of inflammatory origin due to trabecular damage, secondary to pupillary block, or iatrogenic in origin [8]. Macular edema is diagnosed early using OCT. 20% to 45% of patients present complications at the first ophthalmological examination [5,1,4]. Two or three decades ago, the reported complication rate was 60% to 90% after 6 to 10 years [1]. The frequency of complications has been reduced, and visual prognosis has improved in recent years [1,4]. However, uveitis associated with JIA is still correlated with a high risk of late sequelae and vision loss [1]. The presence of complications is a poor prognostic factor.
Medical Treatment: The goal of treatment is to achieve remission in order to avoid complications and preserve visual function. In acute anterior uveitis, only topical glucocorticoids are used in treatment. However, immunosuppressants and biologics discussed below are used in chronic uveitis. All of our patients were on systemic corticosteroid therapy except for one who was on methotrexate.
Topical treatments: Topical corticosteroids are the first-line treatment for both acute and chronic uveitis, with a frequency of instillation adapted to intraocular inflammation. A study has shown that a frequency of instillations less than or equal to 3 times per day reduces the risk of developing cataracts by 87% compared to a higher dose. [2].
General corticosteroid: General Corticosteroid is indicated for severe, chronic uveitis that is resistant to local treatment. It is initiated with methylprednisolone bolus in pediatric patients (1 g/1.73 m2 of body surface area), followed by oral prednisone at a dose of 60 mg/m2 of body surface area. The dosage is gradually decreased over several months depending on the evolution of intraocular inflammation, until the minimum effective daily dose is reached. The associated measures are the same as in adults. In our serie 7 of our patients received a bolus of methylprednisolone.
Immunosuppressants: Immunosuppressants are reserved for severe corticosteroid-resistant uveitis forms whose evolution may lead to blindness.
Methotrexate: In a meta-analysis of 9 studies, methotrexate was used in non-infectious uveitis in 135 patients, including 121 with juvenile idiopathic arthritis (JIA) [2]. The dose of 15 mg/m2 once weekly was most commonly used, with a maximum of 20 mg orally or 25 mg by subcutaneous injection [6]. The average response time to MTX treatment was 4.25 months with an average duration of 10.3 months to achieve complete remission [6]. Improvement in inflammation was observed in 73% of cases [2]. In another study, the use of methotrexate reduced the need for cataract surgery to 29% compared to 64% for patients who were never treated with methotrexate [14]. It is recommended to continue MTX for at least 12 months once uveitis is inactive and for 24 months in individuals with poor visual prognosis.
Mycophenolate mofetil: Mycophenolate mofetil is well-tolerated in children, with an 88% reduction in corticosteroid dose [13].
Tacrolimus, azathioprine, and cyclosporine: These medications are less frequently used in the treatment of uveitis associated with JIA.
Biologic therapies
particularly anti-TNFs, are used more frequently and have been shown to be effective. However, there seems to be a different response depending on the specific anti-TNF used. Several studies support the use of adalimumab (Humira®) in the treatment of uveitis associated with JIA. In one study [7], the combination of adalimumab and methotrexate-controlled inflammation with a lower treatment failure rate compared to children on methotrexate alone. However, patients who received adalimumab had a much higher incidence of serious adverse effects than those who received placebo [7]. A meta-analysis of 229 children with JIA-U showed that infliximab (Remicade®) and adalimumab have similar efficacy. (34) However, during 40 months of follow-up, uveitis remained in remission in 60% of cases in patients treated with adalimumab compared to 18.8% for patients treated with infliximab [10]. The duration of maintenance treatment with biologic agents is uncertain, although consensus recommendations suggest continuous maintenance treatment for 24 months after inflammation has ceased [2]. However, a reactivation of uveitis has been found in the majority of patients after stopping anti-TNF therapy [2].
Surgical treatment
Haut du formulaire
Bas du formulaire
Surgery is necessary in cases of complications that threaten visual function. In cases of band keratopathy, regular instillation every other day or corneal scraping under general anesthesia with an EDTA-based solution can eliminate calcium plaques obstructing the visual axis. Therapeutic photokeratectomy with excimer laser is also an effective method and can complement the action of EDTA. Cataract is a common complication during uveitis associated with JIA. Ocular inflammation must be controlled for at least 3 monthsbefore surgery. Preoperative treatment includes methylprednisolone boluses for 3 days. In our study 3 of our patients underwent cataract surgery [12]. In cases of secondary glaucoma, visual prognosis is poor. For one-third of glaucoma patients, surgery is indicated after failure of medical treatment and consists of an ideally non-perforating trabeculectomy, although the results are more uncertain. Goniotomy or drainage valve placement is an interesting secondary option [11].
Conclusion
Uveitis is the most common extra-articular complication of juvenile idiopathic arthritis (JIA). The identified risk factors for the development of uveitis in JIA include early age, female sex, oligoarticular form, and positivity for antinuclear antibodies (ANA). The diagnosis can be made during additional testing in the evaluation of joint pain or as a result of an eye-related symptomatology consultation. Complications of this ocular condition can be particularly severe and pose a threat to visual function. Early use of systemic immunosuppression has proven effective in treating intraocular inflammation and also helps avoid the side effects associated with corticosteroids. Biologic therapies, such as adalimumab, infliximab, and tocilizumab, represent a significant advancement in the treatment of uveitis associated with JIA, both in terms of efficacy and therapeutic safety. Close collaboration between pediatric rheumatologists and ophthalmologists, as well as regular and systematic screening with slit lamp examination, are essential for early diagnosis and optimal management of this condition, where the risk of unilateral or bilateral blindness remains a possibility.
References
- Arnd Heiligenhaus, Kirsten Minden, Dirk Föll, Uwe Pleyer. Uveitis in Juvenile Idiopathic Arthritis.Deutsches Ärzteblatt International | Dtsch Arztebl Int. 2015; 112: 92-100.
- Sarah L. N. Clarke, Ethan S. Sen and Athimalaipet V. Ramanan. Juvenile idiopathic arthritis-associated uveitis. Clarke et al. Pediatric Rheumatology. 2016; 14: 27.
- Marvillet I. Terrada C. Quartier P. Bui Quoc E. Bodaghi B. Prieur A.M. The threat to vision in juvenile idiopathic arthritis. Revue du Rhumatisme. 2009; 76: 673-679.
- Heiligenhaus A, Niewerth M, Ganser G, Heinz C, Minden K: Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population- based nation-wide study in Germany: suggested modification of the current screening guidelines. Rheumatology. 2007; 46: 1015-9.
- Carvounis PE, Herman DC, Cha S, Burke JP: Incidence and outcomes of uveitis in juvenile rheumatoid arthritis, a synthesis of the literature. Graefe ́s Arch Clin Exp Ophthalmol. 2006; 244: 281- 90.
- Foeldvari I, Wierk A. Methotrexate is an effective treatment for chronic uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2005; X(2): 362-5.
- Ramanan AV, Dick AD, Jones AP, McKay A, Williamson PR. Compeyrot- Lacassagne S. et al. Adalimumab plus Methotrexate for Uveitis in Juvenile Idiopathic Arthritis. N Engl J Med. 2017; 376(17): 1637-1646.
- Sijssens KM, et al. Ocular hypertension and secondary glaucoma in children with uveitis. Ophthalmology. 2006 ; 113 : 853-859 e2.
- Kotaniemi K, Kautiainen H, Karma A, Aho K: Occurrence of uveitis in recently diagnosed juvenile chronic arthritis. A prospective study. Ophthalmology 2001; 108: 2071-5.
- Simonini G, Taddio A, Cattalini M, Caputo R, De Libero C, Naviglio S, et al. Prevention of flare recurrences in childhood-refractory chronic uveitis: an open-label comparative study of adalimumab versus infliximab. Arthritis Care Res. 2011; 63(4): 612.
- Ho CL, Wong EY, Wallon DS. Goniosurgery for glaucoma complicating chronic childhood uveitis. Arch Ophthalmol 2004, 122 : 838- 844.
- Lundvall A, Zetterstrom C. Cataract extraction and intraocular lens implantation in children with uveitis. Br J Ophthalmol 2000; 84: 791-793.
- Brézin A. Les uvéites. Rapport de la société français d’ophtalmologie Paris: Masson. 2010.
- Sijssens KM et al. Risk factors for the development of cataract requiring surgery in uveitis associated with juvenile idiopathic arthritis. Am J Ophthalmol. 2007, 144 : 574-579.