Case report - Volume 3 - Issue 4
Spontaneous rupture of a benign renal cyst: A rare and misleading cause of Wünderlich syndrome
Kamel El-Reshaid1*; Shaikha Al-Bader2; Sayed Mohamad3
1Department of Medicine, Faculty of Medicine, Kuwait University, Kuwait.
2Department of Medicine, Nephrology unit, Amiri hospital, Ministry of health, Kuwait.
3Department of Radiology, Al Salam hospital, Kuwait.
Received Date : June 14, 2023
Accepted Date : July 12, 2023
Published Date: July 19, 2023
Copyright:© Kamel El-Reshaid 2023
*Corresponding Author : Kamel El-Reshaid, Professor, Department of Medicine, Faculty of Medicine, Kuwait University, Kuwait. Fax: (965) 25318454,
Email: kamel@hsc.edu.kw
DOI: Doi.org/10.55920/2771-019X/1499
Abstract
Wünderlich syndrome (WS) is a rare condition characterized by acute onset of spontaneous renal hemorrhage into the subcapsular and perirenal spaces. Wunderlich syndrome is classically characterized by the Lenk's triad: acute flank pain, flank mass, and hypovolemic shock. In this vignette; we describe our experience with a previously healthy adult female who presented with loin pain for weeks followed by gross hematuria, anemia and hypotension. Ultrasound examination of the abdomen and pelvis revealed; (a) an ill-defined hyperechoic mass-like lesion measuring 4.6X4.1 cm at its upper pole of right kidney which, on doppler study, had minimal internal vascularity, (b) moderate perinephric hematoma, moderate hydroureter and hydronephrosis. Triphasic CT scan and MRI, with contrast, of the abdomen and pelvis disclosed a case of ruptured benign cyst and ruled out renal cancer and vascular etiologies. The patient was treated conservatively and did not require renal embolization or nephrectomy. In conclusion; ruptured renal cysts is a rare cause for WS yet requires prompt management with patient’s stabilization and diagnostic approach. Contrary to the more common etiologies viz. tumors and vasculopathy; it rarely requires more than conservative treatment in stable patients.
Keywords: Cyst, rupture, CT, MRI, ultrasound, Wünderlich.
Introduction
Spontaneous, atraumatic, subcapsular and perirenal renal bleeding was first described by Bonet in 1700. Wünderlich defined it as “spontaneous apoplexy of the renal capsule” in 1856 and in 1910, Coenen referred to this condition as Wünderlich syndrome (WS) [1]. Subsequently, Lenk’s characterized it with a triad of acute flank pain (83%), hematuria (19%), and hypovolemic shock (11%) [2]. WS is a rare condition with a total of 165 cases has been reported by 2002 [3]. Its various etiologies include; (a) tumors viz. renal cell carcinoma, angiomyolipomata, metastases, sarcoma, fibroma, adenoma, oncocytoma and transitional cell carcinoma (61%), (b) vasculopathy viz. polyarteritis nodosa and renal artery aneurysms, renal vein thrombosis, renal arteriovenous malformations, fistulas and portal hypertension (17%), (c) infections viz. renal abscess, acute pyelonephritis, emphysematous pyelonephritis and Xanthogranulomatous pyelonephritis (12%), and “miscellaneous” viz. cystic renal diseases, calculus disease, lupus nephritis, coagulation disorders, nephrosclerosis, renal transplantation and preeclampsia (10%) [3]. Moreover, in another literature review, 5-10% of WS were idiopathic [4]. With WS, high index of suspicion is imperative since, excluding, overt hematuria, manifestations can be nonspecific. Moreover, since its etiologies are varied and include life-threating tumors, vasculopathy and infections, prompt management is essential to ensure; (a) patient’s hemodynamic stability (b) definite diagnosis, and (c) safe and effective treatment. Concurring with the latter, we describe our experience with management of a rare presentation of ruptured renal cyst presenting with such syndrome and simulating renal cancer.
Case Report
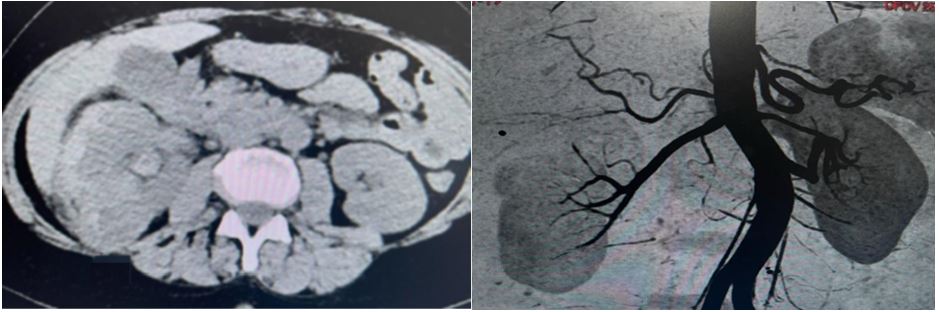
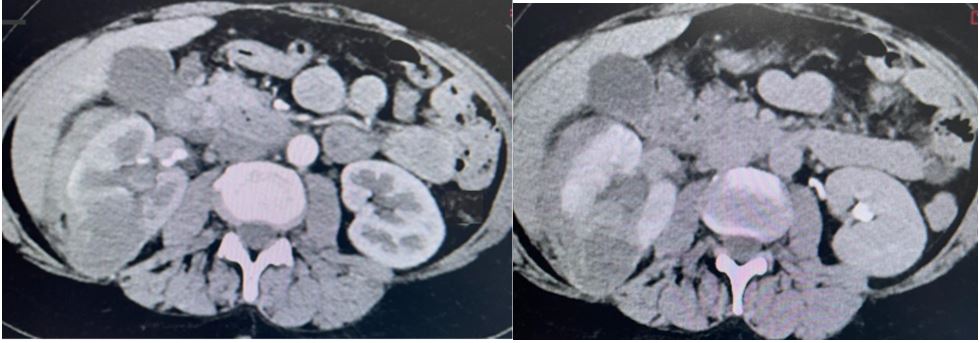
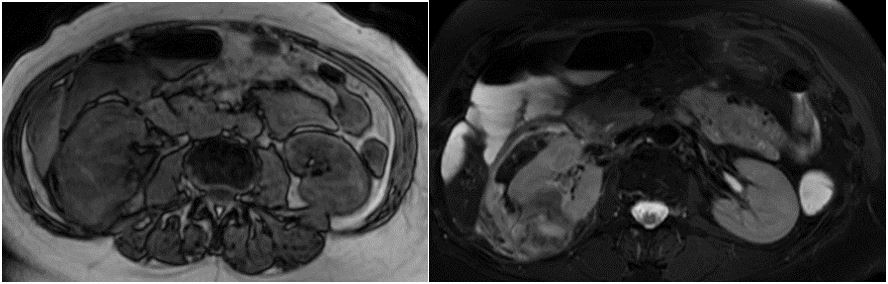
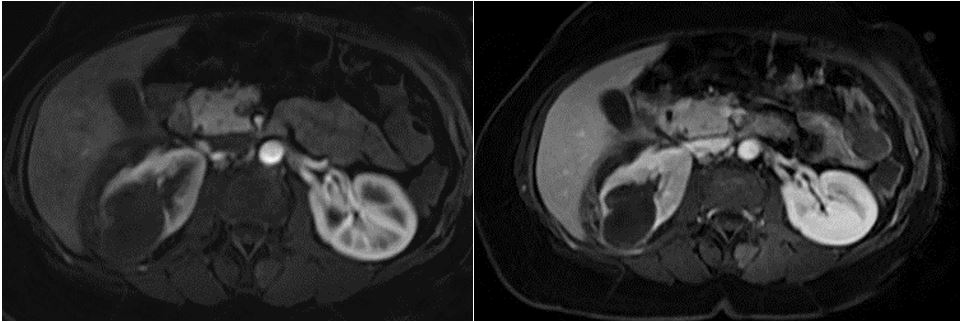
A 57-year-old woman presented with 6 weeks history of dull-aching right loin pain followed by severe hematuria weeks later. She did not have significant past history of medical illness, surgery, allergy or chronic intake of medications. On her initial assessment; her loin pain was, relatively, less yet she was having severe hematuria, for 1 weeks, that was associated with clot formation and urine retention. Her blood pressure was 90/60 mm Hg and she was afebrile with a body weight at 85 kg. She had pallor yet systemic examination did not show other abnormalities. Laboratory investigations showed normal peripheral leucocytic and platelets counts. Hemoglobin was 96 g/L with low MCV and transferrin saturation%. She had normal serum glucose, urea, creatinine, electrolytes as well as liver and lipid tests. Urine routine and microscopy was normal except for excess RBCs/HPF. ECG showed sinus tachycardia. Chest x-ray was normal. Abdominal and pelvic ultrasound (US) revealed lesions in the right kidney which were; (a) an ill-defined hyperechoic mass-like lesion measuring 4.6X4.1 cm at its upper pole which, on doppler study, had minimal internal vascularity, (b) moderate perinephric hematoma, moderate hydroureter and hydronephrosis (Fig.1). The urinary bladder had normal wall thickness yet was distended with mobile blood clots. Initially, she was treated with; (a) 3-way foley catheter placement in the urinary bladder and its irrigation with saline to dissolve its blood clots, and (b) transfusion of 2 units of packed RBCs, normal saline and intravenous iron. After hemodynamic stabilization; she was subjected to (triphasic CT scans and contrast-MRI) which; (a) excluded enhancing tumors (cancer and angiomyolipomata) and retroperitoneal lymphadenopathy/lesions, (b) confirmed the blood content of a cystic lesion, and (c) excluded vascular malformations in the renal arteries and veins (Fig.2-6). By 2 days of conservative therapy; hematuria abated and vital signs as well as hemoglobin level were stable.
Figure 1: The initial ultrasound examination of right kidney showing an upper pole ill-defined hyperechoic mass-like lesion (M) measuring 4.6X4.1 cm with partial cystic component (A) and a moderate perinephric hematoma (P) as well as moderate hydroureter and hydronephrosis few days later (B).
Figure 2: CT scan of the abdomen, without contrast, showing high-density fluid in dilated pelvicalyceal system (A) and normal right renal arteriogram except for the smooth focal cortical lesion (arrow).
Figure 3: CT scan with contrast showing normal left kidney yet the right has; (A) homogenous enhancement restricted to renal cortex and excluding enhancing tumors in the arterial phase and (B) persistent nephrogram indicating obstruction of pelvicalyceal system with blood clots in delayed post-contrast view.
Figure 4: MRI showing the right renal mass-like lesion (arrow) with heterogenous high signal intensity in T1W1 (A) and T2W1 (B) indicating its blood content.
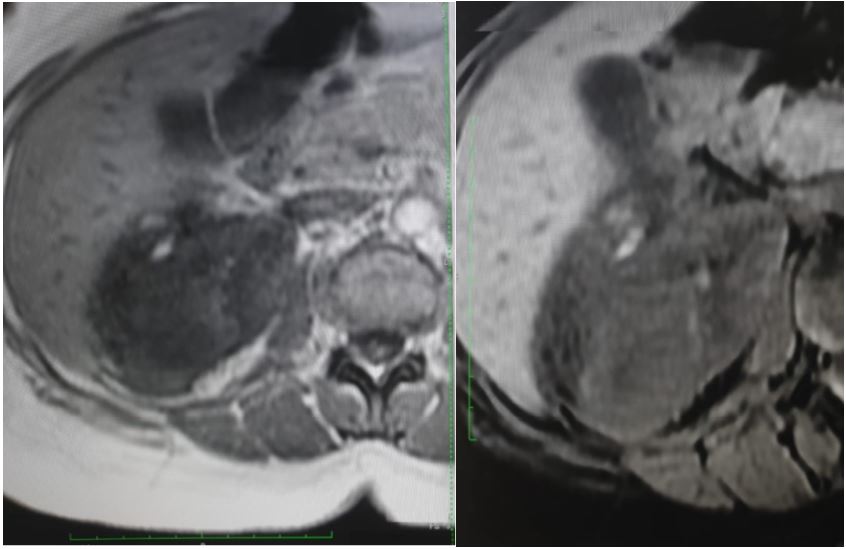
Figure 5: Post-contrast MRI in arterial (A) and venous (B) phases; showing high-signal intensity in T1 & T2 and T1 fat sat indicating its blood content and excluding fat-containing tumor (angiomyolipoma).
Figure 6: MRI (T1W view) showing absence of fat component inside the right kidney mass (A) and confirmed with T1 fat sat view (B) excluding angiomyolipoma.
Discussion
Urine-filled renal cysts are the most common space-occupying lesions of the kidney, with prevalence rate at 14% in young men up to 55% if >70 years yet 7 and 43% in female respective age groups [5]. They evolve, in the renal tubules secondary to intratubular obstruction and/or progressive diverticulization in the distal tubules [6]. Simple cysts are; (a) oval or circular-shaped, (b) with sharply defined outline and a smooth thin wall, (c) homogenously anechoic on US examination and avascular on doppler study, (d) with a radiodensity similar to water on CT density assessment (1 Hounsfield Unit). Simple cysts are generally asymptomatic, representing an incidental finding on abdominal examinations. Complications are rare yet include; misdiagnosis of hereditary/genetic forms, hemorrhage, infection and rupture (spontaneous or post-traumatic) [7]. Traumatic rupture has been reported following blunt trauma, extracorporeal lithotripsy and retrograde endoscopy [8]. On the other hand, spontaneous cyst rupture is extremely rare yet has been reported in benign cysts, autosomal dominant polycystic kidney disease and acquired cysts in dialysis patients [8-11]. Spontaneous rupture of simple renal-cysts has been reported in association with urinary tract obstruction, infection and nephrolithiasis [2]. However, the most common cause of idiopathic cyst rupture is hemorrhage within the cyst due to rupture of a sclerotic artery in its wall [11]. As in our case, stabilization of the patient is the initial priority followed by prompt establishment of the etiology of WS. The latter requires multi-modality approach [12]. The initial ultrasound examination may reveal a cystic mass suggestive of tumor with necrosis, as in our case, yet its lack of vascularity by doppler study is useful [13]. As step-by-step detailed in our patient; tri-phasic CT scan and/or contrast-MRI are 100% sensitive for hematomata and enhancement of tumors. Moreover, in case of acute hemorrhage there is an increase of the attenuation value of the intracystic content (70-90 Hounsfield Unit), then, as blood liquefies and organizes, the attenuation values tend to decrease. Angiography is indicated in suspected cases of; (a) active bleeders especially prior to embolization, (b) vasculitis, (c) aneurysms, and arteriovenous malformations, and venous thrombosis. Contrary to others, treatment of WS secondary to non-infected ruptured cysts is primarily conservative and rarely requires aggressive measures viz. embolization of bleeding of a large sclerotic arteriole, nephrorrhaphy, partial and total nephrectomy [14]. Such phenomenon is attributed to; (a) small cyst-wall arterioles and tamponade of bleeder/s after cyst collapse with perinephric hematoma and pelvicalyceal drainage. Rarely, drainage of large perinephric hematoma is indicated to prevent Page kidney. The latter may lead to future kidney loss and hypertension due to activation of renin-angiotensin-aldosterone system [15]. Finally, advocates for prevention of spontaneous renal cyst rupture have suggested routine percutaneous aspiration of cysts larger than 7.5 cm [15]. However, such procedure is usually followed by repeat fluid collection. Moreover, aspiration followed by intracystic alcohol or other sclerosing materials leads to significant kidney scarring that hinders subsequent radiological investigations for future ailment/s [16]. In conclusion; ruptured renal cyst is an underestimated etiology for WS. Since, its etiologies are varied and include life-threating tumors, vasculopathy and infections, prompt management is essential to ensure; (a) patient’s hemodynamic stability (b) definite diagnosis, and (c) safe and effective treatment.
Authors’ Contributions
Kamel El-Reshaid - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shaikha Al-Bader - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sayed HM Mohamad - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of Submission: The corresponding author is the guarantor of submission.
Source of Support: None
Consent Statement: Written informed consent was obtained from the patient for publication of this article.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Conflict of Interest: Authors declare no conflict of interest
References
- Bielso AE, Campodonico A, Molina R. Síndrome perirrenal espontáneo (síndrome de Wünderlich). Rev Urol. 1962; 2: 17.
- Qing Zhang, J., Fielding, J. R., & Zou, K. H. Etiology Of Spontaneous Perirenal Hemorrhage: A Meta-Analysis. J Urol. 2002; 167: 1593-1596.
- Zhang JQ, Fielding JR, Zou KH. Etiology of spontaneous perirenal hemorrhage: a meta-analysis. J Urol. 2002; 167: 1593-1596.
- Kim JW, Kim JY, Ahn ST, Park TY, Oh MM, et al. Spontaneous perirenal hemorrhage (Wunderlich syndrome): An analysis of 28 cases. Am J Emerg Med. 2019; 37: 45-47.
- Mensel B, Kühn JP, Kracht F, Völzke H, Lieb W, Dabers T, Lorbeer R. Prevalence of renal cysts and association with risk factors in a general population: an MRI-based study. Abdom Radiol (NY). 2018; 43: 3068-3074.
- Baert L, Steg A. On the pathogenesis of simple renal cysts in the adult. A microdissection study. Urol Res. 1977; 5: 103-108.
- Eknoyan G. A clinical view of simple and complex renal cysts. J Am Soc Nephrol. 2009; 20: 1874-1876.
- Papanicolaou N, Pfister RC, Yoder IC. Spontaneous and traumatic rupture of renal cysts: diagnosis and outcome. Radiology. 1986; 160: 99-103.
- Hammami M, Guirat A, Ksibi H, Azzaza M, Rekik N, Beyrouti MI. Intraperitoneal rupture of renal cyst in autosomal dominant polycystic kidney disease. N Am J Med Sci. 2010; 2: 238-240.
- Chen CS, Ahn H, Shin JH, Li HL, Kim JW, Ibrahim A, Chu HH. Renal artery embolization for spontaneous hemorrhage in patients with acquired cystic kidney disease: A 20-year single-center experience. Pak J Med Sci. 2021; 37: 1111-1117.
- Levine E, Grantham JJ, MacDougall ML. Spontaneous subcapsular and perinephric hemorrhage in end-stage kidney disease: clinical and CT findings. AJR. 1987; 148: 755-758.
- Katabathina VS, Katre R, Prasad SR, Surabhi VR, Shanbhogue AK, Sunnapwar A. Wunderlich syndrome: cross-sectional imaging review. J Comput Assist Tomogr. 2011; 35: 425-433.
- Silverman SG, Pedrosa I, Ellis JH, Hindman NM, Schieda N, et al. Bosniak classification of cystic renal masses, version 2019: an update proposal and needs assessment. Radiology, 2019; 292: 475-488.
- Petrone P, Perez-Calvo J, Brathwaite CEM, Islam S, Joseph DK. Traumatic kidney injuries: a systematic review and meta-analysis. Int J Surg. 2020; 74: 13-21.
- Haydar A, Bakri RS, Prime M, Goldsmith DJ. Page kidney--a review of the literature. J Nephrol. 2003; 16: 329-33.
- Sugianto R, Tirtayasa PMW, Samuel AG, Astriani MY, Panuntun MA. Spontaneous renal cyst rupture in a female patient: A case report. IJSCR. 2022; 98: 107614.