Case report - Volume 3 - Issue 4
An Unusual Presentation of Sarcoidosis Mimicking Metastatic Peritoneal Carcinomatosis: A Case Report and Review of the Literature
Lauren Scanlon*; Gary L. Goldberg; Jill Whyte
Department of Obstetrics and Gynecology, Zucker School of Medicine at Hofstra/Northwell.
Received Date : June 14, 2023
Accepted Date : July 12, 2023
Published Date: July 19, 2023
Copyright:© Lauren Scanlon 2023
*Corresponding Author : Lauren Scanlon, Department of Obstetrics and Gynecology, Zucker School of Medicine at Hofstra/Northwell.
Email: laurenscanlonmd@gmail.com
DOI: Doi.org/10.55920/2771-019X/1500
Introduction
Sarcoidosis is a multi-organ system autoimmune disorder characterized by the presence of non-caseating granuloma formation within one or more organ systems [1]. The majority of cases present with lung involvement, however 30-50% of cases have extra-pulmonary involvement at the time of clinical presentation [2]. These extra-pulmonary manifestations typically involve the skin, lymph nodes and eyes. Rarely sarcoid can manifest in the abdomen; however, this is typically noted in the liver and spleen [3]. Peritoneal sarcoidosis is a rare manifestation of the disease with less than 50 reported cases and it can rarely mimic ovarian or primary peritoneal carcinoma with elevated CA125 levels. There are 5 reported cases reported in the literature.
Case Report
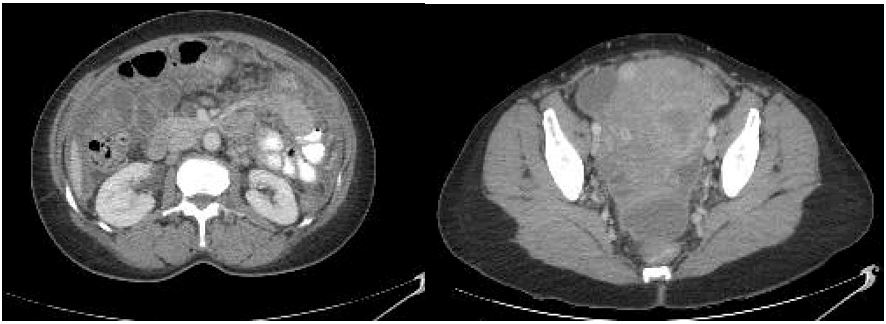
A 54-year-old peri-menopausal woman presented with recurring fevers and chills for 3 days. Prior to this hospital admission, the patient reported abdominal discomfort and constipation for 1 week. She also described increasing abdominal girth, however she was unsure of the duration. She also reported that she had persistent lower back pain and knee pain for approximately 2 years. She had been told in the past that she had uterine fibroids, but these had never been symptomatic. Upon examination she was noted to have significant abdominal distension with ascites and a 16-week size uterus with mild tenderness to palpation. She was noted to be febrile to 39C on admission and she continued to spike fevers >38C approximately every 12 hours throughout the majority of her hospitalization. A source of fever could not be identified and the WBC count was 5.7 without any shift. A Computed Tomography (CT) scan demonstrated moderate abdomino-pelvic ascites with enhancement of the peritoneal reflection and ill-defined areas of peritoneal nodularity. Omental thickening, likely representing omental caking was also noted. Retroperitoneal adenopathy with para-aortic, aorto-caval and cardio-phrenic lymph nodes noted to be enlarged. The uterus contained multiple heterogeneous enhancing lesions (Figure 1).
Figure 1: The uterus contained multiple heterogeneous enhancing lesions.
The initial CA125 was 568U/ml and the Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) were noted to be slightly elevated at 28 and 5.9 respectively. Of note, the Quantiferon Tuberculosis (TB)-gold was performed and was noted to be positive which raised suspicion for disseminated TB. However, no suspicious lung findings were noted on Chest X-Ray and 3 separate sputum cultures were negative. Subsequently a CT guided core biopsy and a FNA of the left retroperitoneal lymph node revealed lymphoid tissue with granulomas and no Acid Fast Bacilli (AFB) were identified. After discharge, an ultrasound guided core biopsy and Fine Needle Aspiration (FNA) of a peritoneal nodule in the right upper quadrant was negative for malignant cells and consistent with lymphoid tissue with granulomatous inflammation. AFB and GMS stains were again negative for organisms.
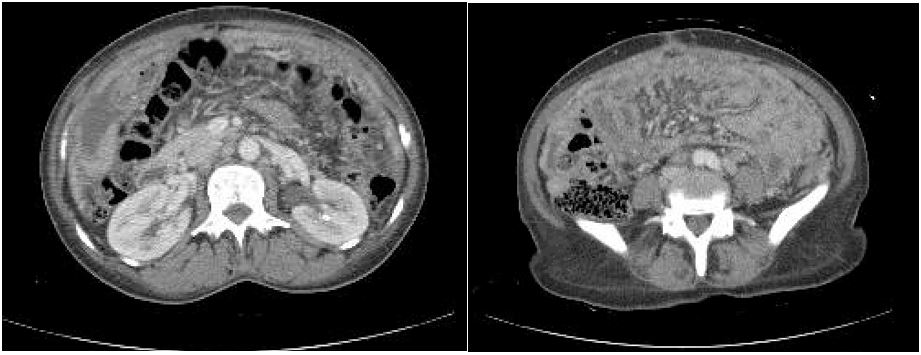
The patient was subsequently lost to follow up and was re-admitted to the hospital 4 months later. She was noted to have persistence of the constitutional symptoms and there was progression of disease noted on the repeat CT scan (Figure 2). There was an interval increase in the peritoneal disease with omental caking as well as increased retroperitoneal adenopathy and thickening of diaphragm. Her ESR and CRP were increasing to 77 and 27.9 respectively. The patient was also noted to have a serum ACE level of 99 (normal range 14-82). A repeat omental biopsy was performed with findings consistent with the prior histology.
Figure 2: Progression of disease noted on the repeat CT scan.
Discussion
Although the lung is the most common site of occurrence of sarcoidosis, it can present in numerous extra-pulmonary locations. The typical clinical presentation of fever, bilateral hilar lymphadenopathy, erythema nodosum and arthralgia may not be present in extra-pulmonary disease, which makes the diagnosis more difficult to ascertain. Peritoneal sarcoid may mimic neoplastic, infectious and other inflammatory diseases on imaging. Lymphoma, primary peritoneal cancer, metastatic ovarian cancer, tuberculosis, Whipple’s disease, actinomycosis, amyloidosis, fibromatosis or inflammatory pseudo-tumors and even endometriosis can be included in the differential diagnosis [4].
The diagnosis of sarcoidosis should be suspected based on clinical suspicion and laboratory tests, however, the definitive diagnosis can only be confirmed histologically. The presence of non-caseating granulomas is characteristic of sarcoidosis, although before making the diagnosis, other granulomatous diseases, especially TB, must be ruled-out [5].
It is exceedingly rare for sarcoidosis to present with peritoneal disease. Under these circumstances, the presence of ascites is noted in a majority of these cases. The ascites is typically an exudate supported by a SAAG <1.1 which indicates a peritoneal process, as noted in this case. This is unlike the ascites seen with more common presentations of sarcoid which are typically transudative processes caused by granulomatous obstruction of pulmonary or hepatic vasculature [6].
Elevated CA125 correlates with disease involving the peritoneum as peritoneal mesothelial cells are potent producers of CA125. This is postulated to be due to increased expression of pro-inflammatory cytokines, namely Interleukin-1b, Interferon-gamma and Vascular Endothelial Growth Factor in response to local insult [7]. While a significantly elevated CA125 often increases our suspicion for malignancy, other conditions should also be considered. An elevated CA125 can also be seen in many benign conditions including endometriosis, pelvic inflammatory disease, during menstruation and pregnancy and in numerous other inflammatory conditions such as SLE. In our review of the reported cases of peritoneal sarcoid, 5 of the cases had elevated CA125 at time of diagnosis [8].
Elevated serum ACE can point toward a diagnosis of sarcoid. ACE being produced by sarcoid granulomas can produce elevated serum Angiotensin Converting Enzyme (ACE) in approximately 60% of patients with sarcoidosis [6]. The elevated ACE levels in our patient in combination with the imaging and histological findings in the absence of tuberculosis lead to a final diagnosis of peritoneal sarcoidosis.
Interestingly there were no other cases reported where repeat imaging had been done in a short interval where such marked disease progression was noted. This again fostered the possibility of malignancy. The disease was appearing to spread rapidly and mimicking metastatic ovarian or primary peritoneal cancer. However, no evidence of malignancy could be found on histology.
Conclusion
The distinctiveness of this case is in the unusual and rare presentation of extra-pulmonary sarcoidosis and the rapid clinical progression of the disease which was a convincing imitation of a metastatic malignancy. In clinical practice it is important to address the diagnostic alternatives, like sarcoidosis, as imaging and laboratory tests may suggest malignancy; however, these can often be non-specific and definitive histology is imperative to the diagnosis and the optimal clinical management of these patients.
References
- Baughman RP. Lower EE, du Bois RM. Sarcoidosis. Lancet 2003; 361: 1111-8.
- Judson M. Extrapulmonary sarcoidosis. Semin Respir Crit Care Med. 2007; 28: 083-101.
- Thomas KW, Hunninghake GW. Sarcoidosis. JAMA 2003; 289(24):3300-3303.
- Lubner MG, Pickhardt PJ. Peritoneal sarcoidosis.the role of imaging in diagnosis. Gastroenterology & Hepatology. 2009; 5: 861-863.
- Newman LS, Rose CS, Maier LA. Sarcoidosis. N Engl J Med. 1997; 336: 1224-1234.
- Ebert EC, Kierson M, Hagspiel KD. Gastrointestinal and hepatic manifestations of sarcoidosis. American Journal of Gastroenterology. 2008; 103(12): 3184-3192.
- Zeimet AG, Marth C, Offner FA, et al. Human peritoneal mesothelial cells are more potent than ovarian cancer cells in producing tumor marker CA-125. Gynecologic Oncology. 1996; 62(3): 384-389
- Kalluri M, Judson MA. Sarcoidosis associated with an elevated serum CA 125 level: description of a case and a review of the literature. American Journal of the Medical Sciences. 2007; 334(6): 441-443.