Case report - Volume 3 - Issue 4
Gastro-gastric intussusception in the setting of unclear lead point: Radiological imaging
Ahmed Mahmoud1*; Ashok Katti2; Carlvin Luces3; Fouad Alaboud4
1Radiology registrar Royal Liverpool University Hospitals, UK.
2Consultant Radiology Royal Liverpool University Hospitals, UK.
3Consultant Gastroentrology Royal Liverpool University Hospitals, UK.
4GPST Royal Liverpool University Hospitals, UK
5Department of Anatomy, Medical School, National and Kapodistrian University of Athens, Greece
Received Date : June 19, 2023
Accepted Date : July 17, 2023
Published Date: July 24, 2023
Copyright:© Ahmed Mahmoud 2023
*Corresponding Author : Ahmed Mahmoud, Radiology registrar Royal Liverpool University Hospitals, UK. Tel: +447771238173,
Email: ahmedwogieh@gmail.com
DOI: Doi.org/10.55920/2771-019X/1505
Introduction
Intussusception is defined as telescoping or invagination of the proximal part of the gastrointestinal tract (intussusceptum) into an adjacent section (intussuscipiens) which results in obliteration of the lumen [1-2]. It is considered as a form of bowel obstruction as it accounts for only 1-5% of cases of bowel obstruction [3]. Intussusception in children can occur at any site in the GI tract, and it often presents similar clinical and radiographic features at all sites. These characteristic features are the key to diagnose intussusception even at unusual sites [4]. While Intussusception is a common diagnosis among children, it is in fact a rare condition in adults with the incidence of approximately 2-3 per 1,000,000 per year [5-6]. Adult intussusception is usually presented with vaguely unusual symptoms where the use of EUS and CT is extremely useful to aid in diagnosis [1-7]. Our case presents an even rarer type of Intussusception called Gastro-gastric Intussusception. According to multiple sources it consists of only 10% of the adult Intussusceptions [7-8].
Literature review
Clinical symptoms of adult intussusception are variable and often nonspecific. Patients could report vague abdominal pain, nausea, vomiting, change in bowel habits, and/or abdominal bloating. Clinical examination frequently does not show any abnormality other than mild abdominal tenderness or distension. These clinical findings can represent other more common conditions such as inflammatory bowel diseases, bowel obstruction due to peritoneal adhesions, and gastroenteritis. This makes the clinical diagnosis of Intussusception more challenging unless there is high index of suspicion [1-7]. In such case, the use of imaging studies like computed tomography (CT) would be required [7].
One of the most common radiological findings in adult intussusception is the presence of a lead point [1-7-8]. One of the famous gastro-gastric case reports with literature review is Behrooz et al published in 2018. In his literature review, Behrooz explained that there have been only 9 case reports of gastro-gastric intussusception documented from 1950 to 2017. Most cases were associated to gastric neoplasms which worked as lead points [7]. There were a few more case reports published afterwards. These reports described other possible causes of gastro-gastric intussusception in absence of clear lead points, such as ascites or hiatus hernia [9-10]. Another study published by Ghahremani et al describing the presence of sliding hiatus hernia in 12 patient cases involving esophago-gastric intussusception. A fundal mass surrounding the narrowed distal oesophagus was noted in the radiological imaging [11]. There is also a similar case presentation by Bowling where the Gastro-gastric AI was due to small intestinal obstruction rather than gastric neoplasm [9]. It is also noted that most published cases are between the age of 65 to 83 years old [7], where our case here is a 63-year-old female.
Case presentation
A 63-year-old lady presented to her GP with symptoms of acute epigastric pain, nausea, and reflux for multiple days. Her pain seems exacerbated with food. She reported that the epigastric pain was like when she had gallstones. Her GP diagnosed her with Gastritis, given appropriate advice with follow up. The patient then returned to the GP with worsening symptoms and unspecific weight loss recently which patient was not sure if it is related to poor appetite or not. The patient was referred under 2-week referral rule for suspected upper GI neoplasm. Her past medical history was cholecystectomy back in 2004.
As part of investigations, the patient had a gastroscopy which has shown a possible submucosal polyp of 50mm in size within the upper body of the stomach, some gastritis, normal oesophagus, and duodenum. Biopsies of the submucosal lesion were taken and have not shown any dysplasia pattern within the lesion. Endoscopic USS was performed which visualised the lesion as well and showed gastro-gastric intussusception without a focal lead point or any focal lesion. It was decided that the patient needed CT thorax& Abdomen& pelvis. CT showed evidence of moderate degree of gastro-gastric intussusception of the fundus of stomach into the body of stomach, about 6 cm, with a degree of mucosal hypertrophy of the fundus of stomach noted. There was no clear lead point detected. The CT also revealed small to moderate sized right diaphragmatic hernia. There was a 5.7 x 4mm/83mm³ subpleural nodule in right lung lower lobe. Multiple other 3mm sized scattered nodules were seen in both lungs which were indeterminate. No significant mediastinal or axillary lymphadenopathy was detected.
CT recommendations were to refer the patient to respiratory team and arrange a follow up CT chest. Respiratory MDT decided to do a follow up CT chest in 12 months. As for the upper GI team, it was decided that no intervention is needed at this stage; therefore, the patient was offered a rescope at interval in couple of months with biopsies as a follow up.
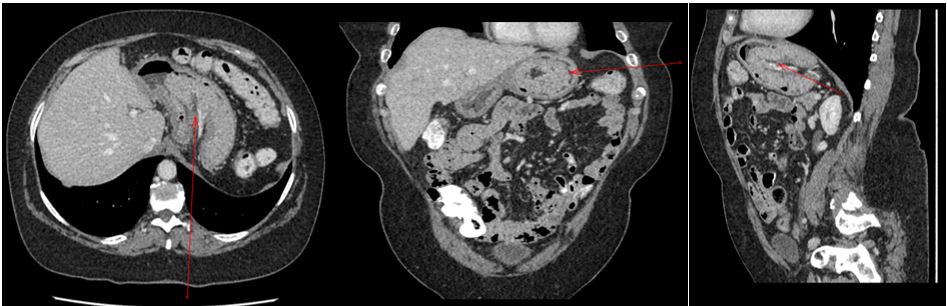
Figures: 1, 2 & 3 with axial, coronal and sagittal reformatted CT images show moderate degree of gastro-gastric intussusception of the fundus of stomach into the body of stomach with a degree of mucosal hypertrophy of the fundus of stomach. Bowel within bowel appearances with invagination of gastric mesentery within noted.
Endoscopic findings:
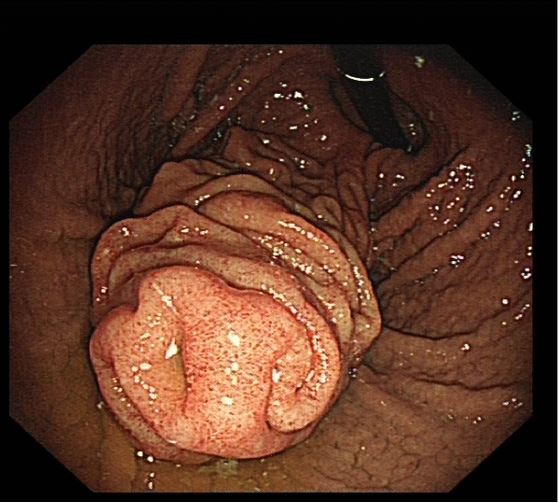
Figure 4: Gastroscopy showed possible submucosal polyp of 50mm in size within the upper body of the stomach.
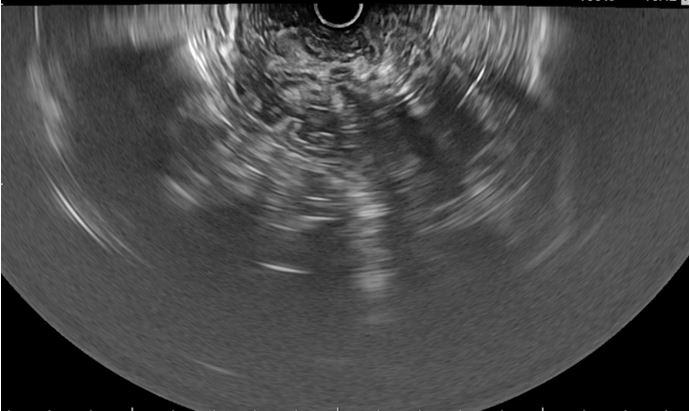
Figure 5: Endoscopic ultrasound images show hypertrophied gastric mucosa with no sinister mass lesion. EUS - biopsy did not show any evidence of dysplasia or malignancy on histology.
Case discussion
The use of CT is diagnostic and extremely useful in identifying lead points [7]. In our case EUS and CT aided in the diagnosis and ruling out the possibility of neoplasms. Adult intussusception is extremely rare and most cases if not surgically corrected will need a close follow up plan to prevent possible complications [9]. In the presence of gastro-gastric intussusception, a lead point should be excluded. The possibility of gastric malignancy should always be explored when a patient is found to have a gastro-gastric intussusception. However, there is no clear lead point. Behrooz et al proposed that in absence of a lead point, there could be ascites or hiatus hernia contributing to the AI [7]. In other words, Gastro-gastric intussusception could be caused by increased intra-abdominal pressure instead of a usual ‘lead point’. Our case supports this theory as it is thought that the hiatus hernia could be leading intra-abdominal pressure to be increased hence resulting in AI. Also, our patient’s age is 63 years old, which lies slightly outside the suggested age group. So, a high suspicion index is needed around that age group. In summary, when diagnosing Gastro-gastric intussusception and gastric neoplasms were excluded, other etiologies should be considered as well.
References
- Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009; 15(4): 407-11.
- Nkembe NM, Mbanga C, Agbor VN. Complicated Idiopathic Ileo-ileal Intussusception in a 45-year-old Male: A Case Report. Int J Case Rep. 2018: 2.
- Singh R, Bhatia C, Kaushik R, Singh S, Punia RS. Gastrogastric Intussusception Secondary to Gastrointestinal Stromal Tumour: a Case Report. SN Comprehensive Clinical Medicine. 2021; 3(2): 744-747. doi:10.1007/s42399-021-00767-w.
- Vikram R, McCulloch AS Zealley IA. True Gastrogastric Intussusception: A Rare Radiologic Diagnosis with Surgical Correlation. American Journal of Roentgenology. 2006; 186(2): 585-586. doi:10.2214/ajr.05.0115.
- Manouras A, Lagoudianakis EE, Dardamanis D, Tsekouras DK, Markogiannakis H, Genetzakis M, et al. Lipoma induced jejunojejunal intussusception. World J Gastroenterol. 2007; 13(26): 3641-4.
- Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J. 2005; 81(953): 174-7.
- Behrooz A, Cleasby M. Gastrogastric intussusception in adults: a case report with review of the literature. BJR | Case Reports. 2018; 4(4): 20180006.
- Lu T, Chng YM. Adult intussusception. Perm J. 2015; 19(1): 79-81
- Bowling JM, Landis PW, Herbener TE. Gastrogastric intussusception in the setting of a small bowel obstruction. Journal of the American College of Emergency Physicians Open. 2022; 3(2). doi:10.1002/emp2.12719.
- Caruso G, Caramma S, Zappalà A, et al. Acute intrathoracic gastric volvulus with retrograde gastric intussusception: A case report of a rare surgical emergency with review of the literature. Int J Surge Case Rep. 2020; 72: 381- 385.
- Ghahremani GG, Collins PA. Esophago-gastric invagination in patients with sliding hiatus hernia. Gastrointest Radiol. 1976; 1: 253-61. doi: 10.1007/BF02256375