Research Article - Volume 3 - Issue 4
Evaluation of results of anterior cervical discectomy and fusion by standalone peek cage for the treatment of double level cervical spondylotic myelopathy
Anowarul Islam1*; Wayez Mahbub2; Suvradev Saha2; Afia Ibnat Islam3
1Professor & Division Head of Spine Surgery, Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
2Resident, Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
3Resident, Holy Family & Red Crecent medical college & Hospital, Dhaka, Bangladesh.
Received Date : June 21, 2023
Accepted Date : July 18, 2023
Published Date: July 25, 2023
Copyright:© Anowarul Islam 2023
*Corresponding Author : Anowarul Islam, Professor & Division Head of Spine Surgery, Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
Email: maislam.spine@gmail.com
DOI: Doi.org/10.55920/2771-019X/1508
Abstract
Objective: To evaluate the results of Anterior Cervical Discectomy and Fusion by Stand-alone PEEK cage for the treatment of double level cervical spondylotic myelopathy.
Background: Cervical spondylotic myelopathy is a common cause of neck pain and radiating arm pain which develops when one or more of the intevertebral discs in the cervical spine start to degenerate. Anterior cervical discectomy and fusion (ACDF) is the gold standard treatment for degenerative cervical spine disease. Multiple techniques and modalities of fixation are used in ACDF, among them use of Stand-alone PEEK cage is standard one. To counteract the complications with the plating for ACDF, Stand-alone cage concept was constructed and favourable outcomes have been described with a low rate of dysphagia. Stand-alone PEEK cage provides immediate load bearing support to the anterior column and may facilitate fusion.
Materials & methods: This retrospective study was conducted in the spine unit of Orthopaedic Surgery department of Bangabandhu Sheikh Mujib Medical University, Shahbag and other private hospitals in Dhaka, Bangladesh from January 2016 to December 2021. A total number of 50 patients with cervical spondylotic myelolopathy with two level involvement confirmed by MRI were selected for the study who were failed to improve after conservative treatment. Outcome was evaluated by using visual analog score (VAS), Modified Odom`s criteria, Nurick’s grading and fusion rate by Bridwell’s criteria.
Results: Mean patient age was 48.4 ± 6.49 years. Male: female ratio 2:1. Pre-operatively, mean VAS score was 7.13±1.51 whereas post-operatively VAS score was decreased significantly to 0.47±0.64 after 12 months of follow up (p value <0.001). Neurological outcome was assessed by Nurick grading system, where all patients were in grade I (80%), grade II (14%) & grade III (6%) pre-operatively. Post-operatively at 12 months follow up, maximum patients (92%) were in grade 0 (p value <0.001). Radiological fusion was assessed by Bridwell fusion criteria, fusion was found in 80% and 90% of patients after 6 and 12 months follow up. Overall improvement was assessed by modified Odom’s score; excellent improvement was seen in majority patients after 12 months of post-operative follow up (86%)
Conclusion: ACDF by stand-alone PEEK cage is the preferred technique for the treatment of double level cervical spondylotic myelopathy with excellent functional outcome. This can be used with minimum risk as well as excellent fusion rate.
Keywords: Cervical spondylotic myelopathy, ACDF, standalone PEEK cage.
Introduction
Cervical spondylotic myelopathy (CSM) is a disorder of the spinal cord due to compression of the cord by degenerative disease depicted at radiological examinations [1]. Myelopathic or upper motor neuron lesion findings (e.g, hyper-reflexia and gait disturbance) are the typical manifestations of this disorder [2]. Patients may also present with radiculopathy due to degenerative process including bulging or tear of annulus, herniation of disc material into the canal causing pressure effect over the spinal cord and nerve roots [3]. Myelopathic hand signs, Grip release sign, Hoffman’s sign, Romberg test along with gait disturbances (broad based and hesitant) are common in advanced conditions. Changes in the pattern of bladder and bowel dysfunction are also found in about 20% -50% of the patients [4]. Surgical procedures performed in cervical myelopathy are aimed at relieving spinal cord compression, as well as achieving stabilization. Anterior cervical discectomy and fusion (ACDF) is the established gold standard treatment for degenerative cervical spine disease both for radiculopathy and for myelopathy [5]. Interbody fusion rate is about 92% by ACDF [6]. Various techniques for performing ACDF depending on surgeon preference are available. Cervical cages of different materials have been used like titanium, PEEK cage and carbon fiber [7]. ACDF with PEEK cage provides good functional outcome and fusion rate following surgery [8]. ACDF by stand-alone PEEK cage provides immediate load bearing support to the anterior column and may facilitate fusion and also has the advantage of mitigating the complications associated with anterior plating [9]. The aim of this study is to evaluate the results of ACDF by Stand-alone PEEK cage for the treatment of double level cervical spondylotic myelopathy.
Material and Methods
This retrospective study was conducted in the Spine division of Orthopaedic Surgery department of Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka from January 2016 to December 2021. A total number of 50 patients with cervical spondylotic myeloradiculopathy with two level involvement confirmed by MRI were selected for the study who were failed to improve after conservative treatment. Patients having involvement of one level, infection, tumor or fracture of vertebra were excluded from the study. Patients were followed up at 3 months, 6 months, 12 months and finally at 24 months. Outcome was measured by using visual analogue score (VAS) for pain, Nurick Grading for neurological status, Bridwell criteria for radiological fusion & finally overall improvement was evaluated by Modified Odom´s criteria. All the data were compiled and sorted properly and the quantitative data was analyzed statistically by using Statistical Package for Social Science (SPSS-26). P <0.001 was considered as the level of significance.
Surgical procedure
Patient was positioned in supine. The Gardener-wells tong traction was applied. A sandbag was placed in between shoulder blades to extend the neck. Patient’s head was rotated slightly to the opposite of the planned approach site. Transverse skin incisions were made over the targeted disc levels. The platysma muscle was identified and incised longitudinally. The esophagus was identified and retracted medially, while the sternocleidomastoid and underlying carotid sheath was retracted laterally. The pre-vertebral fascia was divided, and the longus colli musculature was further retracted. Intra-operative radiograph was obtained to confirm the appropriate cervical levels. The offending disc was removed with a rongeur. The entire disc, vertebral body endplates were decorticated. Stand-alone PEEK cages were inserted and fixed with screw in desired position after measuring with template.
Figure 1: Stand-alone PEEK cage.
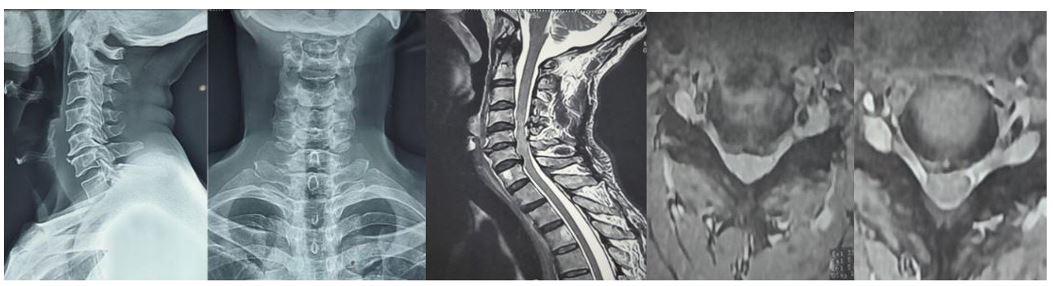
Figure 2: Pre-operative X-ray and MRI showing degenerative changes with herniated disc causing cord compression at C5/C6 and C6/C7 levels.
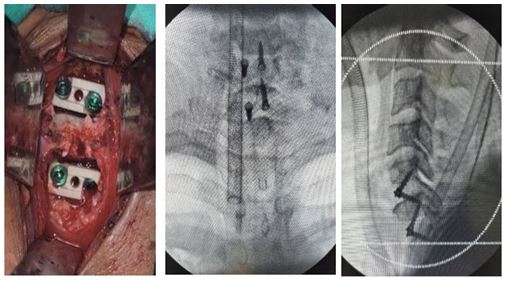
Figure 3: Per-operative picture and C-arm image showing double level stand-alone cages
Figure 4: X-ray cervical spine A-P and lateral view showing Stand-alone PEEK cages at C5/6, C6/7 level.
Results
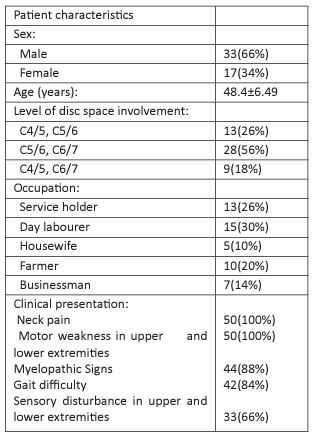
Mean patient age was 48.4 ± 6.49 years. Among them, 33 were men and 17 were women with a male: female ratio 2:1. Patient demographic characteristics are illustrated in Table I. C5-6, C6-7 were most commonly involved disc levels (56%), following in decreasing order C4/5, C5/6 (26%), C4/5, C6/5 (18%). All of the study patients had neck pain and motor weakness in upper and lower extremities. 44 patients (88%) had myelopathic signs and 42 patients (84%) had gait difficulty. Sensory changes in both extremities were seen in 33 patients (66%).
Table 1: Demographic characteristics of patients (n=50).
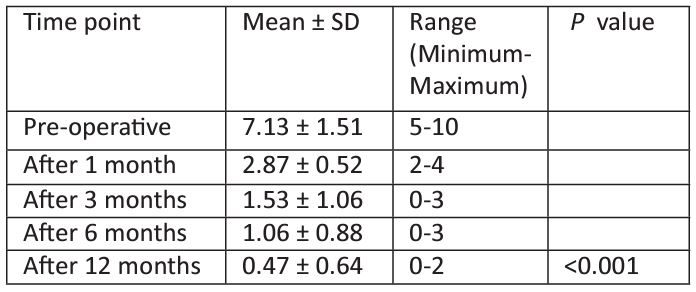
Table 2: Mean VAS score in all patients at different time points (n=50).
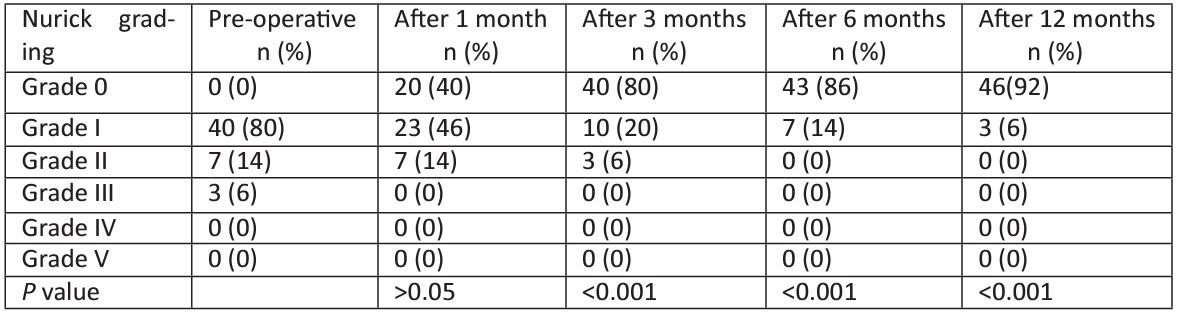
Table 3: Comparison of Nurick grading at different time points (n=50).
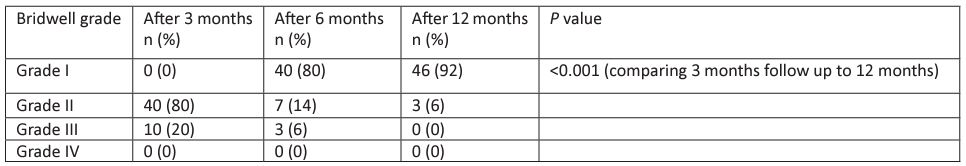
Table 4: Assessment according to Bridwell fusion criteria (n=50).
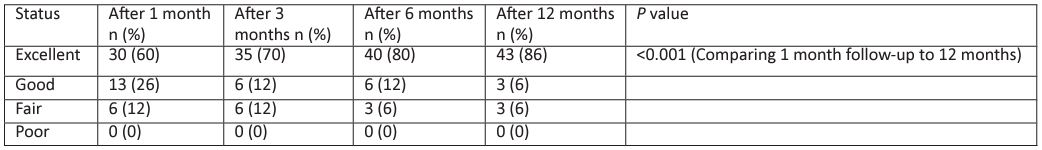
Table 5: Assessment according to modified Odom’s criteria (n=50).
Pre-operatively, mean VAS score of all patients was 7.13±1.51 (5-10) whereas post-operatively VAS score was decreased significantly after 6 and 12 months of follow up 1.06±0.88 and 0.47±0.64 respectively. (p value <0.001). Neurological outcome was assessed by Nurick grading system, where all patients were in grade I (80%), grade II (14%) & grade III (6%) pre-operatively. Post-operatively at 3, 6, 9 and 12 months follow up, maximum patients were in grade 0 (80%, 86% and 92% respectively) with significant difference compared to pre-operative status (p value <0.001). Radiological outcome was assessed by Bridwell fusion criteria, radiological fusion was found in majority of patients after 6 and 12 months follow up (80% and 92%, respectively) (p value <0.001). Overall improvement was assessed by modified Odom’s score, excellent improvement was seen in majority patients after 3, 6 and 12 months of post-operative follow up (70%, 80% and 86%, respectively) (p value <0.001). Perioperative complications were seen in 10 (20%) patients wherein 4 (8%) patients had transient paraparesis, 3 (6%) patients had transient dysphagia, 3 (6%) patients had dural injury. Average postoperative hospital stay was 3±1.2 days which was ranged 3-5 days.
Discussion
In this study, average age of all patient was 48.4 ± 6.49 years (ranging from 35-62 year) with majority belonged to 50-59 years of age (53.3%). Almost similar result was found by Moon et al. (2010) [10]. In this study, most of the patients were male (66%) with a male to female ratio was 2:1. Kim also found male to female ratio of 2:1 in their study (Kim et al. 2017) [11]. In present study, maximum patients were day labourer (30%) who have to carry heavy objects that may contribute to cervical disc prolapse which was also suggested by Kelsey et al. (1984) [12]. All of the study patients had neck pain and motor weakness in upper and lower extremities. 44 patients (88%) had myelopathic signs and 42 patients (84%) had gait difficulty. Sensory changes in both extremities were seen in 33 patients (66%). These are nearer to the study of Shiban et al. (2015) [13]. C5-6, C6-7 were most commonly involved disc levels (56%), following in decreasing order C4/5, C5/6 (26%), C4/5, C6/5 (18%). Quite similar result was observed by Moon et al. (2010) [10] and Topuz et al. (2009) [14] in two different studies.
In this study, mean preoperative VAS score was 7.13±1.51 (5-10) whereas post-operatively VAS score was decreased significantly after 1, 3, 6 and 12 months of follow up (2.87±0.52, 1.53±1.06, 1.06±0.88 and 0.47±0.64 respectively), which is statistically significant (P <0.001). Similar result was observed by Choi et al. (2016) [15]. According to Nurick grading system at 12 months of post-operative follow up, 46 patients (92%) were in grade 0 level and 3 patient (6%) in grade I level. Islam et al. (2020) [16] reported 90.6% in grade 0 level and 6 patients (9.4%) in grade I level in follow up according to Nurick grading in a study on 64 patients. According to Bridwell fusion grading system, radiological fusion (grade I) was found in majority patients after 6 and 12 months of follow up (80% and 92% respectively) which is similar to the study of Wang et al. (2013) [17]. Overall improvement was assessed by modified Odom’s score where postoperative outcome at 12 months follow-up demonstrated 86% patients had excellent outcome and 6% had good outcome. Almost similar result was found by Liao et al. (2008) [18]
Perioperative complications were seen in 10 patients (20%). 4 patients (8%) developed transient paraparesis who all improved within 6 months. 3 patients (6%) had transient dysphagia which resolved within 2 weeks. 3 patients (6%) had dural injury which was treated per operatively by application of gel foam and no further leakage of CSF postoperatively. No patient developed surgical site infection. Choi et al. (2016) [19] found smilar results. Postoperative average hospital stay was 3 ± 1.2 days (range: 3-5 days) in this study which was comparable to Niu et al. (2010) [20].
Conclusion
The use of a stand-alone PEEK cage in a 2-level cervical interbody fusion achieves satisfactory improvements in both clinical outcomes and fusion. So, it can be concluded that ACDF with standalone PEEK cage can be an ideal technique for the treatment of patients with double level cervical spondylotic myelopathy with excellent postoperative outcome and good fusion rate.
References
- Boogaarts HD, Bartels RH. Prevalence of cervical spondylotic myelopathy. European Spine Journal. 2015; 24(2): 139-141.
- Dillin WH. Clinical syndromes in cervical myelopathy. In: The Spine. 5th ed. Philadelphia: W.B. Saunders. 2006; 775-88.
- Baron EM, Young WF. Cervical spondylotic myelopathy: a brief review of its pathophysiology, clinical course and diagnosis. Neurosurgery. 2007; 60(1 Suppl 1): S35-S41.
- Abbed KM, Coumans JV. Cervical radiculopathy: pathophysiology, presentation and clinical evaluation. Neurosurgery. 2007; 60(Suppl 1): S28-S34
- Shiban E, Gapon K, Wostrack M, Meyer B, Lehmberg J. Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta neurochirurgica. 2016; 158(2): 349-355.
- Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011; 3: 16-23.
- Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, et al. Efficacy of anterior cervical fusion: Comparison of titanium cages, polyethere-therketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci. 2008; 15: 1240-1245.
- Islam MA, Hossain MA , Iqbal AA , Parvez MQ , Ahsanuzzaman M and Ahammed S. Anterior cervical discectomy and fusion with polyetherether ketone cages in the management of single and double level cervical spondylotic myelopathy-our experiences of 80 cases. KYAMC Journal. 2018; 9(1): 32-34
- Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clinics in Orthopedic Surgery. 2011; 3(1).
- Moon HJ, Kim JH, Kwon TH, Chung HS, Park YK. The effects of anterior cervical discectomy and fusion with stand-alone cages at two contiguous levels on cervical alignment and outcomes. Acta neurochirurgica. 2011; 153(3): 559-565.
- Kwon WK, Kim PS, Ahn SY, Song JY, Kim JH, Park YK, et al. Analysis of associating factors with C2-7 sagittal vertical axis after two-level anterior cervical fusion: comparison between plate augmentation and stand-alone cages. Spine. 2017; 42(5): 318-325.
- Kelsey JL, Githens PB, Walter SD, Southwick WO, Weil U, Holford TR, et al. An epidemiological study of acute prolapsed cervical intervertebral disc. The Journal of bone and joint surgery. American volume. 1984; 66(6): 907-914
- Shiban E, Gapon K, Wostrack M, Meyer B, Lehmberg J. Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta neurochirurgica. 2016; 158(2): 349-355.
- Topuz K, Colak A, Kaya S, Şimşek H, Kutlay M, Demircan MN, et al. Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up. European Spine Journal.12009; 8(2): 238-243.
- Choi MK, Kim SB, Park CK, Kim SM. Comparison of the clinical and radiologic outcomes obtained with single-versus two-level anterior cervical decompression and fusion using stand-alone PEEK cages filled with allograft. Acta neurochirurgica. 2016; 158(3): 481-487
- Islam MA, Shohidullah M, Mahbub W, Chowdhury AZ. Evaluation of Result of Anterior Cervical Discectomy and Fusion by Standalone PEEK cage in cervical Spondylotic Myeloradiculopathy.
- Wang HR, Li XL, Dong J, Yuan FL, Zhou, J. Skip-level anterior cervical discectomy and fusion with self-locking stand-alone PEEK cages for the treatment of 2 noncontiguous levels of cervical spondylosis. Clinical Spine Surgery. 2013; 26(7): E286-E292.
- Liao JC, Niu CC, Chen WJ, Chen LH. Polyetheretherketone (PEEK) cage filled with cancellous allograft in anterior cervical discectomy and fusion. International orthopaedics. 2008; 32(5): 643-648.
- Choi MK, Kim SB, Park CK, Kim SM. Comparison of the clinical and radiologic outcomes obtained with single-versus two-level anterior cervical decompression and fusion using stand-alone PEEK cages filled with allograft. Acta neurochirurgica. 2016; 158(3): 481-487.
- Niu CC, Liao JC, Chen WJ, Chen LH. Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. Clinical Spine Surgery. 2010; 23(5): 310-316.