Case Report - Volume 3 - Issue 4
Cerebellar Abscess- A rare case
Amit Kumar Pandey1; Rajib Chatterjee2; Pushparaj Moolya3
1Junior Resident, Department of Pediatrics, Rural medical college, Loni, Maharastra, India
2Professor, Department of Pediatrics, Rural medical college, Loni, Maharastra, India
3Neurosurgeon, Department of Surgery, Rural medical college, Loni, Maharastra, India.
Received Date : June 26, 2023
Accepted Date : July 20, 2023
Published Date: July 27, 2023
Copyright:© Amit Kumar Pandey 2023
*Corresponding Author : Amit Kumar Pandey, Junior Resident, Department of Pediatrics, Rural medical college, Loni, Maharastra, India.
Email: amit952.pandey@gmail.com
DOI: Doi.org/10.55920/2771-019X/1511
Abstract
Paediatric brain abscess is a rare disease with a high risk of morbidity and mortality. Brain abscess seems to occur most commonly in the age group of 4-10 years, with the least frequent sites being the cerebellum and brainstem. A cerebellar abscess is characterized by headache, nystagmus, ipsilateral ataxia, dysmetria, and vomiting [1]. Advanced diagnostic modalities such as MRI and CT scans and early administration of antimicrobial agents have drastically reduced the mortality and morbidity associated with brain abscesses.
Keywords: Cerebellar abscess, brain abscess, mastoiditis.
Introduction
The incidence of brain abscesses has been estimated at 0.3 to 1.3 per 100,000 people per year but can be considerably higher in certain risk groups, for example, immunocompromised patients [2]. The most common underlying etiology includes 30%-50% contiguous spread, 10% direct invasion due to trauma or surgery, 10% immunodeficiency, and 30% bacteremia [3,4]. Cerebellar brain abscesses account for 9%–28% of all brain abscesses, and 85%–99% of cases result from the contiguous spread of infection from an ipsilateral otogenic or sinus site [5]. Bacterial spread to the cerebellar region is either retrograde, spread through emissary veins draining the middle ear or sinuses or via direct spread from the site of osteomyelitis or osteitis [5].
Case report
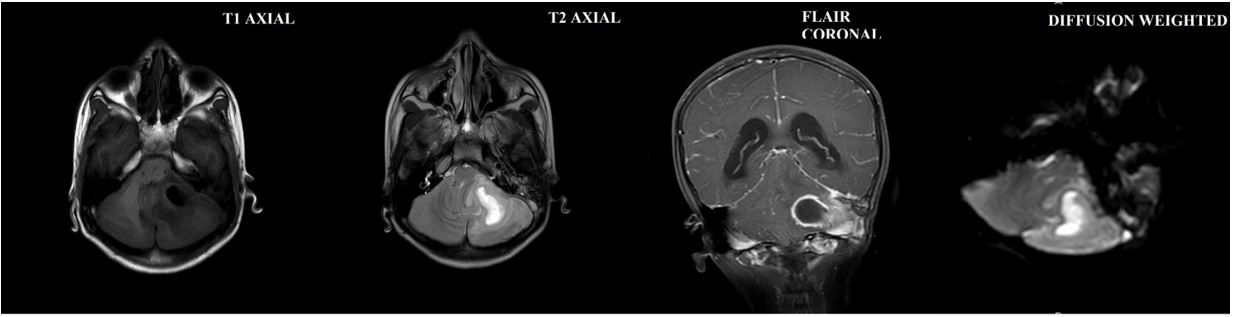
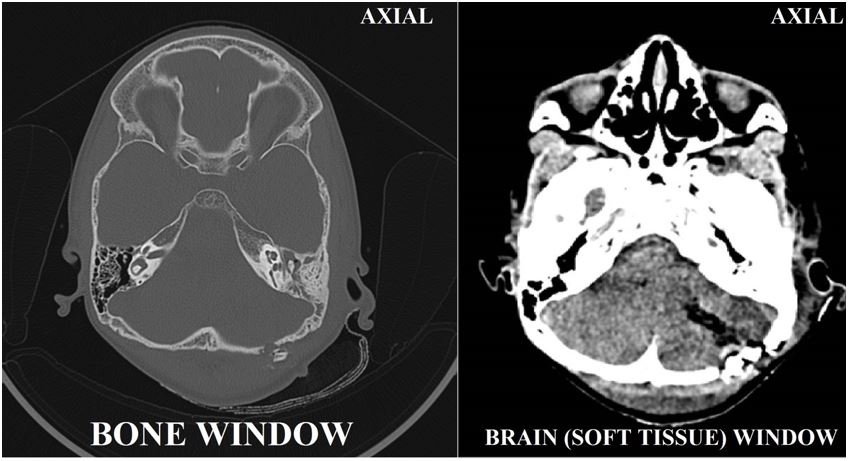
An 11-year-old boy, fourth by order born to nonconsanguineous parents, presented with discharge from the left ear, headache, fever for four days, and multiple episodes of vomiting for three days. He noticed ear discharge from the left ear while sleeping in the left lateral position, which was of intermittent flow with thick purulent consistency. This was associated with sudden onset high grade, intermittent, progressive fever, which was not associated with chills and rigor. He also complained of a throbbing headache that was sudden in onset and progressive, involving the whole left hemisphere of the skull, without any aggravating or relieving factor. He also complained of having experienced 2-3 episodes of vomiting for three days, which was nonprojectile, nonbilious, and nonblood stained. There was no history suggestive of seizure, trauma or foreign body impaction. He presented to the hospital in a drowsy state, with a Glassgow Coma Scale (GCS) score of 10 (E2V4M4), with positive meningeal signs along with altered sensorium. On ophthalmic evaluation, papilloedema grade I was seen, and hence, the patient was started on mannitol, IV fluids, antibiotics, steroids, and O2 support with propped up position. The 3T-MRI study was suggestive of left CSOM with mastoiditis with intracranial extension into the left cerebellar hemisphere measuring 3.9 x 2.6 x 3.6 cm (AP x TR x CC), approximately 18 cc. cm, along with acute lacunar infarct evident in the splenium of the corpus callosum on the right side with few ischemic foci noted involving subcortical and periventricular white matter in the bilateral parietal lobe. [figure 1] The patient was taken up for emergency craniotomy with left cerebellar abscess drainage under general anesthesia, after which the patient improved initially. However, later on, a postoperative CT scan revealed a 29 x 24x18 mm (AP X TR X CC) hypodense area approximately six cc.cm in size in the left cerebellar hemisphere with few hyperdense areas within, causing a mass effect in the form of compression over the vermis, inferior cerebellar peduncle, pons, and IVth ventricle. In addition, this mass effect caused upstream dilatation of both lateral ventricles and the IIIrd ventricle with minimal periventricular seepage suggestive of a (?) residual abscess. [figure 2]
Figure 1: 3T- Brain with contrast study suggestive of left CMOS with mastoiditis with intra carnialextension into left cerebellar hemisphere measuring 3.9x2.6x3.6cm (APxTRxCC) approximately 18.2cm³ along with acute lacunar infract evident in the splenium of corpus callosum on the right side with few ischemic foci noted involving subcortical and periventricular white matter in the bilateral parietal lobe.
Figure 2: HRCT Temporal bone scan axial images reveled hypodense collection in epitympanum, mesotympanum and hypotympanum on left side with obliteration of prussack’s space s/o chronic suppurative otitis media with mastoiditis with e/o 3.9x2.6x3.9cm (APxTRxCC) sized hypodense are noted in left cerebellar hemisphere with hyperdense areas within causing mass effect s/o ? residual abscess.
The cause for the abscess was otologic, and hence, a left modified radical mastoidectomy with atticotomy was planned. Postprocedure, no signs of facial nerve palsy, nystagmus, or soakage were seen. Once the cerebellar abscess diagnosis was obtained during the hospital stay, the patient was started on antibiotics (ceftriaxone, vancomycin, and metronidazole x 21 days). Antiepileptics (levetiracetam) were continued for 12-14 days along with dexamethasone and multivitamins. Once the injectable antibiotics were stopped, oral feropenem was started. The child had a full recovery with no neurological, ophthalmological, or auditory regression. Moreover, he was discharged on feropenem. On follow-up, no neurological deficit was seen, and follow-up MRI was advised, which was not done due to their poor financial status. Currently, the child has no neurological deficit and is performing well at school.
Discussion
Although two-thirds of brain abscesses in children are secondary to infections in the ear or paranasal sinuses, they are very rare complications of otitis media [6]. The classic clinical triad suggestive of brain abscess is fever, headache, and focal neurologic findings, which are more specific than sensitive, as only 20% of affected patients present with all three at the time of diagnosis. in the parietal/temporal region. [4] Overall, a complaint of headache is the most common symptom, ranging up to 60%, whereas fever in 50% and approximately 25% of patients presents with neurological findings such as seizures [4]. As the inflammatory process proceeds, vomiting, papilledema, seizures, hemiparesis, or even coma can develop. A cerebellar abscess is characterized byheadache, nystagmus, ipsilateral ataxia, dysmetria, and vomiting [7].
Brain MRI with contrast is the diagnostic test of choice in cases of brain abscess, whereas cranial CT scans can provide more rapid imaging but lack tissue detailing, which is seen in MRI [7]. Both MRI and CT scans with contrast demonstrate ring-enhancing lesions, whereas in CT scans, cerebritis findings are characterized by a parenchymal low-density lesion, whereas T2-weighted MRI images feature increased signal intensity. Approximately 60% of cases show leukocytosis, with 28% of cases having a culture-proven diagnosis [6,7]. Mostly normal CSF findings have been noted in cases of a cerebellar abscess, but it is avoided due to the risk of brain herniation.
Prompt diagnosis and initiation of antibiotic therapy is the key to a better prognosis of the case. Empirical antibiotic therapy should be administered with 3rd generation cephalosporin and metronidazole, often with vancomycin to cover MRSA and cephalosporin-resistant strains [7,8]. In cases where Listeria species are suspected, penicillin G or ampicillin with gentamycin is indicated, whereas antifungal coverage with amphotericin B should be provided in suspected cases of fungal infestation. Abscess aspiration is recommended in diagnostic culture and decompression unless contraindicated based on the location and patient’s condition. Small abscesses under 2.5 cm in diameter or multiple abscesses may be treated with antibiotics if drainage is contraindicated, with follow-up neuroimaging studies to ensure a decrease in abscess size [1,7,8].
Administration of glucocorticoids can reduce edema, although lack of evidence supporting its use is still in consideration. [8] Factors associated with a high mortality rate at admission included delayed administration of antimicrobial, age < 1year, multiple abscesses, and coma. Long-term sequelae occur in approximately 1/3rd of the survivors, including hemiparesis, seizure, hydrocephalus, cranial nerve abnormality, and behavioral & learning difficulties [7].
Conclusions
The morbidity and mortality associated with cerebellar abscess can be reduced by prompt diagnosis and initiation of antibiotic therapy. After initial medical management, radiological confirmation should be done and underlying etiology should be treated accordingly. Neurosurgical modalities should be discussed and if indicated, should be operated on as soon as possible for a better neurological outcome.
References
- Bokhari MR, Mesfin FB. Brain Abscess. [Updated 2021 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2021. PMID: 28722871.
- Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014; 82(9): 806-13. doi:10.1212/WNL.0000000000000172. Epub 2014 Jan 29. PMID: 24477107.
- Weinberg GA, Stone RT, Swaiman KF, Ashwal S, Ferriero DM, et al., eds. Swaiman’s Pediatric Neurology: Principles and Practice, 6th ed. Philadelphia, PA: Elsevier Saunders 2018; 883-894.
- Martinello RA, Cooney EL. Cerebellar brain abscess associated with tongue piercing. ClinInfect Dis. 2003; 36(2): e32-4. doi: 10.1086/345755. Epub 2003 Jan 3. PMID:12522766.
- Trimis G, Mostrou G, Lourida A, Prodromou F, Syriopoulou V, Theodoridou M. Petrositis and cerebellar abscess complicating chronic otitis media. J Paediatr Child Health. 2003; 39(8): 635-6. doi: 10.1046/j.1440-1754.2003.00251.x. PMID: 14629535.
- Janowski A and Hunstad D. Brain abscess. The Nervous System. In: Kliegman R et. Al, editor. Nelson textbook of pediatrics, 21st edition. volume 2. Elsevier; 2020; 622: 3235.
- Sheehan JP, Jane JA, Ray DK, Goodkin HP. Brain abscess in children. Neurosurg Focus. 2008; 24(6): E6. doi: 10.3171/FOC/2008/24/6/E6. PMID: 18518751.
- Mameli C, Genoni T, Madia C, Doneda C, Penagini F, Zuccotti G. Brain abscess in pediatric age: a review. Childs Nerv Syst. 2019; 35(7): 1117-1128. doi: 10.1007/s00381-019-04182-4. Epub 2019 May 6. PMID: 31062139