Case Report - Volume 3 - Issue 4
Solitary pityriasis versicolor: an uncommon presentation as a large single patch: Report of three cases and review of unusual clinical forms
Emilio Sudy; Francisco Urbina*
Dermatologist in private practice, Santiago de Chile, Chile.
Received Date : June 26, 2023
Accepted Date : July 20, 2023
Published Date: July 27, 2023
Copyright:© Francisco Urbina 2023
*Corresponding Author : Francisco Urbina, Dermatologist in private practice, Santiago de Chile, Chile.
Email: fcourbina@hotmail.com
DOI: Doi.org/10.55920/2771-019X/1512
Abstract
Pityriasis versicolor (PV) is a common disease, easy recognizable, that usually affects the trunk and upper limbs with multiple rounded scaly lesions which can vary in color from case to case. However, infrequent localizations have been reported, as well as diverse unusual clinical presentations, including atrophic, hyperkeratotic, annular, or inverse forms, among other. We describe 3 cases presenting with a single large lesion in the neck, which can hinder the diagnosis. No description of this form was found neither in large series of PV, nor in extensive reviews. This solitary variety would be just another atypical clinical presentation of PV. Clinicians should be aware of this variety in order to avoid unnecessary studies.
Keywords: Pityriasis versicolor, Tinea versicolor, Malassezia furfur
Introduction
Pityriasis versicolor (PV) is a very common disease in daily practice and it is almost always easily diagnosed by any dermatologist, without the need for further laboratory analysis. However, in the last 10 years we have seen 3 cases of PV with an infrequent presentation, characterized by a single and large lesion located in the neck in all of them, which could hinder the diagnosis. No description of this form was found neither in large series of PV, nor in extensive reviews.
Case report
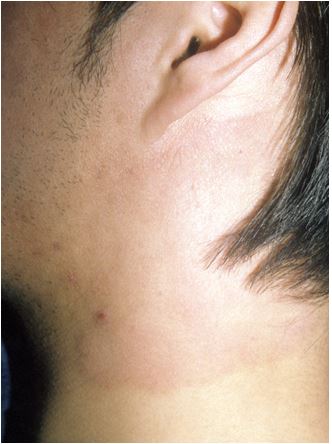
Case 1: A 19-year-old woman in treatment with hydroxyurea for the last 18 months for essential thrombocythemia since birth, presented with an itchy lesion of two and a half months located on the left side of the neck. It consisted of of a slightly erythematous, scaly patch with irregular margins, about 7-9 cm in size (Figure 1). No similar lesions were found on the trunk or elsewhere. She had been initially treated with creams containing clotrimazole with betamethasone, or fusidic acid, with partial improvement, but returning to its initial state when the treatment was stopped. Direct mycological examination revealed yeasts in small amount and the culture yielded Malassezia sp. Oral itraconazole 100 mg/day for 15 days and ketoconazole shampoo were then prescribed. The patient did not return to control.
Figure 1: Solitary erythematous scaly patch on the neck.
Figure 2: Isolated, erythematous scaly patch on the neck.
Case 2: A 24-year-old male similarly presented with a large erythematous scaly patch, also located on the left side of his neck, which had appeared six months earlier during summer time (Figure 2). No other lesions were detected. Direct microscopic examination showed numerous spores and short pseudomycelial filaments, and the culture yielded Malassezia furfur. The lesion improved completely after treatment with oral itraconazole 200 mg daily for one week. A year before, the lesion reappeared with identical characteristics in the same place. No predisposing factors were obtained after thorough questioning, including the use of high-necked garments, neckerchiefs, scarves, or headphones. He was treated again in the same way, and permanent weekly ketoconazol shampooing was recomended.
Case 3: A young male with an hypopigmented scaly patch on the right side of the neck (Figure 3) was also included in this report, although he was seen only once and did not return to control. Despite the fact that the diagnosis was not confirmed with a mycological study in this case, we decided to include it, as a counterpart to the preceding cases with erythematous scaly lesions, this time presenting rather with a hypopigmented, polycyclic, desquamative patch, that fully met the characteristic clinical and diagnostic features of PV, although as a solitary lesion.
Figure 3: Solitary polycyclic hypopigmented scaly patch on the neck.
Discussion
PV occurs most often in young and healthy people, predominantly affecting the seborrheic areas of the trunk. It is favored by basal conditions of hyperhidrosis, seborrhea, tropical climates and habitual dressing with synthetic or occlusive undergarments. Clinically, in its usual form, it presents with multiple thin, irregular, isolated and/or confluent rounded scaly lesions with varying colors from patient to patient, ranging from hypopigmented to different hues of tan, light brown or pink. In typical cases the trunk is mainly affected, although involvement of unusual locations has been reported, including the scalp [1,2,3], eyelids [4,5], face [6] –although it is a common localization in children [7]-, axillae and groins [8,9], pubis [9], perineum [10], perianal, buttocks [11], popliteal [8,9] and antecubital fossae [2,9], web space [12], legs and arms [8], forearms [12], palms [13], nipple and areola [11,14,15], vulva [16], shaft of the penis [11,12,17,18,19], and glans [8,20,21]. It is not clear if there are specific predisposing or etiologic factors acting in the development of PV in those unusual locations [8]. Moreover, not always this nonclassical distribution of lesions occurs in conjunction with the typical eruption of PV, sometimes appearing as an isolated manifestation of it [8].
Some infrequent and quite different clinical presentations have also been described, including a follicular form [22,23], inverse [10] –also called tinea inversicolor [24]- and many others, such as erythematous or rubra [11], atrophic [11,25] –induced by topical corticosteroid application [26], as an idiosyncratic response to Malassezia [27] or a delayed type of hypersensitivity reaction to its epicutaneous antigens [28]-, erythrasmoid [29,30], rotundiform [31], hyperkeratotic [32,33], confetti-like [34] and annular variants [35]; in one report, both hyperpigmented and hypopigmented lesions were detected, with different response to therapy [36].
In large series of patients we have not found mentions of this variety, presenting as a large single patch, not either in extensive reviews of PV [21]. However, as single reports, we have encountered eight well documented examples in the English and Spanish literature, with isolated solitary lesions exclusively affecting the areolar and periareolar area [14], medial thighs [35], popliteal fossae [37], interdigital space, penile shaft [12], antecubital fossae [12], submammary region [38], and neck [39].
Although it is not uncommon in daily practice to observe large lesions of PV formed by the confluence of individual polycyclic patches, they usually retain small areas of intermingled and unaffected skin [38], or satellital rounded lesions in close proximity, a fact that did not occur in our patients, devoid of other lesions.
A rather different condition is perhaps that of rotundiform PV, in which a small, perfectly rounded, hypopigmented, scaly lesion appears as an early first episode of PV, analogous to the herald patch of pityriasis rosea [31]. We ignore the origin of this unique, unilateral and solitary presentation, similarly affecting the neck in the three cases, and neither what caused the reappearance of the same lesion in the same place a year after in our second case (although recurrent episodes of PV are common). We can only mention that it would be important to keep in mind the possibility of solitary PV in the presence of a tenuous, erythematous or hypopigmented, desquamative patch, albeit solitary.
Conclusions
This solitary variety would be just another atypical clinical presentation of PV. Its recognition would be helpful in order to avoid unnecessary biopsies.
References
- Rice JS. Tinea versicolor confined to the hairy scalp. Arch Dermatol. 1963; 87: 643.
- El-Gothamy Z, Ghozzi M. Tinea versicolor of the scalp. Int J Dermatol. 1995; 34(8): 533-534.
- Padilha-Gonçalves A. Unusual locations of pityriasis versicolor with particular reference to scalp lesions. Dermatologia Tropica. 1963; 2: 211-216.
- Huang WW, Tharp MD. A case of tinea versicolor of the eyelids. Pediatr Dermatol. 2013; 30(6): e242-e243.
- Derbel M, Benzina Z, Ghorbel I, Abdelmoula S, Makni F, et al. Blépharite mycosique à Malassezia: à propos d’un cas. J Fr Ophtalmol. 2005; 28(8): 862-865.
- Terragni L, Lasagni A, Oriani A. Pityriasis versicolor of the face. Mycoses. 1991; 34: 345-347.
- Terragni L, Lasagni A, Oriani A, Gelmetti C. Pityriasis versicolor in the pediatric age. Pediatric Dermatology. 1991; 8(1): 9-12.
- Varada S, Dabade T, Loo DS. Uncommon presentations of tinea versicolor. Dermatol Pract Concept. 2014; 4(3): 21.
- Aljabre SHM. Intertriginous lesions in pityriasis versicolor. J Eur Acad Dermatol Venereol. 2003; 17(6): 659-62.
- Rudolph RI, Holzwanger JM. Inverse tinea versicolor. Arch Dermatol. 1975; 111: 1213.
- Romano C. Uncommon cases of pityriasis versicolor. Parassitologia. 2008; 50: 93-95
- Kaur I, Handa S, Kumar B. Tinea versicolor: involvement of unusual sites. Int J Dermatol. 1996; 35: 604-5.
- Kamalam A, Thambiah AS. A study of 3891 cases of mycoses in the tropics. Sabouraudia. 1976; 14: 129-148.
- Anthony JL, Schosser RH, Gross DJ. Unilateral areolar and periareolar tinea versicolor. Int J Dermatol. 1991; 30: 600.
- Sardy M, Korting HC, Ruzicka T, Wolff H. Bilateral areolar and periareolar pityriasis versicolor. JDDG 2010; 8: 617-618.
- Day T, Scurry J. Vulvar pityriasis versicolor in an immunocompetent woman. J Low Genit Tract Dis 2014; 18(3): e71-3.
- Ryu H-W, Cho J-W, Lee K-S. Pityriasis versicolor on penile shaft in a renal transplant recipient. Ann Dermatol 2012; 24(3): 345-347.
- Smith EL. Pityriasis versicolor of the penis. Br J Vener Dis 1978; 54: 441.
- Blumenthal HL. Tinea versicolor of penis. Arch Dermatol 1971; 103: 461-462.
- Nia AK, Smith EL. Pityriasis versicolor of the glans penis. Br J Vener Dis 1979; 75: 230.
- Leung AKC, Barankin B, Lam JM, Leong KG, Hon KL. Tinea versicolor: An updated review. Drugs Context 2022; 11: 2022-9-2.
- Hudson A, Carroll B, Kim SJ. Folliculocentric tinea versicolor. Dermatol Online J 2017; 23(2): 6.
- Nabatian AS, Millet CR, Heymann WR. Folliculocentric tinea versicolor. Cutis 2012; 90: 113, 117-118.
- Ferry M, Shedlofsky L, Newman A, Mengesha Y, Blumetti B. Tinea inversicolor: A rare distribution of a common eruption. Cureus 12(1): e6689.
- Allegue F, Fachal C, González-Vilas D, Zulaica A. Atrophying pityriasis versicolor. Actas Dermosifiliogr 2018; 109: 455-457.
- Tatnall FM, Rycroft RJG. Pityriasis versicolor with cutaneous atrophy induced by topical steroid application. Clin Exp Dermatol 1985; 10: 258-261.
- Levy JMS, Magro C. Atrophying pityriasis versicolor as an idiosyncratic T cell-mediated response to Malasezzia: A case series. J Am Acad Dermatol 2017; 76(4): 730-735.
- Crowson AN, Magro CM. Atrophying tinea versicolor: A clinical and histological study of 12 patients. Int J Dermatol 2003; 42: 928-932.
- Cinelli E, Vastarella M, Fabbrocini G, Gallo L. Erythrasmoid pityriasis versicolor with exclusive involvement of the pubis and inguinal region. Ital J Dermatol Venereol 2021; 156(Suppl 1 to Nº 6): 11-12.
- Gorani A, Oriani A, Falconi Klein E, Veraldi S. Case report. Erythrasmoid pityriasis versicolor. Mycoses 2001; 44(11-12): 516-517.
- Zawar V, Chuh A, Sankalecha S. Rotundiform morphology during the first episode of pityriasis versicolor-a retrospective case-control study on a distinct clinical presentation. J Dermatol case report 2007; Dec 29; 1(1): 10-5.
- Boralevi F, Marco-Bonnet J, Lepreux S, Buzenet C, Couprie B, et al. Hyperkeratotic head and neck Malassezia dermatosis. Dermatology 2006; 212: 36-40.
- Okuda C, Ito M, Naka W, Nishikawa T, Tanuma H, Kume H, Hotchi M, Midgley G. Pityriasis versicolor with a unique clinical appearance. Medical Mycology 1998; 36: 331-344.
- Baz K, Kokturk A, Kaya TI, Ikizoglu G, Yazici AC, et al. Confetti-like pityriasis versicolor. J Eur Acad Dermatol Venereol 2004; 18(2): 240-241.
- Kapadia F, Kharkar V, Vishwanath T. Dermoscopy to the rescue in an annular enigma: A rare case of annular pityriasis versicolor presenting in an unusual location. Dermatol Pract concept 2022; 12(2): e2022057.
- Acharya R, Gyawalee M. Uncommon presentation of pityriasis versicolor; hyper and hypopigmentation in the same patient with variable treatment response. Our Dermatol Online 2017; 8(1): 43-45.
- Kumar B, Kaur I, Kaur S. Pityriasis versicolor –an analysis of 175 patients. Ind J Dermatol Venereol Leprol 1984; 50: 101-105.
- Rodríguez-Díaz E, González Morán A. Placa pigmentada descamativa inframamaria. Piel 1996; 11: 379-81.
- Quinteros P, Urbina F, Sazunic I. Pitiriasis versicolor en placa única. Rev Chilena Dermatol 2001; 17: 303-5.