Review Article - Volume 3 - Issue 4
Discharge education and sepsis re-admission: An integrative review
Prasuna Thomas*
Johns Hopkins School of Nursing, Johns Hopkins University, USA.
Received Date : June 13, 2023
Accepted Date : July 26, 2023
Published Date: Aug 02, 2023
Copyright: © Prasuna Thomas 2023
*Corresponding Author : Prasuna Thomas, Johns Hopkins, School of Nursing, Johns Hopkins University, 525 N, Wolfe Street, Baltimore, Maryland, 21205, USA.
Email: prasunathomas@gmail.com
DOI: Doi.org/10.55920/2771-019X/1517
Abstract
Introduction: Hospital readmission has long been a threat to our country’s healthcare system. Sepsis has recently become the number one disease condition resulting in readmissions following an initial inpatient hospital discharge. Increase in the number of sepsis survivors causes a huge burden to the healthcare system secondary to increased morbidity, mortality, utilization of health care resources, and transition to hospice. This integrative review explored the existing literature on the effect of post sepsis care education on reducing all cause readmission among sepsis survivors.
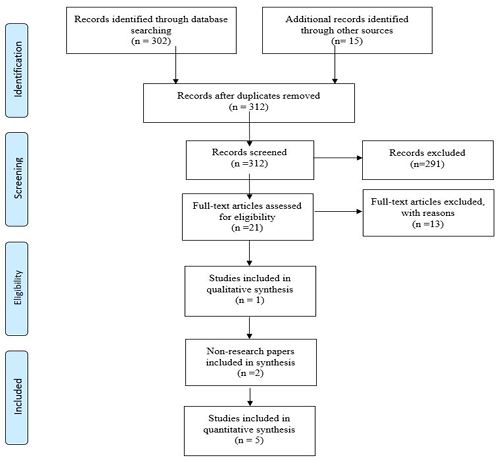
Methods: Pubmed, CINHAL, Cochrane, and Embase were used to survey the literature. The Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) flow chart was used to organize the search strategy and results.
Results: The results of this review suggest that hospitalization characteristics, in particular discharge education could be modified and targeted towards preventing readmissions following sepsis hospitalization. The sepsis discharge education needs to entail the signs and symptoms of infection, and significance of monitoring comorbidities, attending follow up visits, and peer support groups.
Keywords: Sepsis; Hospital readmission; Patient discharge education.
Introduction
Hospital readmission has long been a threat to our country’s healthcare system. Acute myocardial infarction, heart failure, chronic obstructive pulmonary disease, and pneumonia were the primary disease conditions which were closely tracked by the CMS for readmission [1]. Sepsis has recently become the number one disease condition resulting in readmissions following an initial inpatient hospital discharge [1]. Out of 49 million people who are hospitalized with sepsis worldwide, 38 million survive (World Health Organization) [2]. Mortality associated with sepsis has declined over the past few decades resulting in large number of sepsis survivors with chronic comorbidities and new symptoms requiring medical care which eventually contributes to hospital readmissions [3].
According to the 2013 nationwide readmission database, the readmission rate following an index sepsis hospitalization was higher compared to that for AMI, Heart Failure, COPD, and Pneumonia [1]. Increase in the number of sepsis survivors causes a huge burden to the healthcare system secondary to increased morbidity, mortality, utilization of health care resources, and transition to hospice [4,5]. The annual costs associated with sepsis readmission in the U.S healthcare system is estimated to be $17.4 billion among Medicare recipients alone [6].
Given the vicious consequences associated with rehospitalizations, acquiring evidence to guide strategies to prevent rehospitalizations among adult sepsis survivors from the inpatient units is of foremost importance. Education on post sepsis care and the risk for readmission would be an ideal approach in preventing readmissions. Despite sepsis readmissions being potentially preventable, no standardized educational material on post sepsis care currently exists. This integrative review explored the existing literature on the effect of post sepsis care education on reducing all cause readmission among sepsis survivors.
Methods
This integrative review was guided by the question “What are the best practices for discharge education on post sepsis care among the hospitalized patients with an index hospitalization diagnosis of sepsis?”. The following electronic databases were used to survey the literature: Pubmed, CINHAL, Cochrane, and Embase. The search was performed on September 12, 2019. No restrictions were applied in order to get an extensive overview of published literature. The search strategy included the key words: Sepsis [Mesh] OR Bacteremia [Mesh] OR Fungemia [Mesh] OR "Shock, Septic"[Mesh] OR sepsis OR septic OR severe sepsis OR septic shock OR septicemia OR urosepsis AND Patient Readmission [Mesh] OR readmit* OR readmission* OR rehospital* OR hospital readmission AND patient discharge[Mesh] OR patient discharge education OR patient education OR hospital discharge OR discharge planning OR aftercare.
The Preferred Reporting Items for Systematic Reviews and Meta- analyses (PRISMA) flow chart was used to organize the search strategy and results (Figure 1). Initially, 302 articles were obtained by searching the databases. An additional 13 articles were obtained by screening the reference list for similar articles. After removal of duplicates 310 articles remained for review. An additional 291 articles were excluded by screening the titles and abstracts for criteria relevant to the practice question. Remaining 19 full text articles were reviewed for eligibility in final analysis based on exclusion criteria including publication date before 2000 and language other than English. Inclusion criteria of study population of hospitalized patients with an index sepsis admission and discharge process with all-cause unplanned readmission was also used. Finally, 13 articles were excluded with the above reasons, and 6 articles were retained for evaluation and appraisal based on the Johns Hopkins Nursing Evidence-Based Practice Model, and analysis for review [7].
Results
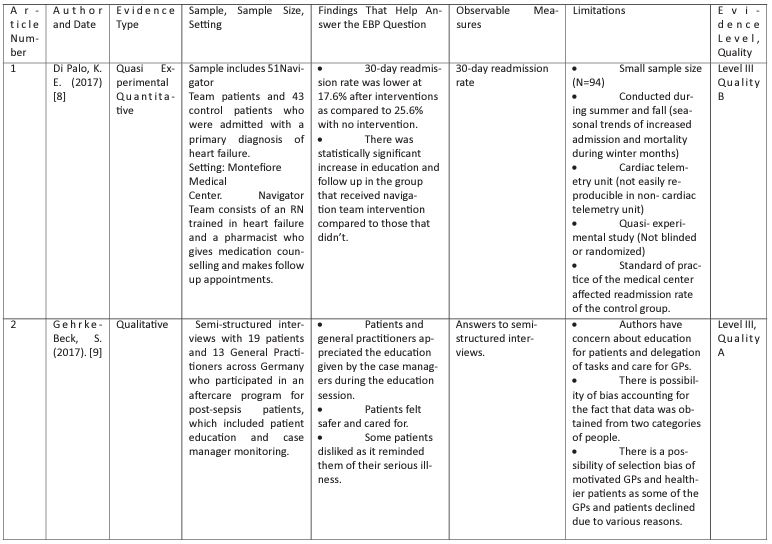
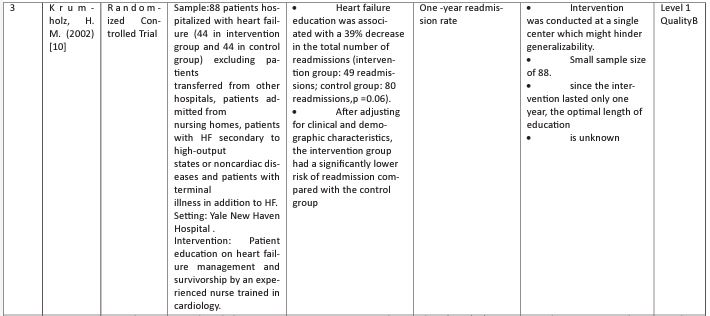
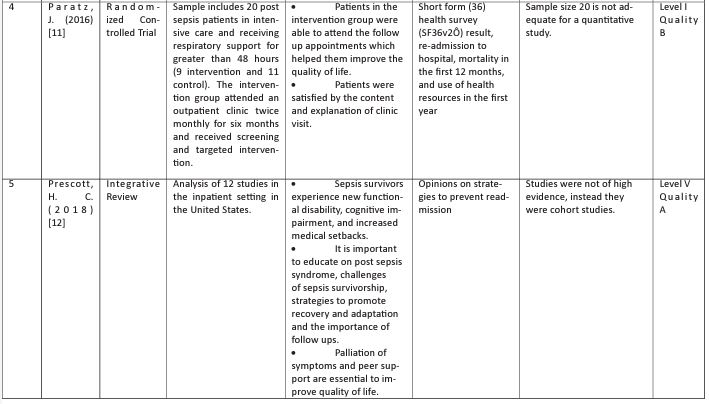
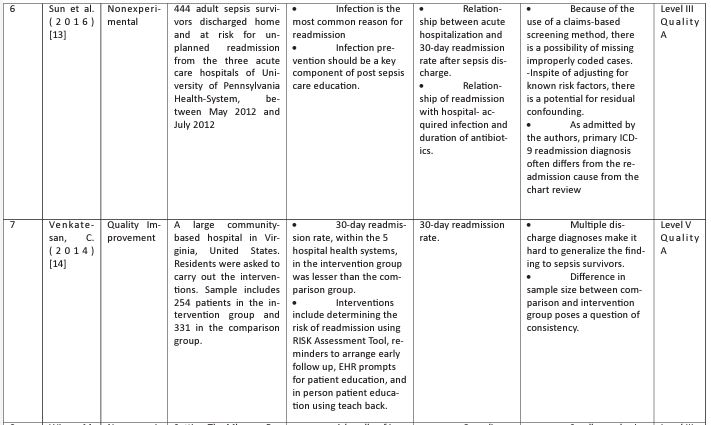
Eight articles published between 2002 and 2018 were included in the final analysis and were found to contain explicit description of the factors contributing to readmission after sepsis discharge and the various strategies including education to prevent readmission. The selected articles consisted of one qualitative study, one randomized control trial, one integrative review, two non-research paper, and three quantitative studies. The studies took place at a range of outpatient/ inpatient sites throughout the world; six articles based in the United States, and the other two in other parts of the world. Using the Johns Hopkins Nursing Evidence- Based Practice Model and guidelines, each article was assessed for evidence level and quality rating [7] (Table 1). The levels of evidence ranged from I-V, and the quality of the articles were good (Quality A or B) except for one.
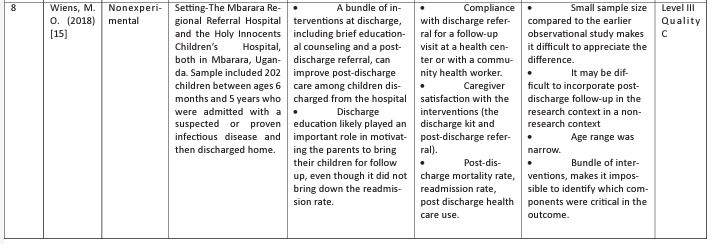
Table 1: Table of Evidence.
Four articles pointed out the importance of discharge education in reducing readmission [9,12,14,15]. Two articles highlighted the importance of training nurses to educate patients on heart failure management and survivorship in reducing readmission [10,8]. Main concepts that emerged from the literature include modifiable causes and risk factors with special emphasis on index hospitalization characteristics, importance of post sepsis care education and the factors to be included in post sepsis care education.
Modifiable causes and risk factors
Longer length of stay, discharge to a facility, hospital acquired infection, volume overload, aspiration, medication reconciliation error, prolonged use of antibiotics, delayed sepsis recognition, delayed ambulation, lack of discharge instruction and proper follow up planning were found to be the potentially modifiable risk factors [12]. The most common cause for readmission following sepsis discharge is a new infection leading to an episode of sepsis [12,13]. Exacerbation of chronic medical conditions was also found to be contributing to readmission following sepsis discharges [12].
Effectiveness of post sepsis care education
Patients greatly appreciated the information given by the case managers on sepsis and post sepsis care [9,14]. Most of them felt safer and cared for. Some patients disliked the education as it reminded them of their serious illness [9]. Brief educational counselling upon discharge improved post discharge care and motivated patients and their families to attend follow up appointments though it did not reduce the rate of rehospitalization [15].
Factors to be included in post sepsis care education
Medical care following sepsis hospitalization should be tailored to alleviate the risk for potential preventable causes of rehospitalization including infection and exacerbation of chronic medical conditions [12,13]. Post sepsis care education should include strategies to reduce the risk for infection-related readmission including vaccine currency and counseling regarding risk for recurrent infection and when to seek medical care [12]. Identification of infection especially when accompanied by signs and symptoms of acute organ dysfunction such as confusion and decreased urine output needs to be an unavoidable educational point [12]. It is important to follow up with primary care within a week following discharge and to be aware of the alternatives in case of an emergency [11,14,15]. Patients should also be educated on aspiration precautions [12].
Discussion
There are modifiable and non- modifiable causes and risk factors which result in readmissions after a sepsis hospitalization. Patient socio-demographics, comorbidities, and hospitalization characteristics are associated with 30-day readmission following a sepsis hospitalization [17,18]. Modifiable hospitalization characteristics include longer length of stay, discharge to a facility, hospital acquired infection, volume overload, aspiration, medication reconciliation error, prolonged use of antibiotics, delayed sepsis recognition, delayed ambulation, lack of discharge instruction and proper follow up planning. Infection was found to be the most common cause for rehospitalization among sepsis survivors [12]. Discharge education on post sepsis care and the risk for readmission would be an ideal approach in preventing readmissions. Currently there is a gap in applying the existing evidence for standardized education on post sepsis care.
This integrative review explored the existing literature on the effect of post sepsis care education on reducing all cause readmission among sepsis survivors. Main aspects related to post sepsis care that emerged from the literature include modifiable causes and risk factors with special emphasis on hospitalization characteristics, importance of post sepsis care education and the factors to be included in post sepsis care education.
Infection, in particular a new infection being the common cause for readmission among sepsis survivors, preventing infection in all the possible ways including vaccine currency and counseling regarding risk for recurrent infection and when to seek medical care can be thought of as a significant component of post sepsis care [12,13]. Comorbidities are common among sepsis survivors [3]. Monitoring and controlling comorbidities are also of prime importance in preventing readmissions.
Out of the six studies analyzed, five included adult population except for the one study which had children between the ages of 6 months and 5 years as the population. Discharge education was received by their parents. Even though discharge education on sepsis did not reduce the rate of readmission, it greatly influenced post sepsis care and encouraged the patients and their families to attend the upcoming appointments [15]. Hygienic practices, signs and symptoms of infection, and importance of early and nearby care were included in the education.
Despite its importance in post sepsis care, follow up visits should be weighed against potential benefits. Burden of multiple comorbidities might make it impossible for patients to attend multiple appointments. Follow up planning should be done wisely so that multiple issues could be addressed in a single visit. Patients need to be made aware of the new challenges including difficulty with memory and concentration, anxiety and depression, and weakness and difficulty completing routine tasks [12]. Strategies to promote recovery following sepsis include working to build up strength and stamina and attending peer support groups [12].
Peer support has been recognized as an intervention to improve the quality of life for sepsis survivors. Through peer support groups patients get an opportunity to know how other sepsis survivors are coping up with the challenges of survivorship and to share their experiences with their peers. Discussion about palliation of symptoms is unavoidable [12]. Aspiration precautions and early mobility were also found to be closely related to better sepsis survivorship.
This review has demonstrated the importance of modifying the risk factors for readmission and improving sepsis survivorship through effective discharge education. It also reminds us about the importance of considering patient’s emotions while delivering information about the disease. The results of this review can be utilized while developing protocols for discharging patients with sepsis. Additionally, this review suggests that certain patients may be more likely to be readmitted, so additional research is needed to determine if targeting specific groups would be most beneficial.
Limitations
This review has several limitations. There was only one study which was level 1 [11]. More high-quality articles would have strengthened this review. Most of the studies were with moderate evidence as they were cohort studies. The study by [9] only emphasized the importance of education on post sepsis care but did not provide the details of patient education by the case managers. The study by [15] provides the details included in patient education, but the study did not bring down the rate of readmission. Three studies included in the review were not US based, which makes it difficult to generalize the findings to the US population.
Conclusion
The purpose of this integrative review was to identify the best practices for post sepsis care education and its effect on reducing all cause readmission among sepsis survivors. The results of this review suggest that hospitalization characteristics, in particular discharge education could be modified and targeted towards preventing readmissions following sepsis hospitalization. Relevant findings from six studies were identified and integrated into three main themes, which then provided the framework for recommendations that could be merged into the current discharge education. Those recommendations include recognizing the signs and symptoms of infection, monitoring comorbidities, and attending follow up visits, and peer support groups. This review ultimately acts as a foundation for future exploration into the relationship between post sepsis care education and the quality of life of patients who received that education. Further research should address the limitations and gaps in knowledge acknowledged in this review; moreover, it will be critical to the development and implementation of best practices to combat the escalating all cause readmission among sepsis survivors.
References
- Mayr FB, Talisa VB, Balakumar V, Chang CH, Fine M, et al. Proportion and cost of unplanned 30-day readmissions after sepsis compared with other medical conditions. Jama. 2017; 317: 530.
- World Health Organization. Global report on the epidemiology and burden of sepsis: Current evidence, identifying gaps and future directions. 2020.
- Galiatsatos P, Follin A, Uradu N, Alghanim F, Daniel Y, et al. The association between neighborhood socioeconomic disadvantage and readmissions for patients hospitalized with sepsis. American Journal of Respiratory and Critical Care medicine. 2019; 199.
- Jones TK, Fuchs BD, Small DS, Halpern SD, Hanish A, et al. Post-acute care use and hospital readmission after sepsis. Annals of the American Thoracic Society. 2015; 12: 904-913.
- Zilberberg MD, Shorr AF, Micek ST, Kollef MH. Risk factors for 30-day readmission among patients with culture-positive severe sepsis and septic shock: A retrospective cohort study. Journal of Hospital Medicine. 2015; 10: 678-685.
- Jencks SF, Williams MV, Coleman EA, Jencks SF, Williams MV, et al. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009; 360: 1418-1428.
- Dang D, Dearholt SL. Appendix D: Evidence level and quality guide. In Johns Hopkins Nursing Evidence-Based Practice: Model and Guidelines. Sigma Theta Tau. 2017.
- Di Palo KE, Patel K, Assafin, M, Pina IL. Implementation of a patient navigator program to reduce 30-day heart failure readmission rate. Progress in cardiovascular diseases. 2017; 60: 259-266.
- Gehrke-Beck S, Bänfer M, Schilling N, Schmidt K, Gensichen J, et al. The specific needs of patients following sepsis: A nested qualitative interview study. CBJGP Open. 2017; 1.
- Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. 2002.
- Paratz J, Kenardy J, Comans T, Coyer F, Thomas P, et al. A follow up clinic for sepsis survivors-preliminary results and feasibility. Intensive Care Medicine Experimental. 2016; 4.
- Prescott HC. Preventing chronic critical illness and rehospitalization: A Focus on Sepsis. Crit Care Clin. 2018; 34: 501-513.
- Sun A, Netzer G, Small DS, Hanish A, Fuchs BD, et al. Association between index hospitalization and hospital readmission in sepsis survivors. Crit Care Med. 2016; 44: 478-487.
- Venkatesan C, Maaty N, Lui K, Kalwaney S, Mishra A, et al. Standardizing the discharge process with an electronic medical record-based checklist - A resident-LED quality improvement initiative. Journal of General Internal Medicine. 2014; 29: S496.
- Wiens MO, Kissoon N, Kabakyenga J. Smart hospital discharges to address a neglected epidemic in sepsis in low- and middle-income countries. JAMA Pediatrics. 2018; 172: 213-214.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009; 6: e1000097.
- Goodwin AJ, Rice DA, Simpson KN, Ford DW. Frequency, cost, and risk factors of readmissions among severe sepsis survivors. Critical Care Medicine. 2015; 43: 738-746.
- Centers for disease control and prevention Sepsis Data & Reports. 2020