Case Report - Volume 3 - Issue 4
Menstrual irregularity and chronic pelvic pain revealing Krukenberg tumours: The contribution of imaging
Imane Mahdar*, G.Lembarki, M.Banao, M.Sabiri, S.Lezar, F.Essodegui
Central Unit of Radiology, Ibn Rochd University Hospital, Casablanca, Morocco.
Received Date : June 22, 2023
Accepted Date : July 28, 2023
Published Date: Aug 04, 2023
Copyright: © Imane Mahdar 2023
*Corresponding Author : Pina J Imane Mahdar, Central Unit of Radiology, Ibn
Rochd University Hospital, Casablanca, Morocco
Email: imahdar80@gmail.com
DOI: Doi.org/10.55920/2771-019X/1521
Abstract
The Krukenberg tumour represents 1-2% of all ovarian masses. It is a rare metastatic tumour of the ovary with a reserved prognosis. The purpose of this case-based article is to discuss imaging features and findings associated with Krukenberg tumours. We present the case of a 30-year-old woman with menstrual irregularity and chronic pelvic pain presenting bilateral ovarian masses on ultrasound. CT scan showed an antro-pyloric wall thickening and peritoneal carcinomatosis. Endoscopy was not conclusive. Biopsy performed during a staging laparoscopy confirmed the diagnosis of Krukenberg tumour. Imaging methods have a valuable contribution in establishing the diagnosis and prognosis of this tumour.
Keywords: Krukenberg, linitis plastica, CT scan.
Introduction
Krukenberg is a rare signet ring cell metastatic tumour of a digestive adenocarcinoma mostly originating from the stomach. It is bilateral in more than 80% of the cases and it represents 1-2% of all ovarian tumours (1). Unlike primary ovarian cancer, Krukenberg tumours are more likely to occur in younger women, which can be explained by the high blood supply leading to hematogenous spread. The clinical presentation varies and is not specific. Imaging examinations including ultrasound, CT, and MRI are very contributive in both the diagnosis and prognosis. Patients present an uneven knobby ovarian surface as well as ascites and lymphatic involvement. The treatment approach remains controversial due to its poor prognosis [1-2].
Clinical presentation
We present the case of a 30-year-old female with no prior medical history. She consulted initially for chronic pelvic pain and menstrual irregularity for over 6 months. The patient reported recurrent episodes of epigastric pain and nausea that have been treated as gastritis as well as a weight loss of over 22 kg over the last 5 months. Serum levels of CA-125 were elevated (155 U/ml).
Differential diagnosis:
Before imaging, the differential diagnosis included primary ovarian tumours.
Investigations/Imaging findings
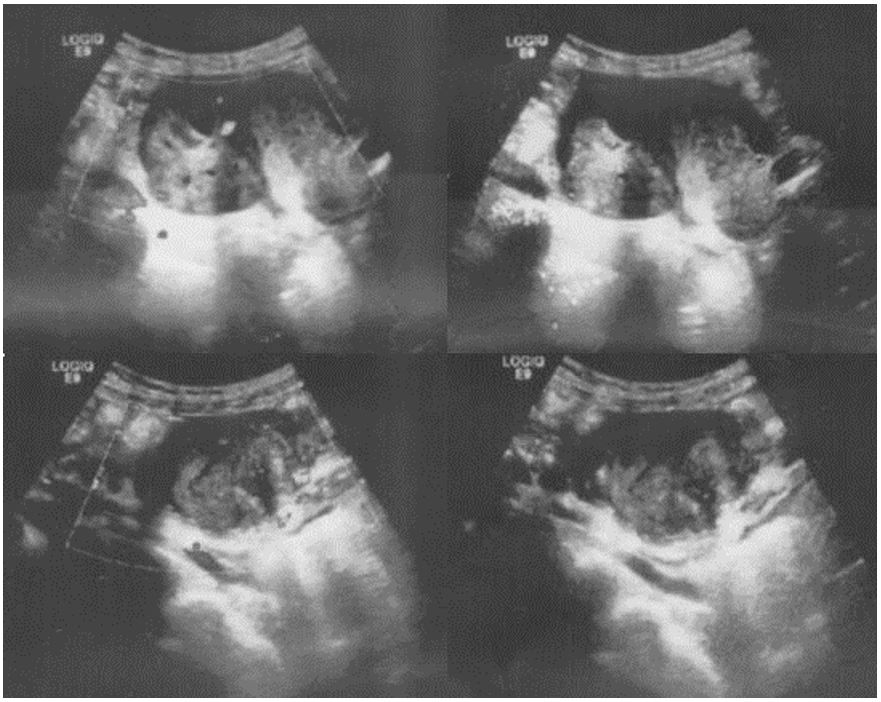
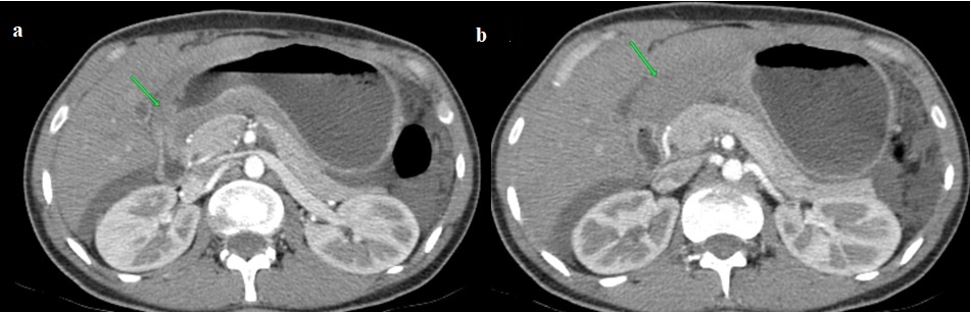
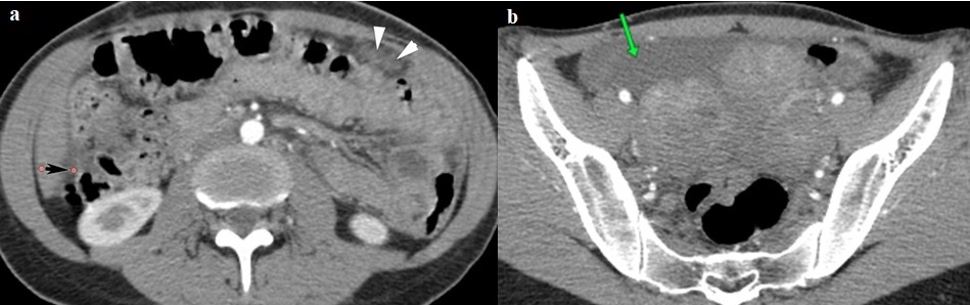
A pelvic ultrasound was performed with a 3.75 MHz convex probe. It revealed bilateral large, well-defined, heterogeneous ovarian masses with irregular margins, containing solid and cystic components, we noted increased vascularity in the solid parts and the presence of hypoechoic areas in favour of necrotic areas (Figure 1). In addition, free fluid in the peritoneal cavity was found in the following regions: perihepatic, perisplenic, pelvic, and between the intestinal loops. Krukenberg tumour was suspected. To confirm the diagnosis an abdominal and pelvic contrast-enhanced computed tomography (CT) examination was indicated. It showed a focal enhanced wall thickening of the antro-pyloric region measuring 13 mm, as well as the obliteration of the fat cleavage plane between the gastric wall and the liver suggestive of an invasive T4 tumour (Figure 2). Peritoneal carcinomatosis was also found as a nodular invasion of the greater omentum and parietal peritoneal thickening was noted, associated with moderate ascites (Figure 3). In the pelvis, two large tissular masses originating from the ovaries were visualized. They expressed heterogeneous contrast enhancement. (Figure 4). An esophagogastroduodenoscopy (EGD) was performed, revealing a thickened, erythematous, indurated gastric mucosa and the biopsy was not conclusive. Later on, a staging laparoscopy was performed with gastric and peritoneal biopsies. Histological examinations confirmed the presence of the ‘signet ring’, consequently, the diagnosis of linitis plastica (LP) was established.
Figure 1: Ultrasound images showing two large heterogeneous masses arising from the ovaries.
Figure 2: CT images showing enhanced wall thickening of the antro-pyloric region of the stomach (a), associated with obliteration of the fat cleavage between the gastric wall and the liver (b).
Figure 3: CT images showing nodular invasion of the greater omentum (white arrowheads), parietal peritoneal thickening (black arrow) (A), and moderate ascites (B).
Figure 4: CT images showing two large ovarian masses with heterogeneous enhancement after contrast agent administration.
Treatment
The tumour was staged T4N0M1 and the patient underwent a palliative treatment plan. She received 6 cures of chemotherapy.
Discussion
About 76% of all Krukenberg tumours originate in the stomach, followed by the colon and rectum (11%), the breast (4%), the biliary system (3%), the remaining 3% includes various sites such as the pancreas, the uterine cervix, urinary bladder and the renal pelvis [3]. The prognosis of a Krukenberg tumour originating from gastric cancer is worse than that of other primary sites. The revelation of the primary cancer site can be masked by ovarian symptoms or other metastatic sites. Patients commonly present abdominal or pelvic pain, vomiting, nausea, vaginal bleeding, and dyspareunia. Ultrasound is usually the first prescribed imaging modality when it comes to pelvic pain and genital abnormalities. The ovarian metastasis can be solid (stomach or breast tumours), mixed (colon, rectum, appendix, or biliary tract), or less frequently predominantly cystic (colon or appendix primary tumour). The solid component is usually heterogeneous hyper or iso-echoic with randomly dispersed vessels noted in the doppler analysis [2]. CT scan demonstrates a variety of aspects, most commonly pelvic masses with heterogeneous enhancement. It is very contributive in assessing the extension to the adjacent organs and structures and establishing the TNM staging. It is also useful in identifying the primary tumour. The treatment approach for patients with linitis plastica is very controversial. It has been recognized that patients undergoing complete resection have a better survival rate. However, the presence of peritoneal carcinomatosis or free peritoneal tumour cells makes the tumour inoperable. The CT scan can determine the presence of peritoneal nodules, masses, peritoneal thickening, and enhancement which can be confirmed by histology after a staging laparoscopy. In these cases the treatment options are palliative and the prognosis is very reserved [2-4].
Learning points
- An ovarian mass associated with signs of gastritis should raise suspicion of a Krukenberg tumour.
- Krukenberg is a rare metastatic ovarian tumour in young women, more commonly originating from the gastrointestinal tract, particularly the stomach.
- Imaging modalities are very valuable in establishing the diagnosis. They are also very solicited in determining the treatment approach and the prognosis.
- CT scan should look for signs of gastric wall thickening, invasion of adjacent organs, and signs of peritoneal carcinomatosis.
Consent statement
No identifying information in the text or images appears in this case report.
The patient consented to this publication.
References
- Young RH. From Krukenberg to today: the ever-present problems posed by metastatic tumors in the ovary: part I. Historical perspective, general principles, mucinous tumors including the Krukenberg tumor. Adv Anat Pathol. 2006; 13: 205-27.
- Wu F, Zhao X, Mi B, Feng L, Yuan N, Lei F et al. Clinical characteristics and prognostic analysis of Krukenberg tumour. Mol Clin Oncol. 2015; 3: 1323-1328.
- Irving JA, Vasques DR, McGuinness TB, Young RH. Krukenberg tumour of renal pelvic origin: report of a case with selected comments on ovarian tumors metastatic from the urinary tract. Int J Gynecol Pathol. 2006; 25: 147-150.
- Zulfiqar M, Koen J, Nougaret S, Bolan C, VanBuren W, McGettigan M, et al. Krukenberg Tumours: Update on Imaging and Clinical Features. AJR Am J Roentgenol. 2020; 215 (4): 1020-1029.