Research article - Volume 3 - Issue 4
Tuberculosis medication adherence in a secondary care center in SouthEastern Nigeria
Gabriel Chidera Edeh1; Chijioke Amara Ezenyeaku2; Chigozie Ozoemena Ifeadike2; Michael Chukwuebuka Awugosi1; Onyeka Chukwudalu Ekwebene3*; Chinonuju Franklin Chiekezie1; Samuel Ifeanyi Emmanuel1
1Faculty of Medicine, Nnamdi Azikiwe University, Awka, Nigeria.
2Department of Community Medicine, Nnamdi Azikiwe University Teaching Hospital Nnewi, Nigeria.
3Department of Biostatistics and Epidemiology, East Tennessee State University, Johnson City, TN, USA.
Received Date : May 10, 2023
Accepted Date : July 28, 2023
Published Date: Aug 04, 2023
Copyright:© Gabriel Chidera Edeh 2023
*Corresponding Author : Onyeka Chukwudalu Ekwebene, Department
of Biostatistics and Epidemiology, East Tennessee State University,
Johnson City, United States.
Email: ekwebene@etsu.edu
DOI: Doi.org/10.55920/2771-019X/1522
Abstract
Adherence to a treatment strategy known as Directly Observed Treatment Short course (DOTS) by patients diagnosed of tuberculosis is essential in the effective treatment of the disease. This is in order to avoid recurrence, resistance and complications that results from non-adherence. This paper assessed the adherence to anti-tuberculosis medications among tuberculosis patients in a secondary healthcare facility in Anambra State, Nigeria. This was a descriptive crosssectional study and a semi-structured interviewer-administered questionnaire was used. The study population comprised of tuberculosis patients who has been on anti-TB medications for at least four weeks at the Tuberculosis clinic. A systematic random sampling technique was used to enrol the respondents into the study. The mean age of the respondents was 39.68±16.66 years. Majority of the respondents correctly alluded to tuberculosis as being caused by bacteria (91.7%); and that the duration of treatment was at least six months (100.0%). A great proportion of the respondents affirmed that a vaccine is available for prevention of tuberculosis infection (91.7%); also all the respondents agreed that covering mouth and nose while coughing/sneezing is a preventive measure of TB spread (100.0%). About 15.2% of the respondents sometimes stop taking their medications when they feel their health condition is under control, however, a great proportion of the respondents had good adherence to medications (76.0%). Major reasons for missing medication among the non-adherent were that they forgot (91.8%) and that there were too much medication to take at once (1.2%). Statistically significant associations existed between drug adherence and age, sex and educational qualification; as respondents within the age range of 60-69 years, female and those who had completed tertiary education had better adherence to anti-TB medications. TB medication non-adherence is a potential risk factor for poor health outcomes, hence more effort is needed to increase the rate of adherence.
Keywords: Tuberculosis; adherence; Tuberculosis patients; Directly observed therapy short course (DOTs).
Background
Tuberculosis (TB) is an infectious disease caused mainly by Mycobacterium tuberculosis, and occasionally by Mycobacterium bovis or Mycobacterium africanum.1 The lungs are usually affected (pulmonary TB), but other sites could also be affected (extra pulmonary tuberculosis) [1]. It is acquired by inhalation of infected droplets coughed out by infected persons and by consumption of unpasteurized milk from infected cow. Tuberculosis thrives where poverty, overcrowding and chronic debilitating illness abound [2]. The true sign of active TB are chronic cough with blood-containing sputum, fever, night sweats, and weight loss [3]. Gene expert, a polymerase-chain reaction(PCR)-based method is the current gold standard for the diagnosis of tuberculosis [4].
Reports has shown that one third of the world population is infected by Tubercle bacilli and are at risk of developing active disease [5]. Globally In 2016, there were an estimated 10.4 million new cases of tuberculosis, of which about 600,000 of the new cases have resistance to Rifampicin [6]. About 429,000 people in Nigeria have TB each year, while the total TB incidence rate was reported as 219 per 100,000 population [7,8]. Nigeria is at the top spot in Africa and sixth globally among the 30 high TB burden countries, and is also among the 14 countries in the world with the triple high burden of TB, TB/HIV and MDR-TB [8].
Adherence to a treatment strategy known as Directly Observed Treatment Short-course (DOTS) by patients diagnosed of tuberculosis is essential in the effective treatment of the disease. This is in order to avoid recurrence, resistance and complications that results from non-adherence. The emergence of resistance to drugs used to treat tuberculosis and particularly multi-drug resistant tuberculosis (MDR-TB) is a significant problem and poses obstacle to effective TB control at both national and global levels. Resistance arises at various management level of a patient, ranging from poor compliance, inadequate supervision, inadequate dosing, drug combinations, duration of treatment and poor training of staff [9]. In a Nepal cross-sectional study, it was found that 48% of the tuberculosis patients were non-compliant with their medication [10]. In a Ghana study on the adherence of TB patients to treatment in the Ketu North District in the Volta Region of Ghana, the adherence rate (81.6%) was discovered which was higher than that recorded in Suhum in the Eastern Region of Ghana (63%), but lower than rates reported in Tanzania (95.7%) and Ethiopia (90.0%) [11-14]. A study done in North-western Nigeria indicated that 30.5% of TB patients defaulted in their TB medication use [15]. In a different study done in Osun State, non-compliance rate to tuberculosis treatment among TB patients in Osun State health facilities was found to be high [16]. A study done in Anambra State by Ubajaka et al demonstrated that 74.7% of the patients were adherent to their drugs [17]. In Another study by Ohamaeme and Ibeh et al in a rural and an urban area shows an adherence rate of 86.2% and 87.6% respectively [18].
Secondary healthcare facility is a second tier of healthcare in Nigeria and hence a major point of access to care for a great number of patients including tuberculosis patients. From literatures reviewed, all the works done in this discourse in this locality took place in tertiary healthcare facilities, hence the need for this work. Also, despite Anambra State having a high rate of default from pulmonary tuberculosis treatment, there has been little work done to identify and readjust this anomaly. Hence, this study will help in determining the baseline knowledge about tuberculosis; adherence to TB treatment; give insight into the various factors influencing treatment defaulting and the relationship of socio-demographics to their level of knowledge and adherence to treatment. Through this, an individualized management approaches and culturally sound intervention strategies can be designed that would help for improvement of adherence to anti-tuberculosis medications thereby helping in tuberculosis control in the region and Nigeria at large.
Methodology
Area of Study
This study was conducted at Saint Charles Borromeo Specialist Hospital located in Onitsha South Local Government Area, Anambra State, Nigeria, a secondary healthcare facility and one of the biggest non-governmental hospitals in South-Eastern Nigeria. It was officially opened in 1965 and have over 250 bed spaces [19] and is integrated with National Tuberculosis and Leprosy Control Programme (NTBLCP) which provide free anti-tuberculosis medicines and services to the public. Onitsha-South harbours a population of about 138,000 people according to 2006 census with nearly equal distribution of male and female and was projected to be around 181,000 people in 2016 , however the major occupation of the inhabitants include: farming, trading, white-collar jobs, businesses, and several others [20,21].
Study Design
A cross-sectional descriptive study design was adopted for this work.
Study Population
The study population comprised of tuberculosis patients who has been on anti-TB medications for at least four weeks at the Tuberculosis Directly Observed Therapy (TbDOTS) clinic in Saint Charles Borromeo Specialist Hospital, Onitsha-South, Anambra state, Nigeria.
Inclusion Criteria
Tuberculosis patients in the clinic who has been on anti-TB medications for at least four weeks in the facility and gave their consent to participate in the study were drafted.
Exclusion Criteria
Respondents that met the study criteria but did not give consent.
Tuberculosis patients attending the clinic who were too sick to participate in the study.
Presumptive tuberculosis cases who are yet to be confirmed.
Tuberculosis patients who had not undergone treatment for up to a month in the facility.
Sample Size Determination
The Cochran’s formula below was used to calculate the sample size
N= Z 2 PQ/D2
where N is the minimum sample size:
Z is the standard normal deviate (1.96) at 95% confidence level.
P = Prevalence of adherence to anti-tuberculosis medication among tuberculosis patients in a study conducted in Anambra state by Ohamaeme et al =87.6% = 0.876 [18].
Q= 1-P = 0.124
D is the degree of precision,which is usually set at 5%(0.05)
N= 1.962x 0.876x 0.124/0.052
N= 166.92 ≈ 167
Therefore, anticipating a non-response rate (f) of 10% as used in a previous study on drug adherence to tuberculosis medication16, the adjusted sample size (Ns) were
Ns = N / 1-f = 167 / 1-0.1 = 167 / 0.9 = 185.46= 185. However, the sample size were later made up to 204.
Sampling Technique
A systematic random sampling technique was adopted for this study. A sample frame was gotten from the records department at the hospital, comprising of the appointments for the TbDOTs clinic days. The Center had five (5) TbDOTs clinic days in a week running from Tuesday to Saturdays with an average of eight (8) patients attending each clinic day. The time for sample collection was estimated to be 10 weeks (i.e. about 2 months and 2 weeks), thus each week 20 out of the 40 persons in a week were recruited in order to make up the sample size of 204. The sample interval was thus calculated: 40/20 = 2. The first person to be recruited for each sample collection day was selected from the first two names in the sampling frame using simple random sampling by balloting and then every 2nd person from this name were selected subsequently. When a selected individual declines to be part of the study, the next person was selected and every second person after him/her until the sample size was achieved.
Study Instrument
Data were collected through a semi structured interviewer administered, anonymous and validated questionnaire after seeking verbal informed consent following a proper orientation of the participants of the objectives and the impact of this study to the society. The questionnaire was developed with guidance from several works already done on the subject/related works [15-17, 22].
Training of Research Assistants
Two (2) research assistants were recruited and trained to help with carrying out this research in record time. These research assistants were nurses working in tuberculosis clinic at St. Charles Borromeo Hospital, Onitsha. They were trained on the contents of the questionnaire, which includes: knowledge of tuberculosis covering aetiology, transmission, treatment and prevention of tuberculosis; adherence to anti-tuberculosis medication; factors influencing drug adherence to anti-tuberculosis medications which was divided into lifestyle factors and health facilities related factors.
Data Management
Measurement of Variables
The main outcome/dependent variable for this study was compliance to anti-TB medications while the independent variables were the socio-demographics, knowledge of tuberculosis and factors influencing the adherence to anti-TB medications.
Assessment of Knowledge
Patients’ knowledge were assessed by asking seven (7) questions about tuberculosis covering the disease aetiology, mode of transmission, treatment and prevention of tuberculosis. Respondents who scored 50% and above were assumed to have “good knowledge” while those who scored less than 50% were considered to have “poor knowledge” about tuberculosis.
Assessment of Drug Adhrence
Non-adherence to anti-TB drugs means an individual whose score is <6 points in the Morisky
Medication Adherence Scale-8 (MMAS-8). MMAS-8 consists of eight items, with a scoring scheme of “yes” = 0 and “no” = 1 for the first seven items, but for the last item, a five-point Likert scale response was used with options of “never,” “once in a while,” “sometimes,” “usually,” and “always.” In this Likert scale, values ranging from 0 to 1was given at a specified interval of 0.25 with “1” given for “never” and “0” given for “always.” The degree of adherence were determined according to the score resulting from the sum of all the correct answers to a maximum score of 8. For the purpose of data analysis, the three original categories of adherence which were ‘high, medium and low’, was re-categorized into two. Accordingly, high and medium adherence was reassigned as adherent with a score greater than or equal to six (6) and low adherence were regarded as non-adherent with a score of less than 6.
Statistical Analysis
Data were analysed using SPSS version 24. Descriptive and inferential Statistics was applied where necessary. Numerical variables were reported as mean and standard deviation, while categorical data were reported using proportion and percentages. Chi-square test was used to assess the association between categorical variables. Variables with p-value ≤ 0.05 in the confidence interval of 95% was taken as being significant.
Results
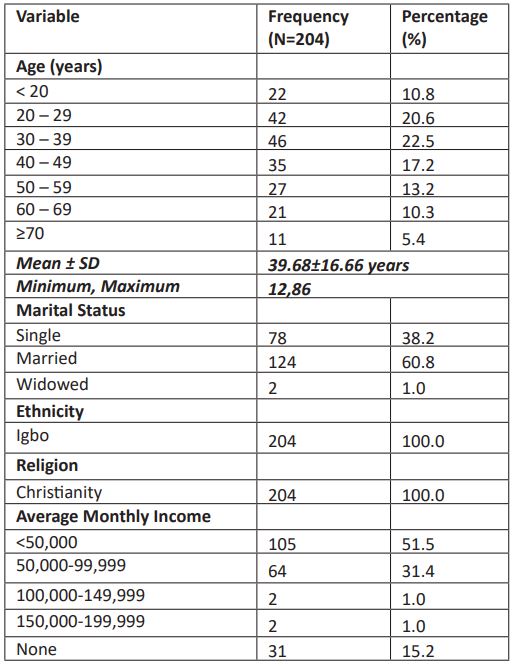
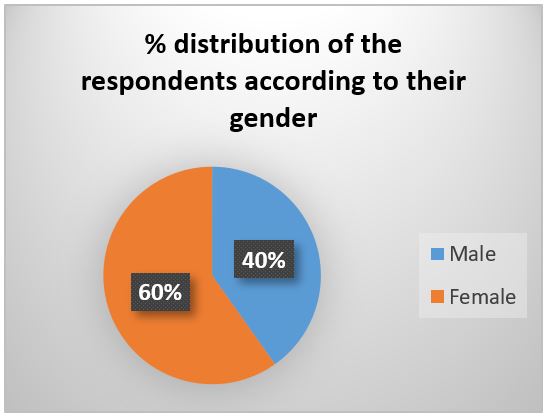
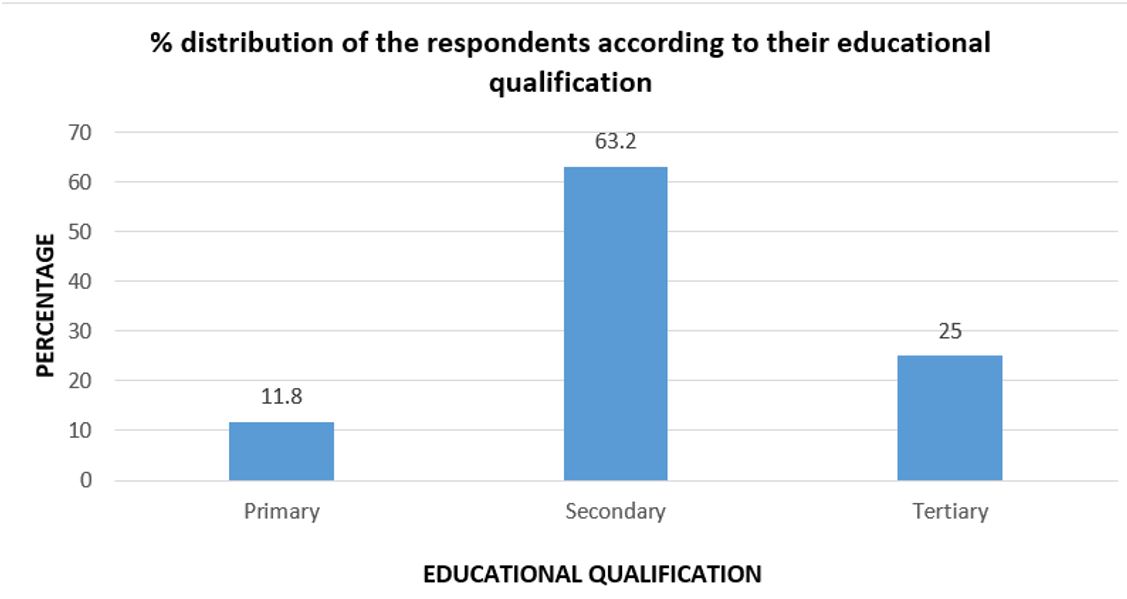
A total of 204 questionnaires were administered to all the tuberculosis patients in the clinic who has been on anti-TB medications for at least four weeks in the facility. All the questionnaires were retrieved, giving a response rate of 100%. Table 1 summarizes the socio-demographic characteristics of the respondents. Their ages ranged from 12 to 86 years with a mean age of 39.68±16.66 years. Majority of the respondents (22.5%) were in the age range of 30-39 years, however, a significant proportion of the respondents were in the age range of 20-49 years and when combined, this age range contains the highest proportion (60.3%) of the respondents. Approximately two-third of the respondents were married (60.8%), however about half of the respondents make an average monthly income of <N50,000 (51.5%). All the respondents were Igbo by tribe and also all were Christians. Figure 1 above shows the percentage distribution of the respondents according to their gender. About 60% of the respondents were female while only 40% were male. Figure 2 above shows the percentage distribution of the respondents according to their educational qualification. About two-third of all the respondents (63.2%) had completed secondary education while the least proportion of the respondents (11.8%) had Primary education as their highest educational qualification.
Table 1: Socio-Demographic characteristics of the respondents.
Figure 1: Distribution of the respondents according to their gender.
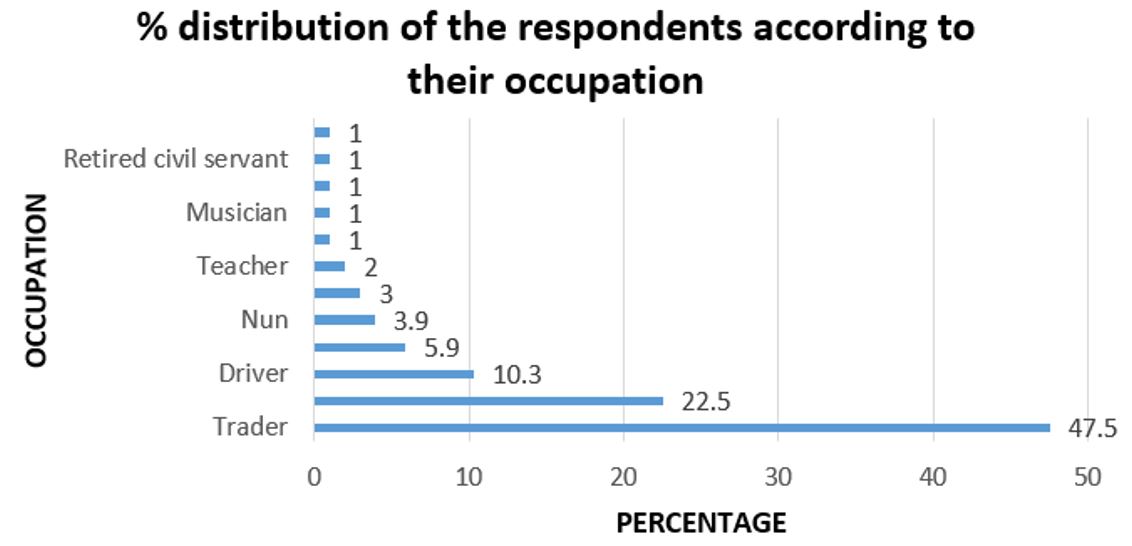
Figure 3: Distribution of the respondents according to their occupation.
Table 2: Respondents’ knowledge of tuberculosis.
Table 3: Respondents’ adherence to anti-tuberculosis medication using morisky medication adherence scale (mmas)-8.
Table 3: Respondents’ adherence to anti-tuberculosis medication using morisky medication adherence scale (mmas)-8.
Table 4: Factors influencing drug adherence to anti-tuberculosis medication.
Table 4.1: Disease and medication related characteristics
Table 4.2: Lifestyle factors.
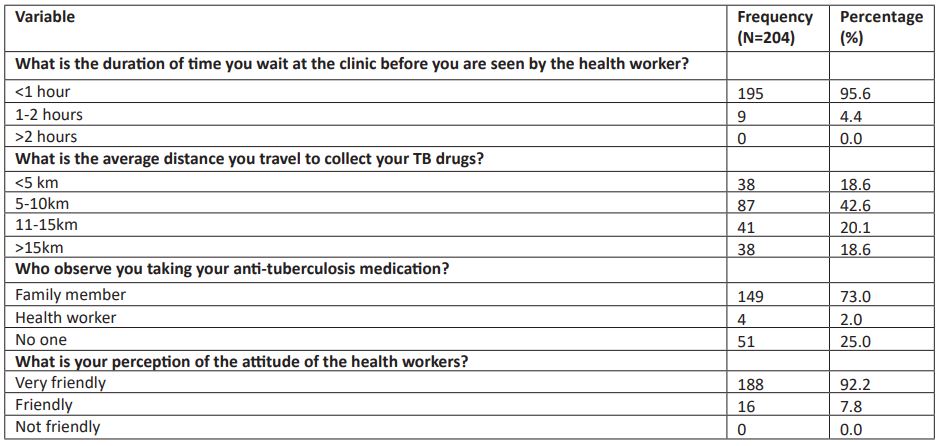
Table 4.3: Health facilities related factors.
Table 5: Association between the respondents’ socio-demographics and knowledge of tuberculosis.
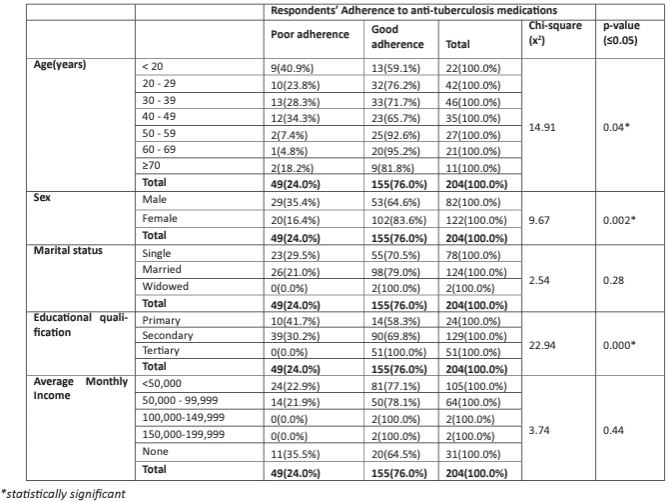
Table 6: Relationship between the respondents’ socio-demographics and adherence to anti-tuberculosis medications.
Figure 3 above shows the percentage distribution of the respondents according to their occupation. About half of all the respondents (47.5%) were traders while the least proportion of the respondents (1% each) were food vendors, plumbers, retired civil servants and tailors.
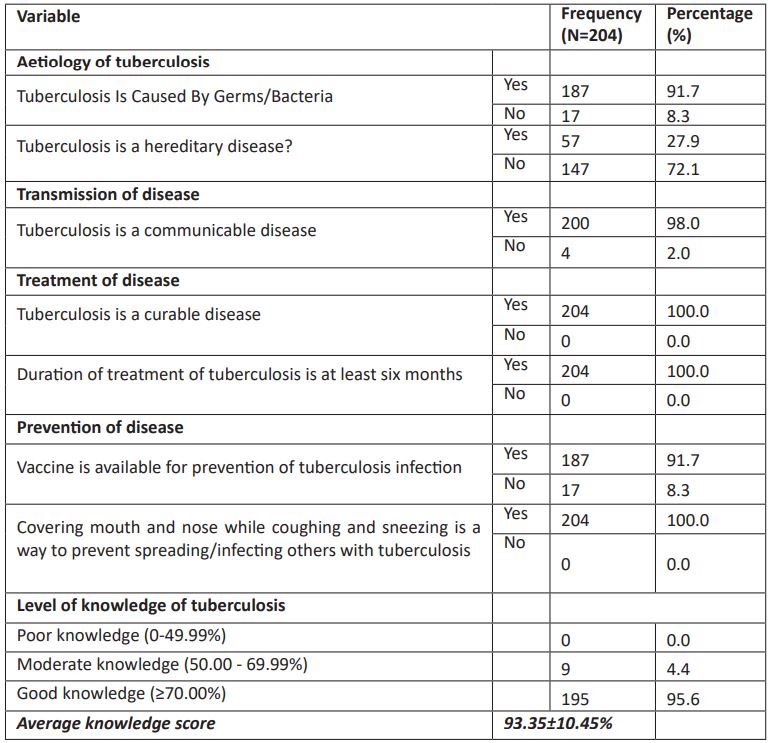
Table 2 above shows the knowledge of tuberculosis among the respondents. As regards the aetiology of tuberculosis, majority of the respondents correctly alluded to tuberculosis as being caused by bacteria (91.7%); and that it is not a hereditary disease (72.1%). With respect to the transmission of tuberculosis, almost all the respondents attested to TB being a communicable disease (98.0%). As regards the treatment of TB, all the respondents agreed that TB is a curable disease (100.0%); and that the duration of treatment is at least six months (100.0%). Also, a great proportion of the respondents attested that a vaccine is available for prevention of tuberculosis infection (91.7%); however all the respondents agreed that covering mouth and nose while coughing and sneezing is a preventive measure of TB spread/infection (100.0%). Overall, almost all the respondents had good knowledge of tuberculosis (95.6%), with an average knowledge score of about 93.35±10.45%.
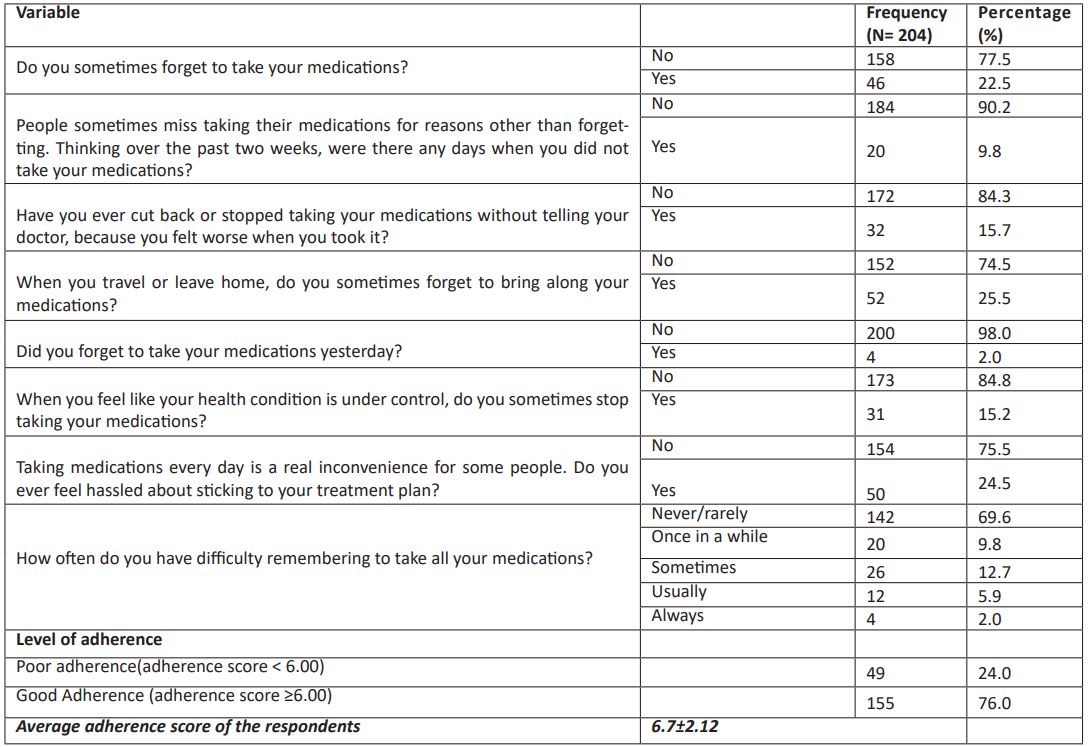
Table 3 above shows the respondents adherence to anti-TB medication using MMAS-8. A great proportion of the respondents claimed they do not sometime forgot to take their medications (77.5%); that for the past two weeks there were no day they did not take their medication (90.2%); never cut back or stopped taking their medications without telling their doctor because they felt worse when they took it (84.3%); never forgot to bring along their medication when they travel or leave home (74.5%); however, only 2.0% of the respondents forgot to take their medication yesterday. About 15.2% of the respondents sometimes stop taking their medications when they feel like their health condition is under control and only about 24.5%feel hassled about sticking to their treatment plan. More than two-third of the respondents never/ rarely had difficulty remembering to take all their medications (69.6%), however a few of the respondents always had difficulty remembering to take all their medications (2.0%). Overall, a great proportion of the respondents had good adherence to anti-TB medications (76.0%).
As regards health facility related factors influencing TB medication adherence, majority of the respondents’ average waiting time in the clinic were less than an hour (95.6%) and most of them travel an average distance of about 5-10km to collect their TB drugs (42.6%). Majority of the respondents were observed by family members (73.0%) while taking their anti-TB medicines, however about a quarter of them were observed by no one (25.0%). All the respondents attested to the health workers as being very friendly to them.
Table 5 shows the association between respondents’ knowledge of tuberculosis and socio-demographic characteristics at the bivariate level using chi-square test of statistical significance. Statistically significant associations existed between level of knowledge and sex of the respondents as female had better knowledge of tuberculosis. Table 6 shows the association between respondents’ adherence to anti-TB medication and socio-demographic characteristics at the bivariate level using chi-square test of statistical significance. Statistically significant associations existed between drug adherence and age, sex and educational qualification; as respondents within the age range of 60-69 years, female and those who had completed tertiary education had better adherence to anti-TB medications.
Discussion
Socio-Demographic Characteristics
The ages of the respondents in this study ranged from 12 to 86 years with mean of 39.68±16.66 years, which coincides with the mean age in a similar study done in Anambra [17]. however it is in contrast to a similar study in north-western Nigeria where their average age were 51.5± 13.8 years.. The age range of 30 - 39 years has the highest percentage (22.5%) in this study which contrasted with the findings of a prior study in Anambra by Ubajaka et al and another study done in Ogun state which revealed that the age group 20 - 29 years had the highest number of TB respondents [17, 23]. However, a significant proportion of the respondents were in the age range of 20-49 years with a prevalence of 60.3%, which was similar to a finding in North-western Nigeria and another study done in Osun state, Nigeria where majority of the study participant were aged between 20 – 50 years [17,18]. There were more females (60.0%), than males (40.0) and this higher percentage of female patients in this study may be because of the general attitude of men in this environment whereby they do not access healthcare until their health deteriorates to the extent that they cannot carry out their daily activities effectively. Majority of the respondents in this study had secondary education (63.2%), which was similar to the study done in North-western Nigeria by Iweama et al [15]; however it contradicted the findings by Ubajaka et al where majority of the respondents had primary educational qualification [17]. Most of the respondents in this present study were traders (47.3%) which was similar to the findings by Ubajaka et al in Anambra State, Nigeria where traders made up about 44.7% of the respondents [17].
Knowledge of Tuberculosis
The patients’ knowledge of TB was considerably high as nearly all respondents identified bacteria as the aetiological agent, that it’s a communicable disease, curable, six months as the least duration of treatment and that covering mouth and nose while coughing and sneezing is a preventive measure. As regards the aetiology of tuberculosis, majority of the respondents correctly alluded to tuberculosis as being caused by bacteria (91.7%) which was higher compared to a prior study in Ogun state where they discovered 71.7% [23]. All the respondents in this study knew that the duration of treatment was at least six months which was similar to the findings by Ajao et al in Osun state [16]. All the patients (100.0%) knew about the precaution method of covering the mouth and nose while coughing or sneezing to prevent transmission to people around which is similar to the Ogun state study by Olawunmi et al [23]. Overall, almost all the respondents had good knowledge of tuberculosis (95.6%), which is in tandem with the discovery by Olawunmi et al, where about 94.2% had a good knowledge about tuberculosis [23]. This good knowledge of tuberculosis as discovered in this study could be attributed to the fact that majority of them had already completed at least secondary education and also the health education given to them as they access care.
Adherence to Anti-Tuberculosis Medications
This study has demonstrated that 76.0% of the patients were adherent to their drugs which was similar to a prior study among TB patients in Anambra State as discovered by Ubajaka et al [17], where they reported an adherence rate of 74.7%, and another in Ogun State with adherence rate of 75.8% [23]; however in a different study done in the same Anambra State by Ohamaeme and Ibeh et al in a rural and an urban settings reported an adherence rate of 86.2% (rural) and 87.6%(urban) respectively which was higher than what was found in this study [18]. The non-adherence rate of 24.0% discovered in this study was lower than that found in a study done in North-western Nigeria which indicated that 30.5% of TB patients defaulted in their TB medication [15] and several other studies in which higher non-adherence rates were reported [24-26]. In Africa, studies done in Tanzania, Ethiopia and Ketu North District in the Volta Region of Ghana reported adherence rate of 95.7%, 90.0% and 81.6% respectively which was way higher than what was gotten in this study, however a study done in Suhum in the Eastern Region of Ghana recorded 63%, which was lower than the rate from this study [11-14]. From this study also, age, sex and educational qualification of the TB patient were found to be significantly associated with compliance to TB treatment. This is similar to previous studies findings such as the one done in Osun state where educational status of the TB patient was found to be significantly associated with compliance to TB treatment [16]. Lower socioeconomic status of the patient such as lower education, economically restraint and unemployment were linked with poor adherence to tuberculosis treatment in a study done in South Africa among public primary care tuberculosis patients [27], however other studies done in Thailand, Ethiopia, Equatorial Guinea and in Nigeria found no significant association between adherence level with socio-demographic or economic status of the patients [28-30]. The high adherence rate observed in this study could because of the health education given to the patients at the point of accessing care. The similarities and dissimilarities noted in relation to other studies could be because of the differences in methodology including study design, type of sampling technique, sample size, and definition of adherence.
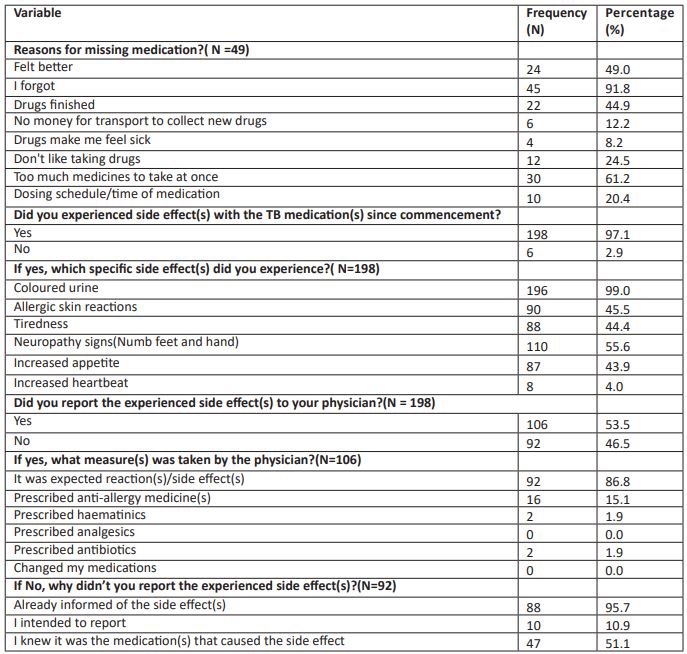
Factors Influencing Adherence to Anti-Tuberculosis Medication
With respect to disease and medication related characteristics, major reasons for missing medication among the non-adherent were that they forgot (91.8%) and that they were too much medication to take at once (1.2%). Dual or triple diseases requires that they take two or more sets of drugs, which could prove to be quite burdensome to the patient. Almost all the respondents experienced side effect(s) with the TB medication since commencement of treatment (97.1%) and among the respondents that experienced side effect(s), the common specific side effect(s) experienced were coloured urine (99.0%) and neuropathic signs (numb feet and hand) (55.6%). In a prior study, patients who experienced drug side effects were found to be significantly associated with medication non-adherence [22].
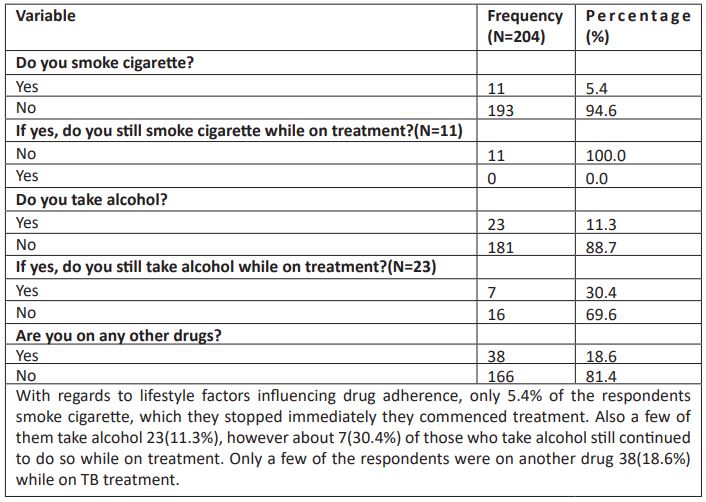
With regards to lifestyle factors influencing drug adherence, only 5.4% of the respondents smoke cigarette, which they stopped immediately they commenced treatment. Also a few of them take alcohol 23(11.3%), however about 7(30.4%) of those who take alcohol still continued to do so while on treatment. Only a few of the respondents were on another drug 38(18.6%) while on TB treatment. Tobacco smoking, alcohol and drug substances abuse was found to be a risk factor of TB treatment interruption and unsuccessful treatment [16,27-29,31].
From this study, majority of the respondents’ average waiting time in the clinic were less than an hour (95.6%) and in a prior study, poor adherence was significantly associated with prolonged waiting time at the health facility [29]. Structural or system factors includes the access to the health care facilities as found in some studies in Northeast Ethiopa, Plateau and Anambra State, Nigeria [29,32,17,18]. Majority of the respondents were observed by family members (73.0%) while taking their anti-TB medicines, however about a quarter of them were observed by no one (25.0%). Previous studies have reported lack of social or family support to be associated with non-adherence behaviour [27,30], however getting support from family or community were discovered to be protective factors for adherence to medication in some other studies [27,22,17]. All the respondents attested to the health workers as being very friendly to them which was in tandem with a previous study in Nigeria which reported that patient satisfaction towards care given by the healthcare workers at clinic were found to result in good adherence among the patients to take their medication correctly [22].
Conclusion
TB medication non-adherence is a potential risk factor for poor health outcomes such as drug resistance, relapse, and even TB patients’ deaths. From this study, almost all the respondents had good knowledge of tuberculosis; and adherence to anti-TB medications was good. Major reasons for missing medication among the non-adherent were that they forgot and that they were too much medication to take at once. Majority of the respondents were observed by family members while taking their anti-TB medicines, however about a quarter of them were observed by no one. All the respondents attested to the health workers as being very friendly to them. Despite the good adherence rate recorded in this study, more effort is needed to increase the rate of adherence.
Recommendations
- Since poor adherence to anti-TB medication is a strong risk factor for MDR-TB, interventions by the healthcare workers should be aimed at improving medication adherence among TB patients during the continuation phase especially. Such interventions could include health counselling, patient-specific drug education, multifaceted interventions that combine resilience and self-efficacy.
- Factors of health service delivery should be improved by the Federal ministry of Health to boost compliance and treatment outcomes among TB patients including reduction of patients waiting time at clinics as well as provision of more DOTS service points to address poor accessibility owing to long distance.
- Nurses and public health education experts at the community and health facility levels should implement a more intensive patient-specific education program to improve people’s knowledge of TB and its treatment such as the implementation of intensive public health education on TB treatment adherence, attenuation of factors that undermine TB medication adherence, and continual resource support for TB patients and DOTS program in all ramifications.
- The national DOTs service coordinators can also inform and influence policy decisions to employ more workers so as to reduce time spent with health workers while other DOTS providers should ensure direct observation of patients, adequate tracking, and follow-up to avoid relapse and failure cases.
Competing interests
The authors declare that they have no competing interests.
Financial support/ sponsorship
The authors declared that this study has received no financial support.
Ethical Considerations
This research work was done with approval from the Nnamdi Azikiwe University Teaching Hospital Health Research Ethics Committee (NAUTHHREC) through the Head of Department of Community Medicine, Nnamdi Azikiwe University, with ethical approval number NAUTH/CS/66/VOL.16/VER.3/198/2022/089. Verbal permission was sought from the head of the facility after the Ethical approval form gotten from NAUTHHREC were presented to the management. Participants were well oriented on the objectives of the study; verbal consent were sought prior to administration of the questionnaire which emphasized the right to non-participation. Data confidentiality were preserved according to the Helsinki declaration of bioethics.
Authors' Contributions
This work was carried out in collaboration among all authors. All authors read and approved the final manuscript.
References
- World Health Organization.Global tuberculosis report 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/250441/9789241565394-eng.pdf(Accessed February 12, 2023)
- Kumar V, Abbas AK, Aster JC. Robbins and Cotrane Pathological Basis of Disease. 9th Edition.New Delhi: Elsevier Limited. 2014: 381.
- Walker B,Colledge NR, Ralston S,Penman I. Davidson’s Principles and Practice of Medicine. 22nd Edition. Edinburgh:ElsevierHealth Sciences. 2014: 675-696.
- Giles HN, Lucas AO. A Short Textbook of Public Medicine for the Tropics and Sub-Tropics. 4th Edition. London:Arnold, A Member of the Hodder Headline Group. 2003: 159-163.
- Floyd K, Glaziou P, Zumla A, Raviglione M. The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. The Lancet Respiratory Medicine. 2018; 6(4): 299-314.
- World Health Organization. WHO Global End Tuberculosis Report 2020. Available from:https://www.who.int/publications/i/item/9789240013131[Accessed February 14, 2023].
- World Health Organization. Global Tuberculosis Report 2019. Available from: https://www.who.int/health-topics/tuberculosis/publications/global_ report_gtbr12_main. [Accessed February 14, 2023]
- Pawlowski A, JanssonM, Skold M, Rottenberg ME, Kallenius G. Tuberculosis and HIV Co-Infection.PLOS Pathogens. 2012; 8.
- Sunder LAP. Textbook of Community Medicine—Preventive and Social Medicine. 3rd Edition. New Delhi:CBS Publishers & Distributors. 2011: 420-431.
- Bam, TS, Chand, KB and Shrestha, SD. Factors responsible for non-compliance among TB patients in Kailali district, Nepal. Journal of Nepal Health Research Counci., 2005; 3(2): 51-7.
- Dogah E, Aviisah M, Kuatewo DM, Kpene GE, Lokpo SY, Edziah FS. Factors Influencing Adherence to Tuberculosis Treatment in the Ketu North District of the Volta Region , Ghana.Hindawi Tuberculosis Research and Treatment, 2021; 6685039(1-6). https://doi.org/10.1155/2021/6685039
- Danso E, Addo IY, Ampomah IG. Patients’ compliance with tuberculosis medication in Ghana: evidence from a periurban community. Advances in Public Health, 2015; 948487: (1-6).
- Mkopi A, Range N, Lwilla NF. Adherence to tuberculosis therapy among patients receiving home-based directly observed treatment: evidence from the United Republic of Tanzania. PloS one. 2012; 7(12): e51828
- Tola HH, Holakouie-Naieni K, Tesfaye E, Mansournia MA, Yaseri M. Prevalence of tuberculosis treatment non-adherence in Ethiopia: a systematic review and meta-analysis. The International Journal of Tuberculosis and Lung Disease. 2019; 23(6): 741-749
- Iweama CN, Agbaje OS, Umoke PCI, Igbokwe CC, Ozoemena EL, Omaka-Amari NL, et al. Nonadherence to tuberculosis treatment and associated factors among patients using directly observed treatment short-course in north-west Nigeria: A cross-sectional study. SAGE Open Med. 2021; 9: 205031212198949.
- Ajao KO, Ogundun OA, Afolabi OT, Ojo TO, Atiba BP, Oguntunase DO. Treatment compliance and challenges among tuberculosis patients across selected health facilities in Osun State Nigeria. Afr J Med Sci. 2014; 43: 21-29.
- Ubajaka CF, Azuike EC, Ugoji JO, Nwibo OE, Ejiofor OC, Modebe IA, et al. Adherence to Drug Medications amongst Tuberculosis Patients in a Tertiary Health Institution in South East Nigeria.International Journal of Clinical Medicine. 2015; 6 399-406.
- Ohamaeme MC, Ibeh CC, Emelumadu OF, Ezeama NN, Anyanwagu UC, Epundu U, et al. Assessment of the implementation of providers and patients adherence to Directly Observed Treatment Shortcourse (DOTS) strategy for Tuberculosis chemotherapy in Anambra State Nigeria. Afr J Med Allied Sci. 2019; 2(2): 29-53.
- History of saint Charles Borromeo hospital, Onitsha. Available from: https://web.facebook.com/1612945178983908/posts/about-st-charles-borromeospecialist-hospital-onitsha-limca-roadanambrastatenig/1971627419782347/?_rdc=1&_rdr(Accessed February 20, 2023)
- Geography of Onitsha South. Available from: https://citypopulation.de/php/nigeria-admin.php?adm2id=NGA004018 (Accessed February 20, 2023)
- Healthcare facilities/hospital in Nigeria. Available from: https://hfr.health.gov.ng/facilities/hospitals-list?page=198. (Accessed February 20, 2023)
- Sariem CN, Gyang SS, Tayo F, Auta A, Omale S, Ndukwe, HC. Factors Influencing Tuberculosis Medication Adherence in a Tertiary Health Institution in Nigeria. West African Journal of Pharmacy, 2013; 24(2): 66-75.
- Olawunmi OB. Factors Influencing Adherence to Tuberculosis Treatment among Dots Clinics Patients in Health Facilities in IJEBU Ode LGA, Ogun State, Nigeria. American Journal of Preventive Medicine and Public Health. 2020; 7(1): 158-70.
- Woimo TT, Yimer WK, Bati T. The prevalence and factors associated for anti-tuberculosis treatment nonadherence among pulmonary tuberculosis patients in public health care facilities in South Ethiopia: a cross-sectional study. BMC Public Health. 2017; 17(1): 269.
- Alobu I, Oshi SN, Oshi DC. Risk factors of treatment default and death among tuberculosis patients in a resourcelimited setting. Asian Pac J Trop Med. 2014; 7(12): 977-984.
- Kidenya BR, Mshana SE, Gerwing-Adima L. Drug adherence and efficacy of smear microscopy in the diagnosis of pulmonary tuberculosis after 2 months of medication in North-western Tanzania. Int J Infect Dis.,2017; 63: 43–47.
- Naidoo P, Peltzer K, Louw J, Matseke G, MchunuG ,Tutshana B. Predictors of tuberculosis (TB) and antiretroviral (ARV) medication non-adherence in public primary care patients in South Africa: a cross sectional study. BioMed Central Public Health. 2013; 13: 396
- Peltzer K, Pengpid S. Predictors of non-adherence to anti-tuberculosis patients in Thailand. Journal of Human Ecology. 2015; 52(2): 26-31.
- Tesfahuneygn G, Medhin G, Legesse M. Adherence to Anti-tuberculosis treatment and treatment outcomes among tuberculosis patients in Alamata District, northeast Ethiopia. BMC Research Notes. 2015; 8(503): 1-11.
- Fagundez G, Perez-Freixo H, Eyene J, Momo JC, Biyé L, Esono T, et al. Treatment Adherence of Tuberculosis Patients Attending Two Reference Units in Equatorial Guinea. PLoS ONE. 2016; 11(9): e0161995.
- Theron G, Peter J, Zijenah L, Chanda D, Mangu C, Clowes P, et al. Psychological distress and its relationship with non-adherence to TB treatment: a multicentre study. BioMed Central Infectious Diseases. 2015; 15(253): 1-12.
- Ibrahim LM,Hadejia IS, Nguku P, Dankoli R, Waziri NE, Akhimien MO, et al. Factors associated with interruption of treatment among Pulmonary Tuberculosis patients in Plateau State, Nigeria. 2011. Pan African Medical Journal. 2014; 17(78): 1-6.