Case report - Volume 3 - Issue 4
Transient ischemic mitral regurgitation caused by non-obstructive coronary lesion
Abhirami Shankar1*; Dali Fan2
1West Anaheim Medical Center, California, USA.
2UC Davis Medical Center, California, USA.
Received Date : June 26, 2023
Accepted Date : July 31, 2023
Published Date: August 07, 2023
Copyright:© Abhirami Shankar 2023
*Corresponding Author : Abhirami Shankar, West Anaheim Medical Center, California, USA.
Email: ashankar@sgu.edu
DOI: Doi.org/10.55920/2771-019X/1523
Abstract
Cases of transient ischemic mitral regurgitation caused by obstructive coronary artery stenosis have been reported in literature. But it can also be caused by non-obstructive coronary lesions. Diagnosis requires high suspicion and clinical acumen backed by a complete cardiac work-up that correlates with the timing of the coronary vasospasm.
Keywords: Obstructive; Stenosis; Plaque; Non-obstructive; Transient, Ischemia; Coronary; Vasospasm; Spasm; Mitral; Regurgitation; Papillary; Dysfunction; Angiogram, Valve; Replacement; Annuloplasty; Carpentier; Edwards.
Abbreviations
BPM- Beats Per Minute
CHF- Congestive Heart Failure Echo- Echocardiography/Echocardiogram
EKG- Electrocardiogram
HF- Heart Failure
HR- Heart Rate
LV- Left Ventricular
MR- Mitral Regurgitation
MV- Mitral Valve
MVA- Mitral Valve Annuloplasty
Case Report
81-year-old Tai female with a history of hypertension, non-occlusive coronary artery disease, atrial fibrillation and hyperthyroidism initially presented with urosepsis and pneumonia. She required intubation and was admitted to MICU. Once she recovered from the above infections with antibiotics and guideline directed therapy, she was transferred to the floors. However, she acutely decompensated and went into cardiogenic shock requiring reintubation. On physical exam, she appeared cachectic. She had bilateral crackles and coarse breath sounds in 2/3 lung fields and irregularly irregular heart sounds with Grade II/VI systolic murmur at the apex but no extremity edema. She was tachycardic in 110s. Labs were grossly unremarkable.
The patient had hypoxic respiratory failure likely secondary to flash pulmonary edema during her acute decompensation episode. Chest Xray showed pulmonary congestion and worsening right-sided pleural effusion. Bedside Echo was done that revealed 4+ MR, 1+ AI, both of which were not seen previously (Figure 1 and Video 1). EKG showed diffuse ST segment depressions (Figure 2). She underwent cardiac catheterization that did not show any ischemic cause for EKG findings (Figure 3). Cardiothoracic surgery was consulted; they declined surgical repair of her MR as they didn’t believe she was a good candidate due to the presence of too many comorbidities. She was medically managed but continued to require Dobutamine and Captopril to sustain her cardiac output. Subsequent repeat EKG 36 hours after presentation showed marked improvement in ST depression (Figure 4). Repeat Echo 44 hours and 90 hours since initial presentation showed resolution of mitral valvular abnormality and associated regurgitation (Figure 5, Video 2 and Video 3).
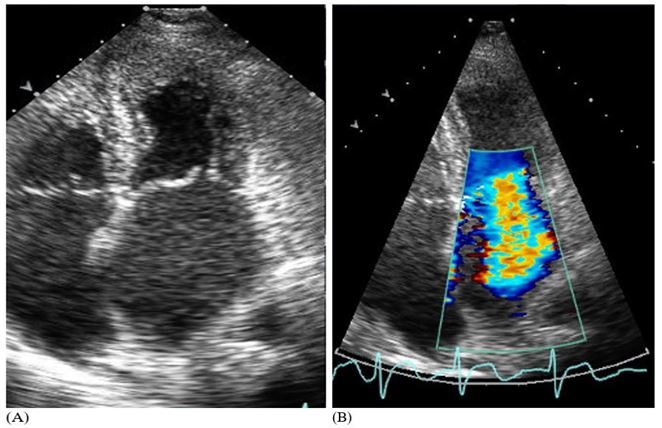
Figure 1: (A) Echo exhibited incomplete Mitral leaflet closure and coaptation along with akinesis and poor movement of the mitral valve. Transient ischemia from vasospasm can cause transient global subendocardial ischemia that in turn can cause mitral tethering and apical displacement of papillary muscles resulting in incomplete valve closure. (B) Same Echo showing severe MR (B).
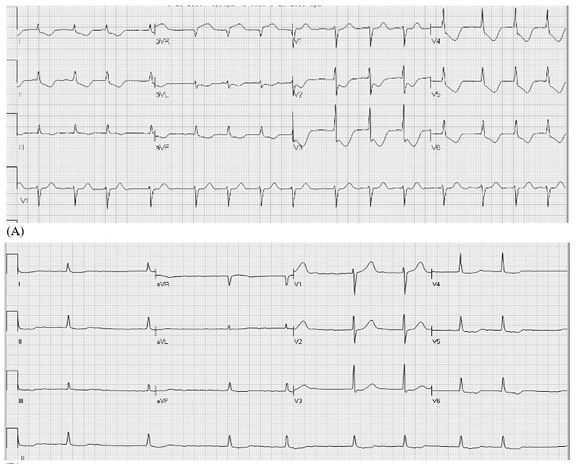
Figure 2: (A) EKG on presentation to the Cardiac team (B) EKG 12-hours prior to acute change in cardio-respiratory status.
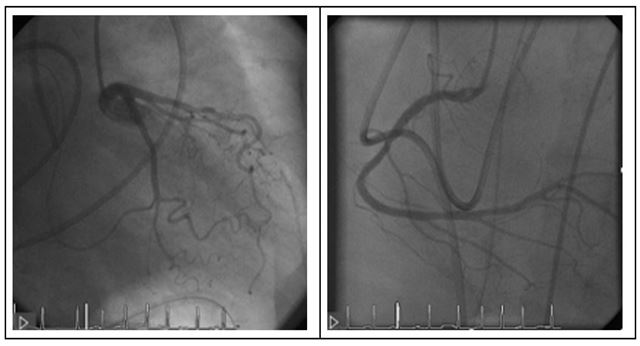
Figure 3: Angiogram revealing no significant coronary arterial occlusion.

Figure 4: Repeat EKG 36-hours after EKG in Figure 2(A). Notice marked improvement in previously present ST-depression.
While her MR resolved and patient initially improved, she then had no significant improvement of her clinical status after several days despite optimal therapy–possibly due to a recurrent attack of vasospasm and MR. She had ventilator dependent respiratory failure and persistently low cardiac index. Given her poor prognosis, her family decided to withdraw care. The patient expired 2 hours later.
Discussion
This patient’s transient severe mitral regurgitation (MR) was likely the result of a coronary artery spasm, causing transient ischemia induced papillary muscle dysfunction along with LV segmental akinesis. As the ischemia was relieved by medical treatment, the LV segmental akinesis resolved and papillary muscle function was restored, resulting in marked reduction of MR. These sequential events happened within a few hours of time. Coronary spasm is a distinct entity that is not well characterised, but is clearly different from plaque and demand ischemia. The patient had no angiographic evidence of significant obstructive diseases at the time of ischemic induced MR. She had a prior nuclear treadmill stress test (when her heart rate (HR) was as high as 140 bpm) with no perfusion defect. She also had atrial fibrillation with very rapid ventricular response (when her HR was as high as 170 bpm) without any significant ST-T changes on EKG. When she did have the ischemic attack (as supported by marked ECG ST-depression, severe MR and segmental LV wall motion abnormality in Echocardiography), her HR was only about 70 bpm. These characteristics are suggestive that coronary spasm (i.e., non-obstructive phenomenon) induced transient ischemia is an entity independent from demand ischemia or plaque rupture (i.e., obstructive event). The question still remains whether she should have benefitted from MV replacement as the intervention.
While there’s little literature about transient ischemic MR caused by non-obstructive lesions (viz. coronary vasospasm), such cases have still been documented. A retrospective study reviewed 6 patients with transient severe MR between 2006-2019 [1]. It was caused by 3 different processes—1) rate dependent LBBB and LV dyssynchrony 2) increased LV preload with transitory mitral annular dilation without change in coaptation angle and 3) intermittent coronary arterial spasm or microvascular dysfunction with apical leaflet tenting and low coaptation angle or incomplete leaflet coaptation, causing global myocardial ischemia which was reproducible with giving methergine [1]. Paroxysmal severe MR mostly presented as acute HF with pulmonary edema and patients with coronary vasospasm had ST segment depressions on EKG1. This was seen in 2 of the 6 studied patients (both women in their 60s, 1 had history of atrial fibrillation), who had resolutions of symptoms (dyspnea and acute HF) after treatment with diltiazem1.
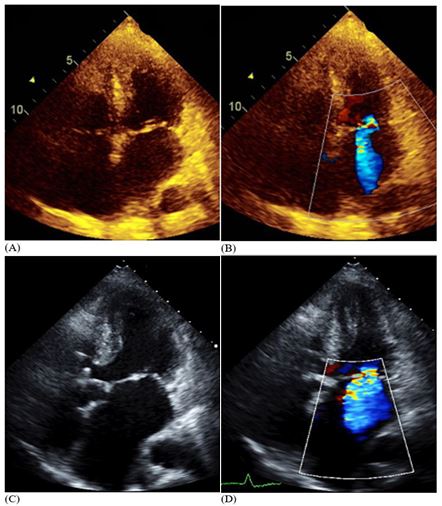
Figure 5: Repeat Echo 44 (A and B) and 90 (C and D) hours since the first one showed better movement, normokinetic mitral valve with normal coaptation with significantly reduced mitral regurgitation.
Another case reported coronary vasospasm causing transient severe MR in an 83-year-old female who presented with acute onset dyspnea, hypotension and significant ST depression on ECG, all of which normalised in minutes of nitroglycerin administration [2]. In a few days she re-developed hypotension and ST-depressions with elevated pulmonary arterial pressures [2]. Echo showed severe MR with no LV wall motion abnormalities [2]. This again resolved with nitroglycerin [2]. Repeat Echo showed trace MR [2]. She had previously been hospitalised multiple times for acute severe pulmonary edema but never had evidence of LV systolic dysfunction or valvular disease on Echo, and angiography showed clean coronaries [2]. Unfortunately, she had recurrence of similar episodes that initially responded to medical therapy with calcium channel blockers and nitroglycerin but was eventually refractory to medications [2]. She eventually died of shock and hemodynamic complications [2].
In another case, a 76-year-old male developed severe MR and associated CHF due to episodes of vasospastic angina [3]. Echo showed LV apical akinesis with ballooning and anterior mitral leaflet deformity causing inappropriate mitral coaptation and severe regurgitation [3]. An acetylcholine provocation test reproduced diffuse coronary spasm in distal right and left coronary arteries and associated severe MR [3]. Repeat Echo showed decreased MR with resolution of apical wall akinesis [3]. The patient’s coronary vasospasm remained refractory to anti-vasospastics and he had similar recurrent episodes [3]. Decision was made to perform Mitral valve annuloplasty (MVA) with a Carpentier-Edwards physio after which the patient had no further recurrence of MR despite having intermittent episodes of vasospastic angina [3]. MVA purportedly increases surface area for coaptation of mitral leaflets thus thwarting the tethering force [3]. The study concluded that MVA is a reasonable approach to patients with recurrent transient severe MR from coronary vasospasm, especially if refractory to medical therapy [3].
Conclusion
Our patient most likely had coronary artery spasm induced transient Severe MR, making it a unique presentation. Cases of transient ischemic MR chiefly caused by obstructive coronary artery stenosis have been reported in the world literature, while there’s few mentions of non-obstructive lesions causing transient ischemia and fleeting MR. It’s very difficult to diagnose as it requires a complete EKG, Echocardiogram and Angiogram data with precise timing to correlate with the coronary spasm ischemia induced transient reversible MR. More research is necessary to assess the benefit of MVA as an intervention for patients, especially with recurrent episodes.
Learning objectives:
- To recognize non-obstructive coronary lesions or coronary artery vasospasm as the culprit in transient ischemia and associated transient severe MR.
- To contemplate the benefit of MV replacement as treatment for patients with recurrent episodes and/or if refractory to medical therapy.
VIDEO LEGENDS
Video 1: Echo (correlating to Figure 1) showing severe MR due to mitral valve incompetence via incomplete leaflet closure and lack of coaptation. There is akinesia of the valve and papillary muscle displacement causing lack of appropriate closure of anterior and posterior valve leaflets.
Video 2: Echo (correlating to Figure 5A and 5B) obtained 44 hours since the first imaging. Mitral valve leaflets are normokinetic with improved leaflet coaptation and thus subsequent reduction of MR.
Video 3: Echo (correlating to Figure 5C and 5D) done 90 hours since the initial Echo. Note significant improvement in mitral regurgitation, better movement and closure of mitral valve leaflets and normal coaptation
References
- Breen TJ, Jain CC, Tan NY, Miranda WR, Nishimura RA. Paroxysmal severe mitral regurgitation. Mayo Clinic Proceedings. 2021; 96(1): 86-91. https://doi.org/10.1016/j.mayocp.2020.06.001
- Kaneko M, Ueda K, Nishimae I, Nitta S, Suzuki M, Kasao M, Shirai T. Subendocardial ischemia because of coronary artery spasm causes transient severe mitral regurgitation. Circulation: Heart Failure, 2018; 11(12). https://doi.org/10.1161/circheartfailure.118.005496
- Shimizu M, Kato Y, Matsukawa R, Masai H, Shima T, Miwa Y, Yamashita T, Okita Y. Recurrent severe mitral regurgitation due to left ventricular apical wall motion abnormality caused by coronary vasospastic angina: a case report. J Cardiol. 2006; 47(1): 31-7. PMID: 16475471.

