Case report - Volume 3 - Issue 4
Early vertebral artery thrombosis presenting as subclavian steal by virtue of windkessel and venturi effect
Abhirami Shankar*; Timothy S. Gibbs; Asaad Hakim
West Anaheim Medical Center, California, USA.
Received Date : June 26, 2023
Accepted Date : July 31, 2023
Published Date: August 07, 2023
Copyright:© Abhirami Shankar 2023
*Corresponding Author : Abhirami Shankar, West Anaheim Medical Center, California, USA.
Email: ashankar@sgu.edu
DOI: Doi.org/10.55920/2771-019X/1524
Abstract
Reversed flow in elastic vessels, especially if partially obstructed, is a common phenomenon. Spectral Doppler ultrasound
can assess underlying flow dynamics but is technician dependent and needs clinical correlation to avoid misdiagnosis.
Vertebral artery backflow can be explained by Windkessel effect, Venturi effect or true Steal syndrome.
Keywords: Dizziness; Vertigo; CVA; TIA; Stroke; Subclavian; Steal; Vertebral; Prevertebral; Carotid; Artery; Occlusion;
Stenosis; Obstruction; Clot; Thrombus; Deceleration; Retrograde; Antegrade; Flow; Reversal; Backflow; Velocity; Bunny;
Ultrasound; Doppler; Waveform; VTI; Compliant; Windkessel; Venturi
Abbreviations
CSVA- Cross Sectional Valve Area
CVA- Cerebral Vascular Accident
DAPT- Dual Antiplatelet Therapy
IAT- Intra-arterial thrombolysis
IVT- Intravenous Thrombolysis
ROM- Range of Motion
SA- Subclavian Artery
TEE- Trans-Esophageal Echocardiogram
TIA- Transient Ischemic Attack
VA- Vertebral Artery
VTI- Velocity Time Integrals
Case Report
A 56 y/o M presented with persistent dizziness and associated nausea, non-bloody emesis and diarrhea since the night before admission. He had generalised fatigue, right sided weakness and room spinning sensation unrelated to head position/movement. He experienced similar episodes the week prior partially relieved with rest. He denied hearing loss, recent upper respiratory tract infection, headache, fever, chills, or food poisoning.
Physical exam: AO*3. Bilateral nystagmus present, symmetric facial movements, normal speech, intact symmetric bilateral upper and lower extremity pulses, sensation, strength, ROM and reflexes with no focal deficits.
Past Medical History: Recently diagnosed hypertension and diabetes (on metformin), hyperlipidemia
Family History: CVA in sibling
Differential Diagnosis: Posterior CVA, TIA, central vertigo, Benign Positional Paroxysmal Vertigo, migraine, intracranial mass, multiple sclerosis, Meniere's Disease, Vestibular neuritis, Subclavian Steal, orthostatic hypotension.
Investigations:
Vitals: Temperature 97.1F, Heart Rate 90, Respiratory Rate 18, Blood Pressure 132/74 (Similar on both arms), SpO2 99% on room air
WBC 17, Hgb 15.3, Na 144, K 3.4, Glucose 210, CO2 25.1, BUN
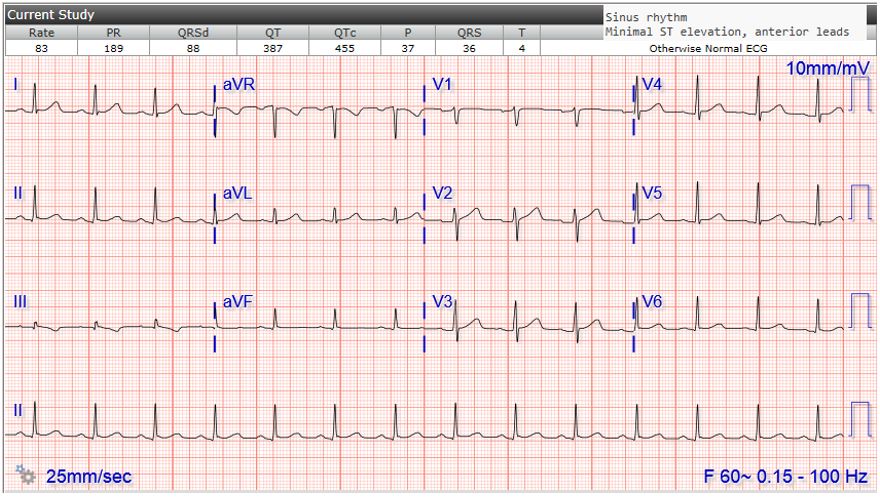
Figure 1: EKG showing sinus rhythm and nonspecific ST changes.
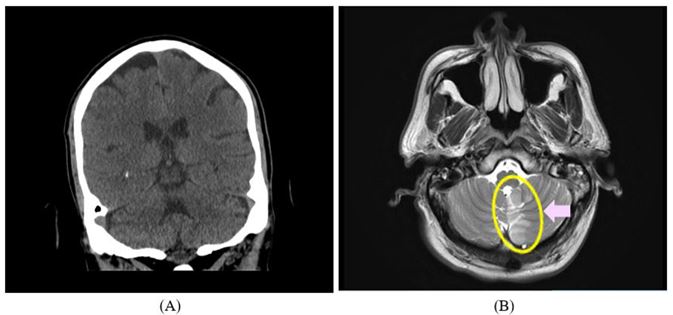
Figure 2: (A) CT Head (CVA not pictured); (B) MRI (sagittal) showing inferior-medial left cerebellar subacute CVA; Pink arrow showing area of encephalomalacia due to infarct.
Cr 20/1, Anion gap 13.9, Ca 8.6, lipase 155, HS Troponin 5 UA: 2+ ketones, 3+ glucose Urine Drug Screen: Negative TSH/free T4 and lipid panel: Within range EKG: Sinus (Image 1) CT Head: Small left superior cerebellar lucency, possible infarct, age uncertain. Mild microvascular disease with small left basal ganglia lacunar infarct (Image 2A)
Management
Neurology was consulted. The patient was started on continuous IV hydration, Aspirin, Atorvastatin, Meclizine and Ondansetron. Permissive hypertension was maintained and he had frequent neuro-checks. MRI showed subacute CVA involving inferior medial aspect of left cerebellar hemisphere (Image 2B). Plavix was added. While performing the Carotid US (Image 3A-3B), the Sonographer was suspicious of Steal syndrome with likely pre-vertebral arterial obstruction given higher peak flow velocity on the right vs the left vertebral artery (VA) and some left flow reversal. Subsequent CTA showed partial obstruction of the left VA-origin likely by a thrombus (Image 4A4D). Imaging results were discussed extensively with the Radiologist who confirmed presence of a partially occluding fresh proximal left VA thrombus close to the origin that could becausing reversed flow within the left VA. Interventional Radiology recommended transferring the patient to a stroke center with Neuro-interventional Radiology for further management. While waiting for transfer, he was continued on DAPT without anticoagulation. A follow-up Carotid Ultrasound (5 days after the first Ultrasound) was ordered to reevaluate the Steal phenomenon. Repeat ultrasound showed no detectable flow within the left VA– the thrombus size had increased, now with total left VA occlusion (Image 5, Image 6). TEE was negative for intramural thrombus.
Follow up
During hospitalisation, the patient continued to have unsteady gait but with otherwise overall improvement of his neurological symptoms. Stroke centre recommended continuing DAPT and discharging the patient home with outpatient neurology follow-up. Patient was discharged home on guideline directed medical therapy with appropriate outpatient follow-up.
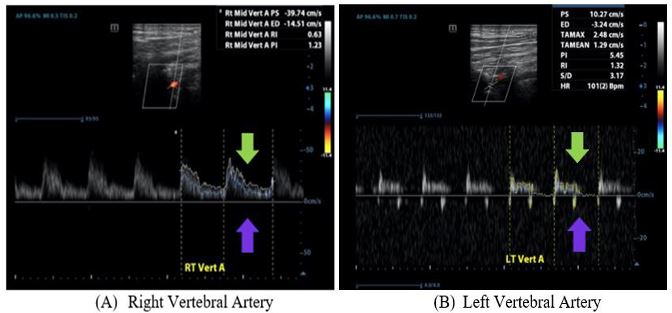
Figure 3: Vertebral arteries visualized during carotid doppler ultrasound study. Green and purple arrows are pointing to anterograde and retrograde flow respectively. In (A) there is higher peak flow velocity (39.74 cm/s) and no retrograde flow with normal waveform. In (B), the peak flow velocity is lower (10.27 cm/s) and there is some anterograde flow (possibly due to partial obstruction) and minimal “retrograde flow.
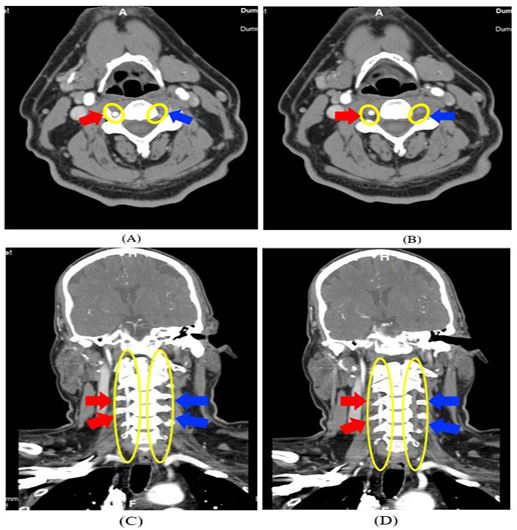
Figure 4: (A) and (B) CTA Head and Neck (sagittal) with left vertebral artery obstruction; (C) and (D) CTA Head and Neck (coronal)
showing left vertebral artery obstruction; Red arrows pointing to R vertebral artery with normal flow. Blue arrows pointing to absent flow representing likely obstruction of the L vertebral artery
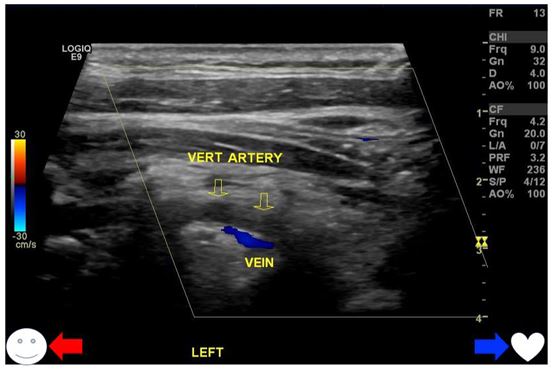
Figure 5: Repeat ultrasound showing total occlusion of L vertebral artery with absent flow. Red and blue arrows represent flow
direction towards the head and towards the heart respectively. Color Doppler demonstrates blood flow in the vertebral vein to the
heart (blue), but there is no flow in the vertebral artery just above the vein (which would appear red on Doppler if flow were present, indicating blood flow to the head).
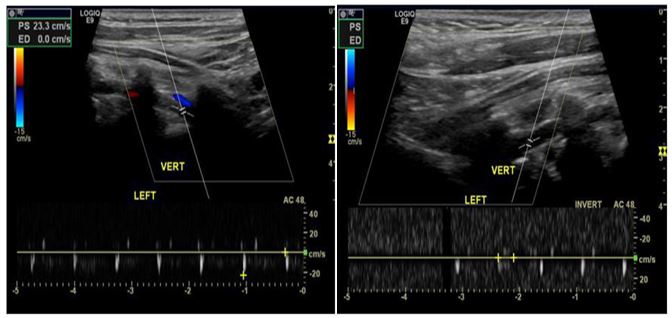
Figure 6: Repeat carotid ultrasound showing no anterograde flow in the left vertebral artery implying total obstruction. There’s
some reverberation due to arterial compliance and Windkessel effect appearing as contained minimal retrograde movement without continuous backward flow within the vertebral artery→ i.e., there is no subclavian “steal,” or stolen stream detected from the
vertebral artery to the subclavian artery. The form represents a blunt percussive form without visible continuous flow.
causing reversed flow within the left VA. Interventional Radiology recommended transferring the patient to a stroke center with Neuro-interventional Radiology for further management. While waiting for transfer, he was continued on DAPT without anticoagulation. A follow-up Carotid Ultrasound (5 days after the first Ultrasound) was ordered to reevaluate the Steal phenomenon. Repeat ultrasound showed no detectable flow within the left VA– the thrombus size had increased, now with total left VA occlusion (Image 5, Image 6). TEE was negative for intramural thrombus.
Follow up
During hospitalisation, the patient continued to have unsteady gait but with otherwise overall improvement of his neurological symptoms. Stroke centre recommended continuing DAPT and discharging the patient home with outpatient neurology follow-up. Patient was discharged home on guideline directed medical therapy with appropriate outpatient follow-up.
Discussion
Vertebral artery flow reversal has been long recognized [1] and can be explained by the phenomenon of Windkessel and Venturi effects. There’s always some degree of retrograde flow in compliant vessels that is increased in vasculature with plaque or obstruction [2]. Due to Windkessel effect, compliant vessels act as a blood reservoir in systole and impel stored blood during diastole along the path of least resistance [2] (usually forward) with some retrograde flow as the reservoir size and thus propelling force decreases. Using Hagen–Poiseuille equation, smaller vessel diameter from an obstruction/narrowing results in increased resistance, hindering anterograde propulsion. This causes a slightly higher backflow. Therefore, any partial obstruction in VA by a plaque/thrombus will cause some retrograde flow beyond the baseline flow reversal (from Windkessel effect within the VA); net backflow is more apparent with an obstruction rather than without. Venturi effect (VE) is a hydrodynamics principle explaining reduced hydrostatic pressure in high flow velocity regions [3]. By principle of mass continuity, fluid velocity (kinetic energy) increases when passing through a narrowing in a tube, while via Bernoulli’s principle this increase is paralleled by a decrease in static pressure (potential energy). When there is a stenosis of the subclavian artery (SA) proximal to VA origin creating a “natural” venturi tube system, the increased flow velocity to conserve momentum is balanced by a decrease in hydrostatic pressure in the vertical branch (vertebral artery) causing decelerated blood flow within the VA due to a reduced/negative
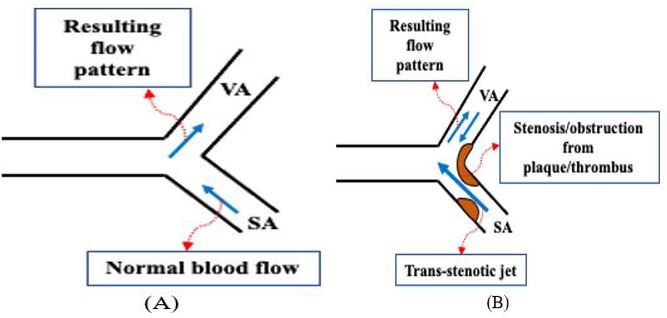
Figure 7: Right sided subclavian artery (SA) and vertebral artery (VA) flow dynamics in the presence (B) and absence (A) of narrowing. (B) Represents systolic blood flow deceleration within the VA during peak flow in SA from post-stenotic pressure loss causing
drop in VA flow velocity [6].
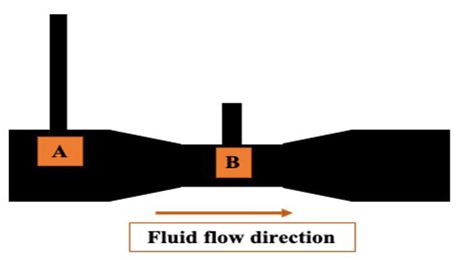
Figure 8: Venturi tube system. Flow velocity at B is greater than at A for the same quantity of fluid passing through these points at
a given time; and the height of the vertical branches represent the hydrostatic pressure in those regions [6].
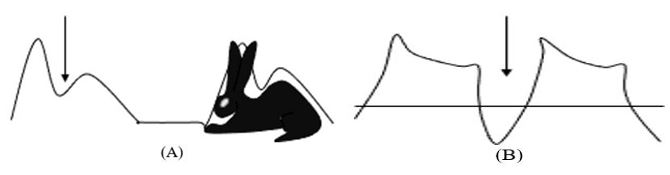
Figure 9: (A) Arrow showing mid-systolic velocity deceleration in vertebral artery. Pre-steal waveform seen as a “bunny” tracing.
(B) Pre-steal waveform now a complete steal form by marked mid-systolic dip and transient systolic flow reversal (wave below the
pressure system [3] – I.e., the stenotic area in SA or proximal VA causes a trans-stenotic jet prompting a Venturi effect on the branching VA due to a post-stenotic pressure loss resulting in VA flow deceleration (Image 7 and 8) [3]. Flow reversal similar to a collateral circuit occurs in extreme flow velocities in SA stenosis [6]. A study evaluating aortic arch blood flow velocities by TEE via color guided pulsed doppler showed that retrograde/antegrade flow velocity-time integrals (VTI) ratio was higher in patients with aortic plaque (and relatively higher in aortic arch than ascending/descending aorta) than without [2]. VTI*cross-sectional valve area (CSVA)=stroke volume; therefore, for the same stroke volume, VTI is higher in lower CSVA. Given VA is somewhat perpendicular to the SA without the “arch” component (thus distal VA obstruction wouldn’t need additional force for backflow as in distal aorta), there should be retrograde flow with higher VTI ratios in distal vs proximal obstruction. Although, variability in VA diameter, compliance, resistance and impedance compared to aorta should be accounted for. Carotid and vertebral waveforms on Spectral Doppler ultrasound can decipher underlying flow hemodynamics and likely associated disorders but requires clinical correlation to avoid misdiagnosis [4]. It can detect rapid signal loss or high-resistance flow demonstrating vertebrobasilar artery occlusion but is technician dependent [5]. High velocity systolic flow across VA origin due to stenosis of SA or proximal VA causes transient VA pressure drop and mid-systolic flow decline producing presteal waveforms on doppler ultrasonography [4]. This appears as the “bunny” waveform, with the trough depth correlating to degree of stenosis and associated velocity decline (Image 9A-9B) [4]. Intraluminal VA pressure and resistance depends on flow within VA and angle between distal VA and basilar artery [3]. For angle <90°, unusual flow in extracranial vessels insinuates proximal VA obstruction [6]. If angle >90°, it’s likely due to AV fistula [6]. A study investigated 43 participants with retrograde vertebral arterial flow on doppler ultrasound of which 16% had subclavian steal symptoms and 9% had hemispheric CVA symptoms [1]. 30% had no hemispheric CVA symptoms, of which ~9% had antegrade and retrograde flow in the vertebral artery, which was not seen in those with steal symptoms [1].
Conclusion
Vertebral artery occlusion can cause ischemia in the region
of proximal vertebrobasilar artery; if occlusion is extracranial
and close to the origin of VA, it usually causes medullary/cerebellar ischemia and occurs as a TIA [5]. Spectral Doppler ultrasound can detect rapid signal loss, high-resistance flow or
waveform changes to estimate underlying flow dynamics [5].
Systolic flow deceleration at VA-origin occurs due to SA/proximal VA obstruction, Windkessel effect and/or Venturi effect
from associated trans-stenotic pressure drop. VA retrograde
flow per se is benign, but depending on causality of reversed
flow patients will need appropriate intervention [1]. Treatment options are intravenous thrombolysis (IVT) or local intraarterial thrombolysis (IAT), endovascular thrombectomy and
ultrasonic fibrinolysis [5]. IVT attains recanalization in lower
percentage patients compared to IAT but is non-invasive and
readily available [5]. IAT doesn’t enhance outcomes despite
higher recanalization rates [5]. IAT is still first-line except in
time-sensitive cases where IVT is preferred [5].
Learning objectives:
1. To differentiate retrograde vertebral artery flow via physiologic phenomenon from true Subclavian Steal Syndrome.
2. To correlate Carotid doppler flow waveforms and velocities
in combination with clinical findings for more accurate diagnosis.
Conclusion
extracranial and close to the origin of VA, it usually causes medullary/cerebellar ischemia and occurs as a TIA [5]. Spectral Doppler ultrasound can detect rapid signal loss, high-resistance flow or waveform changes to estimate underlying flow dynamics [5]. Systolic flow deceleration at VA-origin occurs due to SA/proximal VA obstruction, Windkessel effect and/or Venturi effect from associated trans-stenotic pressure drop. VA retrograde flow per se is benign, but depending on causality of reversed flow patients will need appropriate intervention [1]. Treatment options are intravenous thrombolysis (IVT) or local intra-arterial thrombolysis (IAT), endovascular thrombectomy and ultrasonic fibrinolysis [5]. IVT attains recanalization in lower percentage patients compared to IAT but is non-invasive and readily available [5]. IAT doesn’t enhance outcomes despite higher recanalization rates [5]. IAT is still first-line except in time-sensitive cases where IVT is preferred [5].
Learning objectives:
- To differentiate retrograde vertebral artery flow via physiologic phenomenon from true Subclavian Steal Syndrome.
- To correlate Carotid doppler flow waveforms and velocities in combination with clinical findings for more accurate diagnosis.
References
- Nicholls SC, Koutlas TC, Strandness DE. Clinical significance of retrograde flow in the vertebral artery. Annals of Vascular Surgery. 1991; 5(4): 331-336. https://doi.org/10.1007/bf02015293
- Svedlund S, Wetterholm R, Volkmann R, Caidahl K. Retrograde blood flow in the aortic arch determined by transesophageal Doppler ultrasound. Cerebrovascular Diseases. 2008; 27(1): 22-28. https://doi.org/10.1159/000172630
- Ritter MA, Ringelstein EB. The Venturi effect and cerebrovascular ultrasound. Cerebrovascular Diseases. 2002; 4(2): 98-104. https://doi.org/10.1159/000064736
- Rohren EM, Kliewer MA, Carroll BA, Hertzberg BS. A spectrum of Doppler waveforms in the carotid and vertebral arteries. American Journal of Roentgenology. 2003; 181(6): 1695-1704. https://doi.org/10.2214/ajr.181.6.1811695
- Schoen JC, Boysen MM, Warren CR, Chakravarthy B, Lotfipour S. Vertebrobasilar artery occlusion. West J Emerg Med. 2011; 12(2): 233-9. PMID: 21691534; PMCID: PMC3099615.
- Ritter MA, Ringelstein EB. The Venturi Effect and Cerebrovascular Ultrasound. Cerebrovascular Diseases. 2002; 4: 98-104.

