Case report - Volume 3 - Issue 4
Homolateral and synchronic clear cell and papillary type of renal cell carcinoma – Diagnostic hints and review of literature
Surbhi Gupta Aggarwal1; Naman Aggarwal2; Shreya Garg3; Priya P S1*
1Department of Radiology, Kasturba medical college, Manipal academy of higher education, Karnataka, India.
2Department of Urology, Kasturba medical college, Manipal academy of higher education, Karnataka, India.
3Department of Pathology, Kasturba medical college, Manipal academy of higher education, Karnataka, India.
Received Date : June 03, 2023
Accepted Date : August 08, 2023
Published Date: August 21, 2023
Copyright:© Abhirami Shankar 2023
*Corresponding Author :Priya P S, Associate Professor, Department of
Radiology, Kasturba medical college, Manipal academy of higher education, Karnataka, India.
Email: docsurbhi2359@gmail.com
DOI: Doi.org/10.55920/2771-019X/1525
Abstract
Commonest solid mass of kidney is renal cell carcinoma, constituting 2-3% of all adult cancers. Synchronous malignant and
benign renal tumours bilaterally have been described in a few studies. However, homolateral and synchronic appearance
of malignant renal masses is extremely rare and there have been only a few case reports that had different subtypes of
malignant renal neoplasms of the same kidney on histopathology. In this report, we present a 66-year-old male patient
who had two different histological variants, ie, papillary RCC and clear cell RCC in his right kidney, and underwent radical
nephrectomy. Our aim is to provide radiological diagnostic hints and review the literature relevant to this rare case, as the
awareness of its occurrence can help in early diagnosis and deciding an appropriate management course.
Abbreviations: CT- Computed Tomography, USG- Ultrasonography, AML- Angiomyolipoma, RCC- Renal cell carcinoma, CCRCC- Clear cellrenal cell carcinoma, PRCC- Papillary renal cell carcinoma, PN- Partial nephrectomy, RN- Radical nephrectomy.
Introduction
Renal cell carcinoma (RCC) is the most common solid mass in the kidney constituting 2-3% of all adult cancers [1]. The most common subtype of RCC is clear cell (80%), besides papillary(10%) and chromophobe type RCC(5%) [2]. Common benign renal neoplasms include renal oncocytoma, angiomyolipoma (AML) and renal adenomas.
Data on ipsilateral synchronous clear renal cell carcinoma (CCRCC) and papillary renal cell carcinoma (PRCC) is insufficient. Therefore, they are often misdiagnosed preoperatively as a single primary malignancy with intrarenal metastasis or sometimes other benign masses. Hence, effective management might be affected because the two subtypes differ in prognosis [3].
Homolateral and synchronic appearance of renal tumours is extremely rare and there have been only a few case reports that had different subtypes of malignant renal neoplasms of the same kidney on histopathology. In this report, we present a 66-year-old male patient who had two different histological variants, ie, papillary RCC and clear cell RCC in his right kidney, and underwent radical nephrectomy. We also aim at providing radiological diagnostic hints and reviewed the literature relevant to this rare case.
Case report
A 66-year-old male patient presented t with complaint of right flank pain and was referred to the department of urology at KMC Hospital, Manipal. An ultrasound scan revealed a mass in the lower pole of the right kidney. No other mass was reported on USG. Subsequently, a CT scan was advised for characterisation of the mass, which revealed a well-defined hypoenhancing mass (relative to renal cortex) in the lower pole of right kidney, 4.4 x 3.4cm diameter, which was partially exophytic and not showing any fat/ calcification/ necrosis within. The CT scan also showed another smaller well defined arterially hyper-enhancing lesion (relative to renal cortex) measuring 1 x 0.9cm at the upper pole of right kidney. This lesion was not picked up on USG. A radiological diagnosis of renal cell carcinoma (likely papillary type) was given for the larger lower pole tumour, however, given the rarity of two histological subtypes in same kidney, a differential of lipid poor angiomyolipoma was given for the upper pole lesion. The physical examination of the patient was normal. Blood tests were also normal except a serum creatinine level of 1.58mg/dL and blood urea 23 mg/dL. The patient was a known hypertensive for 20 years. He had no other relevant previous medical history. The tumour was clinically diagnosed as probably RCC with metastasis and underwent radical nephrectomy. Surgery was uneventful and the patient discharged on post-op day three, with no significant complications. At six months and one-year follow-up, the patient was doing well with no evidence of recurrent disease.
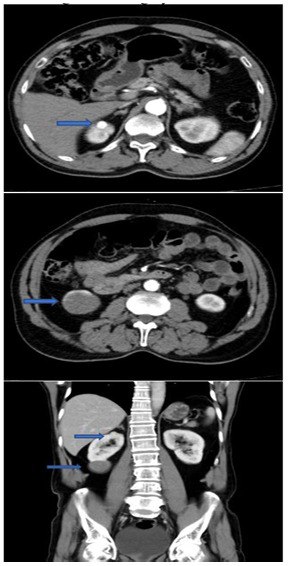
Figure 1: Contrast CT of the patient in the arterial phase. a. a hyper-enhancing solid lesion in the upper pole (arrow), b. a hypoenhancing solid lesion in the lower pole (arrow). c. Coronal view showing upper and lower pole lesions of the right kidney
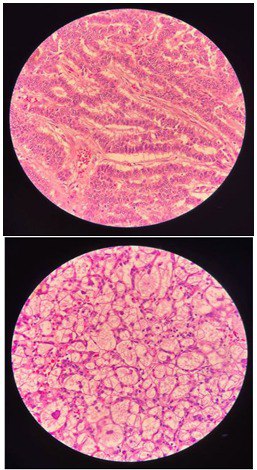
Figure 2: Postoperative histopathological examination showing microscopic images of a. Papillary RCC and b. clear cell RCC.
Discussion
Renal cell carcinoma (RCC) constitutes 2-3% of all cancers in adults [1]. The incidence of RCC has also risen over the past several decades due to incidental detection [4]. The most common subtype of RCC is clear cell (80%), besides papillary(10%) and chromophobe type RCC(5%) [2].
The most common etiological factors for RCC include smoking, obesity and hypertension [5]. Smoking is considered one of the key factors in the aetiology of RCC, with an increased dose-related risk. The relationship between hypertension/ obesity and RCC is not yet well established. Our patient had a long history of hypertension for almost 22 years.
Radiologically, Most CCRCCs are hypervascular solid masses, enhancing vividly in the early nephrographic phase with decreasing enhancement in the subsequent phases, showing fast in and fast out pattern. In contrast, PRCC are hypovascular solid masses which show hypoenhancement compared to renal cortex, there is no significant difference in the enhancement shown in the three phases of the PRCC during CT urography, as the vessels of its fibrovascular core are thin and sparse in the papillae [6].
Treatment recommendation includes surgical excision [7] [either radical nephrectomy (RN) or partial nephrectomy (PN)] for all localised RCCs [8]. Hence, during preoperative assessment, the presence of multiple tumours does not change the excision criteria. However, histopathologic evaluation may define different histological subtypes of tumours. RCC comprises several subtypes with specific histopathological characteristics, including clear cell, papillary, and chromophobe subtypes.
On pathological examination, CCRCC has clear cytoplasm with solid, cystic or tubular growth patterns. PRCC includes two subtypes: type 1 with small cells containing pale cytoplasm and type 2 with large cells and eosinophilic cytoplasm.
Sporadically occurring multifocal tumours have an incidence of 4-20% (9-12) at the time of diagnosis. Multiple synchronous renal masses may have a genetic predisposition to RCC, like hereditary familial RCC syndrome or acquired conditions, like chronic kidney disease, having a tendency to develop bilateral PRCC [13].
Sor-bellini et al. in their research estimated the prevalence of multifocal RCC and stated the incidence of ipsilateral multifocal RCC as 6.8% and bilateral RCC as 11.7% [14].
A study conducted by Muna Alhusban et al. stated that multiple ipsilateral synchronous RCC of different histological subtypes are a special entity and needs to be considered preoperatively even with low incidence rates [15].
A dataset including 97 patients presenting with multifocal renal masses [16]. They found 8 patients who had a mixed clear cell and papillary renal cell carcinoma, all of whom were treated with partial nephrectomy. Capaccio et al. [17] reported 7 patients with unilateral synchronous tumours with different histologic subtypes. 3 cases in their study had synchronous papillary and clear cell RCC and underwent radical nephrectomy. Ustuner et al. [18] also reported a case of a 67-year-old male who had clear cell and papillary RCC in the right kidney, that was successfully treated with radical nephrectomy.
Awareness of the coexistence of synchronous renal cell carcinoma of different histological subtypes within the same kidney is crucial in management, especially when planning for nephron-sparing surgery (NSS) and active surveillance for renal masses [19].
Studies by Blute ML and Minervini A, including a large sample size concluded that 5-6% of the patients with multiple ipsilateral renal tumours have a tendency to develop a contralateral metachronous recurrence, this risk being 5 times that of patients with a sporadic single tumour [19,20].
There is insufficient data to compare the different subtypes of RCC in the same kidney with bilateral multifocal or unifocal tumours in terms of survival or oncologic survey. Patel et al. [21] more recently found that malignant concordance was 89% among patients who had bilateral synchronous renal tumours. However, similar data on unilateral synchronous RCC of differing subtypes is lacking.
Hence, it is crucial for radiologists, urologists and pathologists to be vigilant of such cases during a solid renal mass workup. Additional therapeutic adjustments may be necessitated, derailing the initial treatment plan [22].
Conclusion
Our study reports an unusual case of homolateral synchronic clear cell and papillary type RCCs in the right kidney. The rarity of two simultaneous primary renal malignancies of varying histological subtypes in the same kidney merits reporting. The lack of awareness among the diagnostic and treating physicians may cause misleading preoperative diagnosis. Hence, it is crucial for radiologists, urologists and pathologists to be vigilant of such cases during the workup of a solid renal mass so that additional therapeutic adjustments can be made.
References
- Bray FF, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal AJ. Erratum: Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca Cancer J Clin. 2020; 70(4): 313.
- Ht C, McGovern FJ. Renal-cell carcinoma. N Engl J Med. 2005; 353: 2477-90.
- Yin J, Zheng M. Ipsilateral synchronous papillary and clear renal cell carcinoma: A case report and review of literature. World journal of clinical cases. 2022; 10(16): 5428.
- Alasker A, Williams SK, Ghavamian R. Small renal mass: to treat or not to treat. Current urology reports. 2013; 14(1): 13-8.
- Lipworth L, Tarone RE, McLaughlin JK. The epidemiology of renal cell carcinoma. The Journal of urology. 2006; 176(6): 2353-8.
- Tsuda K, Kinouchi T, Tanikawa G, Yasuhara Y, Yanagawa M, Kakimoto K, et al. Imaging characteristics of papillary renal cell carcinoma by computed tomography scan and magnetic resonance imaging. International journal of urology. 2005; 12(9): 795-800.
- Patel MI, Simmons R, Kattan MW, Motzer RJ, Reuter VE, Russo P. Long-term follow-up of bilateral sporadic renal tumors. Urology. 2003; 61(5): 921-5.
- Ljungberg B, Cowan NC, Hanbury DC, Hora M, Kuczyk MA, Merseburger AS, et al. EAU guidelines on renal cell carcinoma: the 2010 update. European urology. 2010; 58(3): 398-406.
- Richstone L, Scherr DS, Reuter VR, et al. Multifocal renal cortical tumors: fre- quency, associated clinicopathological features and impact on survival. J Urol. 2004; 171(2 Pt 1): 615-620.
- Dimarco DS, Lohse CM, Zincke H, Cheville JC, Blute ML. Long-term survival of patients with unilateral sporadic multifocal renal cell carcinoma according to histologic subtype compared with patients with solitary tumors after radical nephrectomy. Urology. 2004 ;64(3): 462-7.
- Lang H, Lindner V, Martin M, Letourneux H, Roy C, Saussine C, Jacqmin D. Prognostic value of multifocality on progression and survival in localized renal cell carcinoma. European urology. 2004; 45(6): 749-53.
- Baltaci S, Orhan D, Soyupek S, Bedük Y, Tulunay Ö, Göğüş O. Influence of tumor stage, size, grade, vascular involvement, histological cell type and histological pattern on multifocality of renal cell carcinoma. The Journal of urology. 2000; 164(1): 3 6-9.
- Breda A, Luccarelli G, Rodriguez-Faba O, Guirado L, Facundo C, Bettocchi C, et al. Clinical and pathological outcomes of renal cell carcinoma (RCC) in native kidneys of patients with end-stage renal disease: a long-term comparative retrospective study with RCC diagnosed in the general population. World journal of urology. 2015; 33(1): 1-7.
- Sorbellini M, Bratslavsky G. Decreasing the indications for radical nephrectomy: a study of multifocal renal cell carcinoma. Frontiers in oncology. 2012; 2: 84.
- Alhusban M, Alhamss S, Alzumaili B, Al-Daghmin A. Ipsilateral synchronous clear and papillary renal cell carcinoma: A case report and review of the literature. Urology case reports. 2018; 16: 110-3.
- Simhan J, Canter DJ, Sterious SN, Smaldone MC, Tsai KJ, Li T, Viterbo R, Chen DY, Greenberg RE, Kutikov A, Uzzo RG. Pathological concordance and surgical outcomes of sporadic synchronous unilateral multifocal renal masses treated with partial nephrectomy. The Journal of urology. 2013; 189(1): 43-7.
- Capaccio E, Varca V, Simonato A, Toncini C, Carmignani G, Derchi LE. Synchronous parenchymal renal tumors of different histology in the same kidney. Acta Radiologica. 2009; 50(10): 1187-92.
- Ustuner M, Yaprak B, Teke K, Ciftci S, Kart M, Yildiz K, Culha M. Coexisting papillary and clear renal cell carcinoma in the same kidney. Case Reports in Urology. 2014; 2014.
- Blute ML, Thibault GP, Leibovich BC, Cheville JC, Lohse CM, Zincke H. Multiple ipsilateral renal tumors discovered at planned nephron sparing surgery: importance of tumor histology and risk of metachronous recurrence. The Journal of urology. 2003; 170(3): 760-3.
- Minervini A, Serni S, Giubilei G, Lanzi F, Vittori G, Lapini A, Carini M. Multiple ipsilateral renal tumors: retrospective analysis of surgical and oncological results of tumor enucleation vs radical nephrectomy. European Journal of Surgical Oncology (EJSO). 2009; 35(5): 521-6.
- Patel AR, Lee BH, Campbell SC, Zhou M, Fergany AF. Bilateral synchronous sporadic renal tumors: pathologic concordance and clinical implications. Urology. 2011; 78(5): 1095-9.
- Symeonidis A, Tsikopoulos I, Symeonidis EN, Tsifountoudis I, Michailidis A, Tsantila I, et al. More than meets the eye: A case of synchronous ipsilateral clear cell renal cell carcinoma and urothelial carcinoma of the pelvicalyceal system and literature review. Acta Bio Medica: Atenei Parmensis. 2022; 92(6).

