Case report - Volume 3 - Issue 4
Groin foreign body in intravenous drug users: Case series
Srikant Agrawal1*; Jayaram Pandey2; Pratiksha Paudel3; Kumar Shrestha1; Dikshya Joshi1; Deepak Thapa Magar1; Dinesh Chapagain1; Kiran Shrestha1
1Bir Hospital, National Academy of Medical Sciences, Kathmandu, Nepal.
2Nepalese Army Institute of Health Sciences, Kathmandu, Nepal.
3B. P. Koirala Memorial Cancer Hospital, Bharatpur, Nepal.
Received Date : July 07, 2023
Accepted Date : August 10, 2023
Published Date: August 22, 2023
Copyright: © Srikant Agrawal 2023
*Corresponding Author: Srikant Agrawal, Department of Cardiothoracic and Vascular Surgery, National Academy of Medical Sciences,Kathmandu, Nepal.
Email: drsrikantag@gmail.com
DOI: Doi.org/10.55920/2771-019X/1527
Abstract
Introduction: Patients with a retained foreign body are a common scenario in healthcare setting. In patients who inject
drugs, chances of self-implantation are common. Retained foreign body may lead to cellulitis, deep tissue infections, sinus,
restriction of joint movements, necrotizing fasciitis, osteomyelitis or formation of a tumor-like mass.
Case series: We present cases of three male patients who presented with retained groin pain following intravenous drug
abuse. They underwent open inguinal exploration and retrieval of foreign body. No intra- or post-operative complications
were seen.
Conclusion: Strong suspicion of foreign body retention needs to be made in intravenous drug abusers who present with
groin pain. Early retrieval of the foreign body is recommended to prevent further dreaded complications.
Keywords: Retained foreign body, intravenous drug abuse, surgical retrieval, case series
Introduction
Patients with a retained foreign body are a common scenario in healthcare setting. The implantation can be accidental, selfinflicted or a part of a self- embedding procedure. Foreign body retained for a prolonged duration may complicate to cellulitis, deep tissue infections, sinus, restriction of joint movements, necrotizing fasciitis, osteomyelitis or formation of a tumorlike mass [1]. Foreign bodies may be ingested, inserted into
body cavities or may enter the body by penetrating injury or iatrogenically. Among penetrating injuries, intravenous drug use is considered to be a world-wide problem responsible for numerous minor to life-threatening and fatal complications. Intravenous drug abusers use peripheral veins as the route for injecting drugs. Once the peripheral veins get sclerosed, the drug abusers resort to shooting in the groin which is termed as “groin hit” for the access to femoral vein [2]. Likewise, the chances of self-implantation while trying to inject the drug in the femoral vein in the thigh is common in patients who inject drugs (PWIDs).
Case Presentation
Herein, we report three cases of foreign body (needle fragment) retentions over groin in young patients who injects drugs.
Case 1
A 22 year male presented with pain over left groin for 7 days and burning sensation in left lower limb following self inflicted needle prick injury over left groin region 7 days back. He had been using intravenous drugs for the last 2 years. His vital signs were stable with unremarkable findings on general examination. On local examination of left lower limb, there was a black spot over left inguinal crease which was tender on palpation. There was no obvious swelling and local temperature was not raised. Distal neurovascular status was intact. Baseline investigations were within normal limits. Ultrasonography of lower limb did not show any foreign artifact. CT angiography of bilateral lower limb showed well defined hyperdense linear lesion likely metallic foreign body in left groin, just medial to femoral vein (Figure 1).
Case 2
A 36 year male presented with pain over left groin following a self-inflicted needle prick in left groin for 5 days. He gives history of intravenous drug abuse for the last 6 months. On
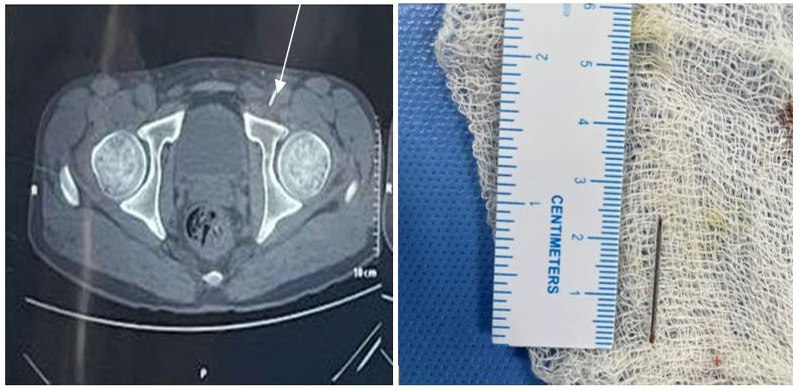
Figure 1 and 2: He underwent left inguinal exploration under subarachnoid block with intraoperative findings of metallic foreign body (needle tip) approx. 2.5cm in length, just medial to left femoral vein (Figure 2).

Figure 3 and 4: He underwent left inguinal exploration under spinal anesthesia .Intraoperative findings were approx. 20mm long metallic foreign body (needle tip) in left inguinal region, just lateral to saphenous vein in muscular plane
local examination of the left lower limb, there was a puncture mark on the left inguinal region with palpable nodular structure underlying the puncture site. Left inguinal lymph node was enlarged. Baseline investigations were within normal limits. Ultrasonography of left groin showed metallic artifact at great saphenous vein- common femoral vein junction. CT angiography of bilateral lower limb showed well defined hyperdense linear lesion likely metallic foreign body in left groin, just lateral to femoral vein anterior to pubic bone (Figure 3, 4).
Case 3
A 25 year male presented with pain and swelling in right groin for 1 month following self inflicted needle prick. He had been using intravenous drug since 1 year. On local examination of the right groin, 2X2 cm fluctuant swelling was present over the right femoral region. Pointed metallic object was felt in the
swelling with localized tenderness. However, local temperature was not raised. Baseline investigations were within normal limits. CT angiography of bilateral lower limb showed a linear metallic foreign body in right groin just anterior to femoral vein (Figure 5). All the patients had uneventful postoperative recovery and were discharged on second postoperative day. On follow up after a month, no fresh issues were seen.
Discussion
The prevalence of needle fragment retention in people who inject drugs (PWIDs) is unknown as there are no studies of representative populations described in the literature. In 2002, Norfolk and Gray stated that 14 of 70 (20%) PWIDs, held in Bristol police custody reported a total of 23 broken needles during their injecting history and noted that the majority (61%) of the broken needles had been re-used [3]. Subcutaneous needle retention in PWIDs commonly causes local symptoms such as
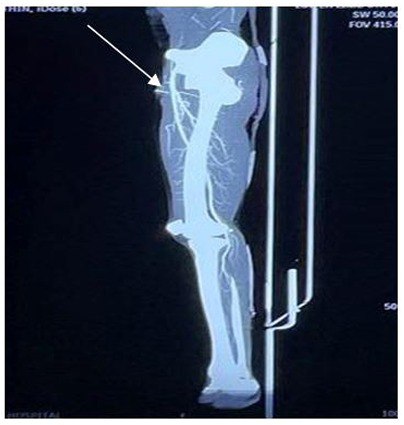
Figure 5: He underwent exploration of the right inguinal region and a 4cm linear needle in the subcutaneous plane was found intraoperatively.
pain and infections. Additionally, previous case reports have described serious complications from broken needles, including needle embolisms in the brain, heart, or lungs [4,5]. Faulty or damaged needles, hardened veins associated with chronic inflammation or sudden movement at the injection site are the possible causes of needle breaking [1–3]. Broken needles are less likely if PWIDs always use a fresh needle and avoid injecting into a site where the skin and veins are hardened through frequent use. Repeated injection of drugs damages veins, leading to vein sclerosis [3]. Consequently, due to damaged and inaccessible peripheral veins, some PWIDs turn to central veins such as those of the groin and neck, and they sometimes even inject in subcutaneous region or muscle tissues [3]. Indeed, patients with needle retentions near central veins are likely to have a prolonged drug use history. When a PWID presents with local pain (or inflammation) in an injection area, clinicians should think about the possibility of fragmented needles. To avoid a needle stick injury, clinicians should be aware that retained needles can be asymptomatic. In addition, a needle fragmentcan be a subtle incidental finding in imaging examinations and thus can be easily overlooked if the examiner is unaware of the patient’s background. It is therefore important that the individual’s intravenous drug use is disclosed when referring the patient for radiological examinations. Depending on the orientation and depth of the needle in the tissue, needle fragments may not always be identifed using ultrasound [6], as the first case demonstrated. CT angiography is most reliable in identifying the foreign body in relation to vessels and aids in definitive management. Nonetheless, the benefit of removing a needle fragment that causes local symptoms must be balanced against possible harms (such as operation-related risks, possible complications, and the risk posed to the surgical staff if the patient is infected with human immunodeficiency virus or viral hepatitis). We empirically suggest that, in addition to managing the fragmented needle, clinicians should educate PWIDs of the services available to them as well as to seek medical help when needed.
Conclusion
High suspicion of foreign body retention should be made in young patients with history of intravenous drug abuse who present with groin pain. Early retrieval of needle fragment reduces the risk of further dreaded complications.
Conflicts of Interest: None.
Ethical Approval: Not applicable.
Consent to Participate: Not applicable.
Consent for publication: The patients give us their consent for this publication.
Availability of data and material: The data and material have been used and disseminated legally and transparency.
Code availability (software application or custom code): Not applicable.
Ethical Approval: All the authors approved the manuscript and his contents.
Funding: The authors have not received any financial support for this publication.
Acknowledgement: Consent has been taken from the patients for publication of this case series
References
- Del Giudice P. Cutaneous complications of intravenous drug abuse. Br J Dermatol [Internet]. 2004; 150(1): 1-10. Available from: https://pubmed.ncbi.nlm.nih.gov/14746612/
- Roszler MH, McCarroll KA, Donovan KR, Rashid T, Kling GA. The groin hit: complications of intravenous drug abuse. Radiographics [Internet]. 1989; 9(3): 487-508. Available from: https://pubmed.ncbi.nlm.nih.gov/2727357/
- Norfolk GA, Gray SF. Intravenous drug users and broken needles--a hidden risk? Addiction [Internet]. 2003; 98(8): 1163-6. Available from: https://pubmed.ncbi.nlm.nih.gov/12873251/
- Nérot A, Bing F. Acute stroke secondary to intracranial arterial needle migration. Neurology [Internet]. 2020; 94(19): 841-2. Available from: https://n.neurology.org/content/94/19/841
- Waidyanatha S, Sekhsaria S. Left ventricular perforation from a dislodged needle migrating via a pulmonary artery branch in an intravenous drug user. BMJ Case Reports CP [Internet]. 2021;
14(1): e237333. Available from: https://casereports.bmj.com/ content/14/1/e237333 - Kiely J. The use of ultrasound guidance for foreign body removal. J Plast Reconstr Aesthet Surg [Internet]. 2019; 72(5): 848-62. Available from: https://pubmed.ncbi.nlm.nih.gov/30579905/

