Research Article - Volume 3 - Issue 4
Bouveret’s syndrome in a young, stable patient: Clinical case report and summary of evidence
Ana Victoria Espinosa de los Monteros-González*
General Surgery Department, High Specialty Medical Unit “Centro Médico Nacional de Occidente Lic Ignacio García Téllez”. Mexican Institute of Social Security. Guadalajara, Jalisco, Mexico
Received Date : July 07, 2023
Accepted Date : August 11, 2023
Published Date: August 23, 2023
Copyright:© Qusay Abdoh 2023
*Corresponding Author : Ana Victoria Espinosa de los Monteros Gonzalez, General Surgery Department. High Specialty Medical Unit “Centro Médico Nacional de Occidente Lic. Ignacio García Téllez”. Mexican Institute of Social Security. Belisario Dominguez St 1000, Guadalajara, Mexico. 44329.
Email: ana.espinosam@alumno.udg.mx
DOI: Doi.org/10.55920/2771-019X/1529
Abstract
Bouveret’s syndrome is an infrequent cause of bowel obstruction, and the less frequent presentation form of gallstone ileus with high mortality. Only 315 cases have been reported until 2016. Given the scarce number of cases, there is no consensus on the appropriate management. We present the case of a middle-aged Mexican woman referred to a high specialty surgical center with imaging evidence of duodenal calculus and bilioenteric fistula. A 10 x 5 cm gallstone impacted in the duodenum was removed via an open anterior gastrotomy. She had good postoperative course. Each case should be treated based on patient’s health status, location and size of the gallstones as well as experience and availability of minimally invasive techniques.
Keywords: Bouveret’s syndrome; Gallstone disease; Cholecystoduodenal fistula; Gastrotomy; Gallstone ileus; Gastric outlet obstruction; Hepato-Pancreato-Biliary surgery
Background
Gallstone ileus occurs in only 0.3-0.5% of patients with cholelithiasis. The most common site of obstruction is the distal ileum, but, in 1-3% of patients, it occurs at the duodenal bulb or pylorus. This is known as Bouveret´s syndrome after the publication by French physician Leon August Bouveret in 1896 [1]. Better diagnostic and surgical techniques have reduced mortality, but still remains as high as 12% [2]. Surgical procedure selection is controversial. We present the case of a middleaged woman referred to a Hepato-Pancreato-Biliary surgery center in Mexico with radiologic and endoscopic identification of calculus in the duodenum with cholecystoduodenal and cholecystocolonic fistula requiring urgent intervention with satisfactory postoperative outcome.
Case presentation
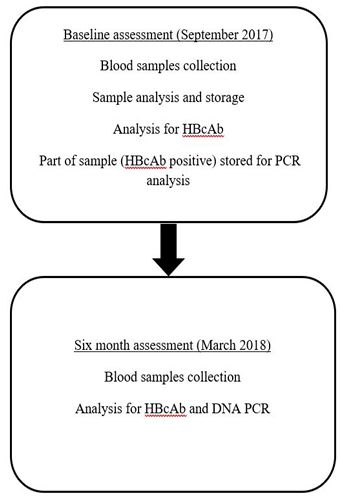
A 54-year-old Mexican women presented to a regional hospital with 2 week colicky abdominal pain accompanied by persistent nausea and vomiting that completely prevented oral intake. The patient did not refer chronic diseases. Eight months prior to admission, she was diagnosed by a private practitioner with cholelithiasis and started on protocol for elective cholecystectomy. On initial evaluation, she was non-icteric, with tenderness and a palpable mass in the right-upper quadrant. Vital signs and laboratory tests including blood cell count, glucose, creatinine, electrolytes and procalcitonin were within normal ranges. Liver biochemical tests also showed no abnormalities (total bilirubin 0.73 mg/dl, direct bilirubin 0.47 mg/dl, AST 17 U/L, ALT 9 U/L, alkaline phosphatase 67 U/l). An oral contrastenhanced CT reported pneumobilia, and a 36x69 mm calculus in the second duodenal portion with cholecystoduodenal and cholecystocolonic fistula (Figure 1). At endoscopy, an obstructive reddish tissue with a yellowish surface in antrum suggestive of erosion was observed (Figure 2). She was started on parenteral nutrition and referred to our unit for evaluation by a hepato-pancreato-biliary surgeon. She was taken for exploratory laparotomy, finding firm adherences from the gallbladder to the duodenum and transverse colon, a cholecistoduodenal and cholecistocolonic fistula with a 10 cm x 5 cm gallstone impacted in duodenum (Figure 3). Calculus was removed through an anterior gastrotomy which was then closed in one plane with Connel-Mayo stitches. A nasojejunal tube was placed distal to the fistula for enteral nutrition. On postoperative day 10 oral the water-soluble con-
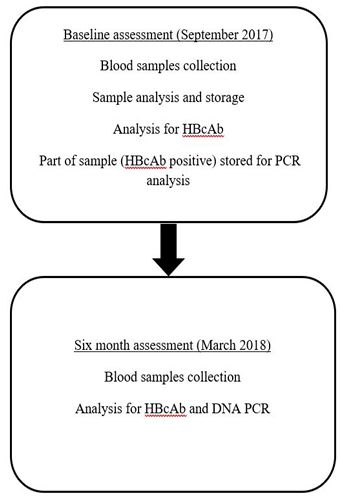
Figure 1: Computed Tomography with oral contrast evidencing pneumobilia, duodenal calculus, and hepatic hypodensity in segments IV, V and VI with cholecystoduodenal and cholecystocolonic fistula. A) Coronal B)Axial.
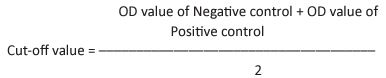
Figure 2: EGD evidencing calculus in duodenal bulb.
Discussion
Bouveret’s syndrome has a 1.9 to 1 female predominance and, different from our case, a median age of presentation of 74 years [3]. Indeed, in patients older than 65 years it explains 25% of non-hernia intestinal obstructions [4]. The most common cause is a fistula between the gallbladder and the digestive tract due to wall necrosis with recurrent inflammation, most commonly of the choledocoduodenal type
(60%) [4]. Multiple fistulas, as in our case, have not been previously documented. Symptoms and laboratory findings tend to be unspecific and imaging studies are necessary for differential and definitive diagnostic. Computed tomography has the best diagnostic performance, identifying the ectopic stone in 81.48% [4] of cases. Magnetic resonance imaging can unveil issoatenuating calculi, but it is less accessible in an urgent scenario. In endoscopy, the gallstone is directly observed in two-thirds of examinations [2]. In 20-40% of cases, the diagnosis is made during surgical exploration [3]. Endoscopic extraction has a 1.6% risk of complications [3].
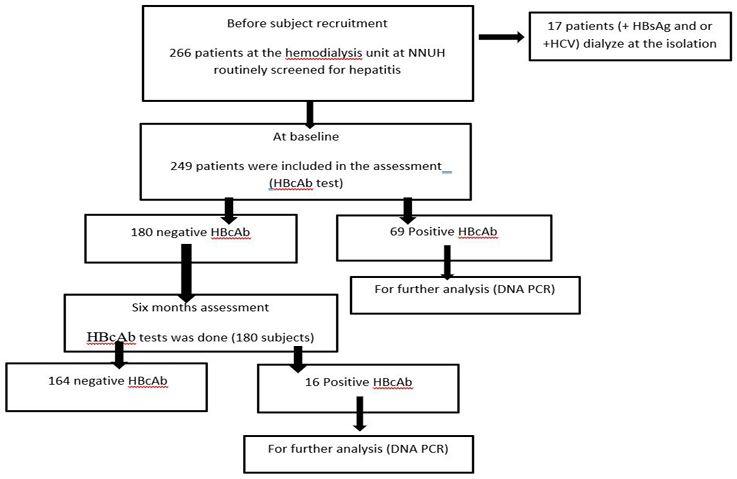
Figure 4: Adapted from Ong J, et al. Bouveret syndrome: A systematic Review of Endoscopic Therapy and a novel predictive tool to Aid in Management. J clin Gastroenterol. 2020;54(9). Score 0.86 has a 95% confidence interval (0.79-0.94). Lower scores are associated with lower probability endoscopic success. EHL: Electrohydraulic lithotripsy; ESWL: Extracorporeal shock wave lithotripsy; LL: Laser lithotripsy; ML: Mechanical lithotripsy.
Figure 5: Treatment summary Diagram.
compared to 17.3 to 25.9% with open surgery [5]. However, it has failed to prove superior. The greatest review of endoscopic interventions by Ong et al., which included 164 cases, found that 60.5% required salvage surgery. They proposed a formula to assess pretest probability of success based on 3 variables with a cutoff value of 0.86, but it has not yet been validated [5]. According to this score, there was only 10% or less probability of endoscopic treatment success due in our case to disfavourable size and unavailability of lithotripsy techniques despite accessible location (Figure 4). During surgical extraction via enterolithotomy or gastrotomy, proper direction of closure is important to prevent stenosis and complete examination of the small bowel to exclude additional stones, which are identified in 16% of cases [6]. Extraction alone has the lowest morbidity and mortality [5]. However, incidence of recurrence is 17%. The high risk of choledocolithiasis (17%) and gallbladder carcinoma (15%) [7] is also of concern, although this latter association is not clear. Some studies have found that delay in diagnosis is more relevant for postoperative results than surgical time [4]. Therefore, in young and stable patients, a single-stage cholecystectomy should be offered, but in case of adhesions and friability of tissues a two-stage approach might be preferable, as we decided in this patient. Figure 5 summarizes recommendations for treatment decisions.
References
- Qasaimeh GR, Bakkar S, Jadallah K. Bouveret’s Syndrome: An Overlooked Diagnosis. A Case Report and Review of Literature. Int Surg. 2014; 99. https://doi.org/10.9738/INTSURG-D-14-00087.1.
- Nickel F, Müller-Eschner MM, Chu J, Von Tengg-Kobligk H, MüllerStich BP. Bouveret’s syndrome: Presentation of two cases with review of the literature and development of a surgical treatment
strategy. BMC Surg. 2013. https://doi.org/10.1186/1471-2482- 13-33. - Haddad FG, Mansour W, Deeb L. Bouveret’s Syndrome: Literature Review. Cureus. 2018. https://doi.org/10.7759/cureus.2299.
- Chica LFÁ, Cuéllar WB, Cardozo OLR. Íleo biliar y síndrome de Bouveret. Lo mismo pero distinto descripción de dos casos y revisión de la literature. Rev Colomb Gastroenterol. 2010; 25.
Ong J, Swift C, Stokell BG, Ong S, Lucarelli P, Shankar A, et al. Bouveret Syndrome: A Systematic - Review of Endoscopic Therapy and a Novel Predictive Tool to Aid in Management. J Clin Gastroenterol. 2020; 54. https://doi.org/10.1097/ MCG.0000000000001221.
- Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. American Journal of Gastroenterology. 2002. https://doi.org/10.1016/S0002-9270(01):04013-8.
- Bouveret’s Syndrome: An Extensive Summary of the Literature. Archives of Gastroenterology Research. 2020. https://doi. org/10.33696/gastroenterology.1.009.

