Case report - Volume 3 - Issue 4
Kartagener Syndrome: Three rare cases report and systematic review
Cong Nguyen Hai1*; Cam Truong Dinh2; Loi Trinh Duc1; Thang Tran Quyet3
1Department of Tuberculosis and Respiratory Pathology, Military Hospital 175, Ho Chi Minh City, Vietnam.
2Military Hospital 175, Ho Chi Minh City, Vietnam.
3Department of Radiology, Military Hospital 175, Ho Chi Minh City, Vietnam.
Received Date : July 17, 2023
Accepted Date : Aug 16, 2023
Published Date: Aug 25, 2023
Copyright: © Cong Nguyen Hai 2023
*Corresponding Author : Cong Nguyen Hai, Department of Tuberculosis and Respiratory Pathology, Military Hospital 175, Ho Chi Minh City, Vietnam.
Email: nguyen_med@ymail.com
DOI: Doi.org/10.55920/2771-019X/1533
Abstract
Kartagener Syndrome (KS) is a rare genetic disorder characterized by defects in ciliary motility, affecting multiple organs and characterized by the presence of a triad of abnormalities: bronchiectasis, chronic sinusitis, and situs inversus. Most patients with this syndrome are infertile. In this report, we present three cases of KS, including two males and one female. Although they all have KS, there are differences in clinical features and disease progression. We describe the clinical symptoms, disease progression, and provide an overview of the literature.
Keywords: Kartagener syndrome; primary ciliary dyskinesia; ciliary dysfunction; infertility in males; chronic sinusitis; bronchiectasis; situs inversus
Introduction
Kartagener syndrome (KS) belongs to the group of primary ciliary dyskinesia (PCD), which are a spectrum of genetic disorders. It is an autosomal recessive condition. PCD is characterized by chronic upper and lower respiratory tract disease, infertility/ectopic pregnancy, and situs anomalies, that occur in 50% of PCD patients (Kartagener syndrome), and these may be associated with congenital heart abnormalities [1]. The clinical hallmark of KS is the presence of the triad of bronchiectasis, chronic sinusitis, and situs inversus [2,3,4]. The syndrome was first described by Siewart in 1904, and Kartagener later recognized the correlation between these three factors and reported four cases in 1933. The estimated prevalence of KS is approximately 1/30,000 individuals, with a range of 1/12,500 to 1/50,000 [4].
The normal ciliary function is crucial for respiratory tract protection, sperm motility, and appropriate organ positioning during embryonic development. In KS, mutations in DNAI1 and DNAH5 genes result in impaired ciliary motility, leading to recurrent lung infections, chronic sinusitis, infertility, and situs inversus [5,6]. Chronic respiratory failure with elevated CO2 levels commonly occurs in the later stages and is a major cause of death in patients with KS. However, the progression of lung function decline can vary depending on various factors. In this report, we present three clinical cases of KS admitted to the hospital due to respiratory infections, highlighting the differences in clinical features and disease progression.
Case description
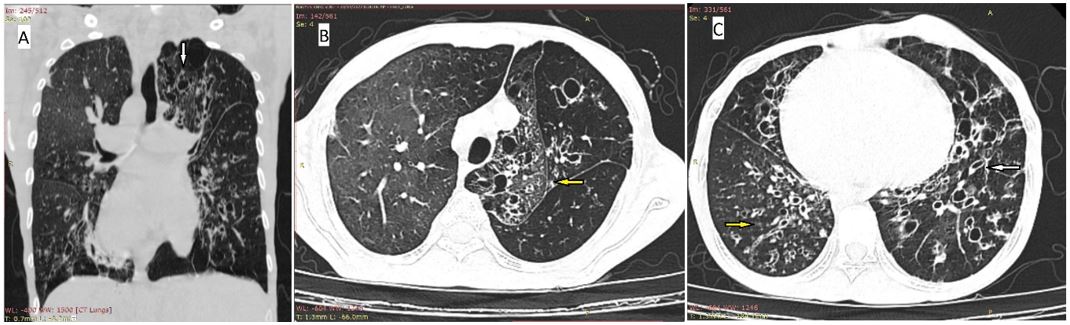
Case 1: The patient is a 34-year-old non-smoking male with a thin physique (BMI of 17.7). He had a history of recurrent respiratory tract infections since childhood, presenting with symptoms such as a runny nose, productive cough with purulent sputum, and varying degrees of fever. These symptoms often improve after a course of antibiotics, anti-inflammatory drugs, and expectorants, but tend to recur under favorable conditions such as weather changes. The patient began experiencing shortness of breath with exertion at the age of 24. Upon examination and diagnosis, he was found to have KS. In the following years, the patient has had frequent hospital admissions for severe lower respiratory tract infections. Bacterial culture of bronchoalveolar lavage fluid revealed growth of multidrug-resistant bacteria such as Streptococcus agalactiae and Pseudomonas species. The degree of shortness of breath has progressively worsened over time, and currently, the patient experiences difficulty breathing even with mild daily activities. Blood gas analysis indicates chronic respiratory failure, with elevated blood CO2 levels since the patient was 32 years old. Particularly, the patient got married at the age of 27 but has not been able to conceive a child. He has undergone semen analysis, which showed a decrease in sperm count and motility. The chest CT showed dextrocardia and extensive tubulocystic dilation of bronchial tubes with thickend walls, and signs of current endobronchial infection (Figure 1). Currently, the patient relies on ongoing medical care and treatment, including intermittent courses of oral antibiotics, expectorants, oxygen therapy, and non-invasive ventilation.
Figure 1: Coronal chest CT view showing dextrocardia and extensive tubulocystic dilation of bronchial tubes with thickened walls (white arrow), predominantly in both lower lobes and left upper lobe (A). Additionally, centrilobular ground-glass opacities and noticeable tree-in-bud sign (yellow arrow) in both lower lobes and right ligula segment, suggests current endobronchial infection on axial (B) and (C) views.
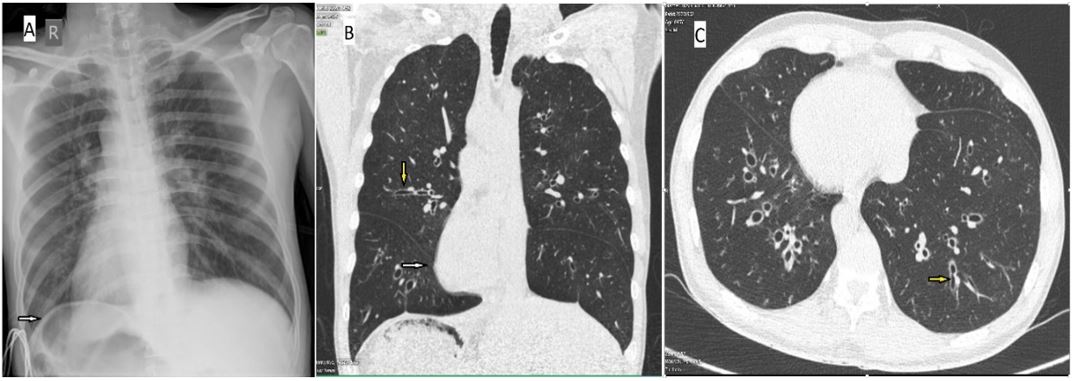
Figure 2: PA chest X-ray showing dextrocardia and stomach bubble under the right diaphragm (A) (white arrow). Chest CT scans showing tubular bronchiectasis (yellow arrow) in upper and lower lobes of both lungs, predominantly in lower lobes in reconstruction coronal (B) and axial (C) views
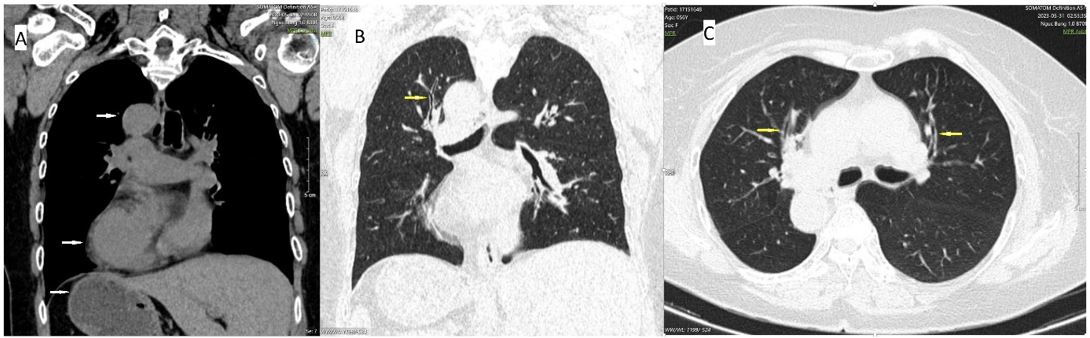
Figure 3: Chest CT image showing situs inversus with cardiac apex, aortic knuckle, stomach fundus on right on coronal view (A) (white arrows). Additionally, coronal (B) and axial (C) views showing subtle tubular bronchiectasis (yellow arrows) in upper lobe of right lung and lower lobes of both lungs.
Case 2: A man was 45-year-old, presenting with symptoms of chronic respiratory inflammation and sinusitis, including recurrent nasal discharge, coughing, and frequent phlegm production since adolescence. The patient was diagnosed with situs inversus at the age of 25. At the age of 40, he started experiencing progressively worsening shortness of breath. Interestingly, the patient had two children, both of whom are perfectly heathy. He was admitted to the hospital due to increased difficulty breathing and interrupted sleep. Upon examination at the time of admission, the patient appeared to be of average physique, with disoriented consciousness and severe shortness of breath. Lung examination revealed decreased breath sounds bilaterally, diffuse wheezing, crackling sounds throughout both lungs. PA chest X-ray and high-resolution computed tomography (HRCT) of the chest showed dextrocardia, and bronchiectasis (Figure 2). Arterial blood gas analysis indicated respiratory failure, with a PaCO2 level of 105 mmHg. Bacterial culture of the sputum showed abundant growth of Pseudomonas aeruginosa which remained sensitive to multiple antibiotics. The treatment plan included antibiotics, expectorants, anti-inflammatory drugs, bronchodilators, and non-invasive ventilation.
Case 3: The patient is a 56-year-old female with a history of chronic sinusitis since childhood, presenting with episodes of nasal discharge that occur during weather changes. In addition, she has been diagnosed and treated for asthma. During this period, the patient underwent regular health check-ups and underwent chest X-ray and CT scan of the chest and abdomen, revealing situs inversus and subtle bronchiectasis in the upper lobe of right lung and bilateral lower lobes of both lungs (Figure 3). Currently, the patient does not exhibit any respiratory symptoms on clinical examination. Respiratory function tests and blood gas analysis are within normal limits. The patient currently has one healthy child.
Discussion
Primary ciliary dyskinesia is an autosomal recessive genetic disorder that can be congenital or acquired, affecting the functioning of cilia lining the respiratory tract and fallopian tubes. The immotility of cilia is due to a deficiency in dynein arms of the cilia. These immotile cilia are also present in other areas with cilia, specifically in the inner ear and sperm ducts. Therefore, patients often exhibit chronic recurrent sinusitis, middle ear infections, deafness, infertility, lung inflammation, and bronchiectasis. Approximately 50% of PCDs patients have situs inversus. When situs inversus is present along with sinusitis and bronchiectasis, it is known as KS [7,8,9].
The normal ciliary function is crucial for protecting the respiratory tract, sperm motility, and proper positioning of organs during embryonic development. Deficiencies or abnormalities in the dynein arms, radial spokes, and microtubules of the cilia, encoded by mutated DNAI1 and DNAH5 genes, have been identified as structural and functional anomalies that lead to impaired ciliary function. Abnormal ciliary motion at different sites leads to recurrent respiratory infections, infertility, and situs inversus [4,5,6].
The recommended diagnostic criteria for this syndrome include a history of bronchial infection and chronic rhinosinusitis since childhood, combined with one or more of the following characteristics: (a) situs inversus or right-sided heart in the patient or siblings, (b) live but immotile sperm, (c) loss or reduced ability of mucociliary clearance in the bronchi, and (d) ciliary ultrastructural defects observed under electron microscopy [10,11,12]. Laboratory screening tests include measuring nitric oxide levels in exhaled breath and conducting a saccharin test to evaluate mucociliary function in the nasal mucosa. High-speed video microscopy is used to assess the frequency and pattern of ciliary motion, while transmission electron microscopy is used to detect structural defects in cilia. Genetic testing to identify mutations in DNAI1 and DNAH5 genes is also conducted in the laboratory for definitive diagnosis. Abnormalities observed include reduced nasal nitric oxide concentration (approximately 10% of normal levels), prolonged saccharin clearance time (>1 hour), decreased ciliary beat frequency (<11 Hz/second), and defects in ciliary ultrastructure (dynein arms) and mutated DNAI1 and DNAH5 genes [5]. In a clinical setting, it is important to differentiate KS from Young syndrome, a rare genetic disorder similar to KS, which typically affects middle-aged males with chronic sinusitis, infertility due to azoospermia, and bronchiectasis. Individuals with this disorder have normal lung function but tend to secrete thick, viscous mucus, increasing the risk of pulmonary infections. The process of sperm production is normal, but reduced fertility is attributed to impaired transport of sperm through the reproductive tract [9,13].
All three of our patients had a history of sinusitis, recurrent respiratory infections since childhood, bronchiectasis, and situs inversus observed in imaging. The two male patients exhibited more severe clinical symptoms and progression. The first patient experienced multiple episodes of severe respiratory infections, which negatively affected his overall health and quality of life. Lung function declined rapidly, leading to early onset respiratory failure, occurring only 8 years after the disease was diagnosed. The patient now depends entirely on medical support and is infertile. The second patient shows a slower progression with fewer respiratory tract infections, and the decline in lung function occurs at a slower rate. After 15 years from the time of diagnosis, the patient presents with chronic respiratory failure with CO2 retention, and their overall condition is better. Particularly, the second patient has normal reproductive function.
In the third patient, lung damage is minimal and there have been almost no respiratory tract infections throughout the course of the disease up to the present time. Besides the symptoms of allergic rhinosinusitis, the patient is entirely healthy and does not exhibit any signs of respiratory tract infection. CT imaging of the lungs also shows very little bronchiectasis. The patient also has normal reproductive function. However, they are also diagnosed with bronchial asthma. Thus, there are clear differences in respiratory symptoms, disease progression, and reproductive function among the three patients. This may be related to the extent of structural damage and functional impairment of the target organs. Moreover, in female patients with KS, the degree of damage to target organs such as the lungs and reproductive system may be milder compared to male patients. On the other hand, the third patient is a female and has not been exposed to cigarette smoke, which differentiates her from the male patients, and cigarette smoke could be a risk factor for the progression of lung damage in KS patients. However, further studies with larger sample sizes are needed in the future to substantiate this hypothesis. Furthermore, the possibility of reproductive capacity in KS patients is rare. This can be explained by the potential heterogeneity through intermediate genetic influences on phenotypic expressions [2].
The standard respiratory treatment for patients with KS includes the use of antibiotics (preferably those with good coverage against Pseudomonas). The effectiveness of DNase and other mucolytic agents such as hypertonic saline and acetylcysteine has not been fully evaluated in these patients, but they can be used, especially in patients with recurrent infections or ongoing respiratory symptoms. Respiratory physical therapy, oxygen therapy, and non-invasive ventilation should be considered in cases of respiratory failure with CO2 retention [12]. Low-dose prolonged prophylactic antibiotics should be administered in individuals who frequently experience acute exacerbations of bronchiectasis (≥ 3 times per year). Routine vaccination against influenza and pneumococcus is highly effective in preventing respiratory infections in these patients [12,14]. It is particularly important to avoid exposure to harmful agents such as cigarette smoke. Despite having a slower progression of respiratory failure compared to case 1 and case 2 experienced respiratory failure at an early stage when compared to patients with chronic obstructive pulmonary disease and respiratory failure [4,15,16,17]. In our two male patients, both of whom had extensive bronchiectasis in both lungs, sputum cultures consistently revealed infection with multidrug-resistant gram-negative bacteria. Thus, gram-negative bacterial infections are commonly observed in KS patients with significant bronchiectasis.
Conclusion
The diagnosis of KS relies on clinical criteria and imaging findings since genetic testing and invasive interventions are challenging to perform. The extent of organ damage and its consequences can vary among individuals. Early and common manifestations include symptoms of sinusitis, followed by recurrent lower respiratory tract infections. Screening should be emphasized in patients with a history of sinusitis and recurrent bronchitis. Infertility in males with KS is a common feature, although a few cases may still retain reproductive function. In some female patients, reproductive function may be less affected. Early diagnosis, avoidance of exposure to harmful agents such as cigarette smoke, respiratory infection prevention, and prompt treatment may potentially slow down the progression of lung damage and improve the quality of life for affected individuals.
Ethics Statement
Written informed consent was obtained from the patient to publish clinical details. Institutional review board approval is not required for deidentified cases reports.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author Contributions
The literature search was performed by CNH. Data collection was done by CNH, LTD. All authors contributed equally to the analysis and interpretation of data of the case report: CNH, CTD, LTD, TTQ, and CNH drafted the manuscript.
Funding:The authors received no financial support for the research authorship and / or publication of this article
Acknowledgments
All the authors would like to thank patients and Military Hospital 175 Staff for their support to publish these cases report.
References
- Mirra V, Werner C, Santamaria F. Primary Ciliary Dyskinesia: An Update on Clinical Aspects, Genetics, Diagnosis, and Future Treatment Strategies. Front Pediatr. 2017.
- Barthwal MS. Kartagener's syndrome in a fertile male - An uncommon variant. Lung India. 2006; 23(3): 123.
- Dixit R, Dixit K, Jindal S, et al. An unusual presentation of immotile-cilia syndrome with azoospermia: Case report and literature review. Lung India Off Organ Indian Chest Soc. 2009; 26(4): 142-145.
- Mishra M, Kumar N, Jaiswal A, et al. Kartagener’s syndrome: A case series. Lung India Off Organ Indian Chest Soc. 2009; 29(4): 366-369.
- Chilvers MA, Rutman A, and O’Callaghan C. Ciliary beat pattern is associated with specific ultrastructural defects in primary ciliary dyskinesia. J Allergy Clin Immunol. 2003; 112(3): 518-524.
- Lobo LJ, Zariwala MA, Noone PG. Ciliary dyskinesia: primary ciliary dyskinesia in adults. Eur Respir Mon. 2011; 52:130–49. .
- Olbrich H, Häffner K, Kispert A, et al. Mutations in DNAH5 cause primary ciliary dyskinesia and randomization of left-right asymmetry. Nat Genet. 2002; 0(2): 143-144.
- Skeik N, Jabr F. Kartagener syndrome. Int J Gen Med. 2011; 4: 41-43.
- Kartagener Syndrome - an overview | ScienceDirect Topics. <https://www.sciencedirect.com/topics/medicine-and-dentistry/kartagener-syndrome>, accessed: 06/23/2023.
- Fraser RS, Muller NL, Colman N, Pare PD. Bronchiectasis and other bronchial abnormalities. In: Fraser RS, Muller NL, Colman N, Pare PD, editors. Diagnosis of diseases of the chest. 4th ed. Philadelphia: W.B. Saunders Company; 1999; 2281-3.
- Wahba M. Kartagener syndrome | Radiology Reference Article | Radiopaedia.org. Radiopaedia, <https://radiopaedia.org/articles/kartagener-syndrome-1>, accessed: 06/23/2023.
- Ibrahim R, Daood H. Kartagener syndrome: A case report. Can J Respir Ther CJRT Rev Can Ther Respir RCTR. 2021; 57: 44–48.
- Mohammed SK, Jan A. Young Syndrome. StatPearls. StatPearls Publishing, Treasure Island (FL). 2023.
- Najafi S, Mohammadpour A, and Eshghizadeh M. Kartagener syndrome: A Case Report. Asian J Pharm Clin Res. 2018; 7-9.
- Jayashankar CA, Somasekar DS, Perugu PK, Reddy KV, Prakash B, Santosh KV. Kartagener’s syndrome: A case report. Sch J Med Case Rep. 2014; 2(1): 7-10.
- Hailu SS, Amerga ED, Gorfu Y, Zewdineh D. Kartagener’s syndrome: A Case Report. Ethiop Med J. 2016; 54(2): 91-4.
- Dave C, Wharton S, Mukherjee R, Faqihi BM, Stockley RA, Turner AM. Development and Relevance of Hypercapnia in COPD. Can Respir J. 2021; 2021: 6623093.