Case report - Volume 3 - Issue 4
Stanford A aortic dissection with involvement of supraaortic vessels associated with bicuspid aortic valve, ascending aortic aneurysm and coarctation of the proximal descending aorta: A case report
Lissandrello Ezequias1*; Guardiani Fernando2; Ahuad Guerrero Rodolfo Andrés3; Cohen Arazi Hernán4*
1Resident, Department of Cardiology, Corporación Médica Clinic, Buenos Aires, Argentina
2Coordinator of the Department of Cardiology, Corporación Medica Clinic, Buenos Aires, Argentina
3Head of the Department of Cardiology, Corporación Médica Clinic, Buenos Aires, Argentina
4Coordinator of the Department of Cardiology, Olivos Clinic, Buenos Aires, Argentina
Received Date : July 17, 2023
Accepted Date : Aug 16, 2023
Published Date: Aug 25, 2023
Copyright: © Lissandrello Ezequias Lionel 2023
*Corresponding Author : Lissandrello Ezequias Lionel, Resident, Department of Cardiology, Corporación Médica Clinic, Buenos Aires, Argentina.
Email: ezequiaslissandrello@gmail.com
DOI: Doi.org/10.55920/2771-019X/1534
Abstract
Background: Of all acute aortic syndromes, more than 85% correspond to aortic dissection, reaching a mortality rate in the first 24 hours up to 50% in its natural evolution. The signs and symptoms are not always present but are very specific. Computed axial tomography is the most widely used imaging study to evaluate acute aortic syndromes due to its speed, availability, and high sensitivity (more than 95%).
Case Description: This paper reports the case of a patient who presented in the emergency service with precordial pain radiating to the jaw and back, diffuse changes in the electrocardiogram and showing in the tomography type A aortic dissection associated with aneurysm of the aorta and coarctation of the proximal descending aorta. In addition, the echocardiogram showed severe early diastolic aortic regurgitation and bicuspid aortic valve. He underwent surgery immediately, achieving hospital discharge after a few weeks.
Conclusion: The early suspect, the diagnosis with early imaging of the heart and aorta and prompt intervention may improve the prognosis in a pathology as serious and with such a high mortality rate as aortic dissection.
Introduction
Aortic dissection is characterized by a tear in the intima and media layer of the aorta, producing a dissection flap that separates the true lumen from the extraluminal channel called the false lumen, with the possibility of anterograde and/or retrograde extension of the lesion and limiting the distal flow.
Determining the exact prevalence of aortic dissection is s challenging due to its high mortality rate, particularly before reaching the hospital. However, in studies involving the general population, it is estimated than there are between 2.6 and 3.5 cases of aortic dissection per 100.000 people per year. This condition occurs more frequently in older men, typically between their fifth and seventh decade of life, who have a history of high blood pressure and atherosclerosis. In younger patients, aortic dissection is often associated with factors such as a bicuspid aortic valve, collagen disorders, smoking and history of cardiac surgery.
Case report
History and presentation
A 30 year-old male patient, with a history of smoking, unstudied arterial hypertension, and dislocated lens of the left eye, consulted in emergency service due to precordial pain lasting one hour, pain intensity 10/10, of sudden onset, radiating to the jaw and back.
Physical examination
As relevant, the patient present tachycardia, diaphoretic, blood pressure of 140/30 mmHg, imperceptible pulses in lower limbs and presence of holodiastolic murmur en myocardium.
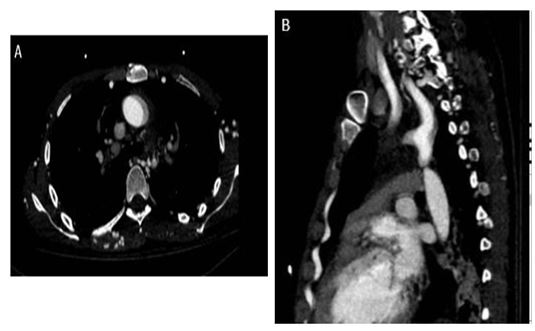
Figure 1: A) In this computed axial tomography, the dissection flap can be seen at the level of the ascending aorta, at the same time that the coarctation point of the proximal descending aorta is seen (blue arrow). B) In another section of the same study, it can also be observe the involvement of the supra-aortic vessels, with the dissection flap ending inside the coarctation.
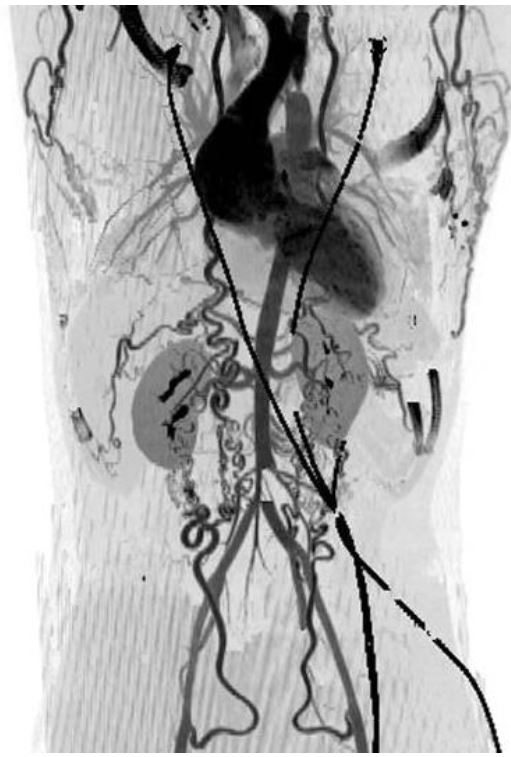
Figure 2: In this 3D reconstruction, it can be objectified the ascending aortic aneurysm, the coarctation of the proximal descending aorta generating the staining difference before and after coarctation, and the evidence of significant collateral circulation and increased permeability at the mammary, mediastinal, dorsal, axillary, abdominal and lumbar levels.
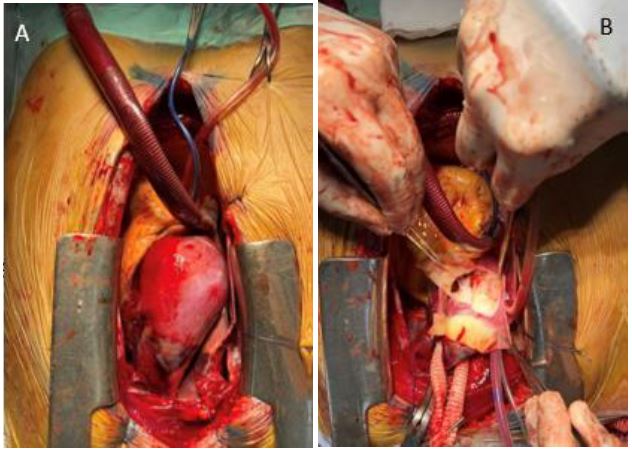
Figure 3: A) When performing the sternotomy, the aneurysmal dilatation of the ascending aorta is evident, observing a hematoma on its wall. B) Continued surgery, the intimal dissection of the same aortic zone was observed.
Investigations
ECG showed diffuse ST. Segment depression with ST segment elevation in AVR. Computed axial tomography was performed evidencing aneurysmal dilatation of the ascending aorta (diameter 62 mm) with the presence of a dissection flap that extended to the proximal descending aorta, compromising the arch, brachiocephalic trunk, right and left carotids up to skull base and right and left subclavians at their birth, flap that ends inside a coarctation in the proximal descending aorta (8 mm diameter). The transthoracic echocardiogram also revealed severe early diastolic aortic regurgitation and bicuspid aortic valve.
Operation Procedure
Emergency surgery was performed, revealing all the findings seen in the images, performing aortic valve replacement with mechanical valve No. 27, replacement of the ascending aorta with a Dacron tube, and preimplantation of the left coronary artery.
Postoperative Course
From de hemodynamic point of view, it evolves with cardiogenic shock and requirements for high doses of inotropes and vasoactive agents, intercurring with reanimated cardiorespiratory arrest. He also experienced massive medical bleeding, without response to the medical treatment established, with reoperation requirements. In the following days, the doses of inotropes were decreased until their closure was achieved and the patient could be extubated, without neurological sequelae but with intense ischemia in both lower limbs, requiring their amputation. Four weeks later, hospital discharge was granted and percutaneous stent implantation was performed as an outpatient treatment for coarctation of the aorta without complication.
Conclusion
Beyond low prevalence of acute aortic syndromes, clinical suspicion and request for adequate complementary studies is important because the prompt and targeted intervention can change the prognosis of a disease with such a high rate of mortality and complications, and for this reason it is important to identify and control cardiovascular risk factors and follow-up on pathologies that may predispose it.
References
- Guevara E, Bagnati, R, Bastianelli G, Baratta S, Battu C, Bluro I, y cols. Consenso de Patología de la Aorta. Rev Argent Cardiol 2023;91 (Suplemento 1): 1-97. http://dx.doi.org/10.7775/rac. es.v91.s1
- Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD; ESC Committee for Practice Guidelines.Eur Heart J. 2014 Nov 1;35(41):2873-926. doi: 10.1093/eurheartj/ehu281. Epub 2014 Aug 29.PMID: 25173340
- Isselbacher EM, Preventza O, Hamilton Black J 3rd, Augoustides JG; 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/ American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Dec 13;146(24):e334-e482. doi:
- Sen I, Erben YM, Franco-Mesa C, DeMartino RR. Epidemiology of aortic dissection. Semin Vasc Surg. 2021 Mar;34(1):10-17. doi: 10.1053/j.semvascsurg.2021.02.003. Epub 2021 Feb 5. PMID: 33757630.