Case report - Volume 3 - Issue 4
A huge solitary duodenal hamartoma; A rare endoscopic finding
Abeer Abdellatef1*; Alhosaeyn Ibrahim Isa2; Mazen Naga1
1Department of Internal Medicine, Hepatogastroenterology Unit, Kasr Al-Ainy School of medicine, Cairo University, Cairo, Egypt.
2Dar Elsalam Cancer Center, SMC, MOH, Egypt.
Received Date : July 30, 2023
Accepted Date : Aug 24, 2023
Published Date: Aug 31, 2023
Copyright: © Abeer Abdellatef 2023
*Corresponding Author : Abeer Abdellatef, Department of Internal Medicine, Hepatogastroenterology Unit, Kasr Al-Ainy School of medicine, Cairo University, Cairo, Egypt.
Email: Abeer.abdellatif86@gmail.com
DOI: Doi.org/10.55920/2771-019X/1537
Abstract
Background: Duodenal polyps are not commonly observed and are typically associated with conditions such as Familial adenomatosis polyposis or Peutz-Jeghers syndrome. However, there are rare instances where duodenal polyps may be encountered as isolated polyps, causing gastrointestinal symptoms.
Case presentation: We present a case of a 41 years old female patient presented with upper GI symptoms, upper endoscopy revealed an accidentally huge duodenal polyp. A hemoclip was applied to the base of the polyp and then removed by polypectomy snare, a small defect was closed successfully with 2 hemoclips. The histopathology revealed a polypoid lesion overlying lobules of Brunner’s gland hyperplasia separated by fibromuscular septa, hamartoma.
Conclusion: Solitary hamartomatous duodenal polyps remain asymptomatic until huge size or complicated. The successful treatment depends on the size and location upon which could be resected either endoscopically or surgically.
Keywords: Duodenal polyp; Solitary huge duodenal hamartoma; Endoscopic resection.
Background
Generally, duodenal polyps are uncommon, they are usually found with Familial adenomatosis polyposis or Peutz-Jegher’s syndrome, but maybe rarely seen as a solitary polyp presenting with gastrointestinal symptoms [1]. Duodenal polyps are usually asymptomatic and symptoms are usually related to size and location and range from dyspepsia, and abdominal pain, to more seriously overt gastrointestinal bleeding, intussusception, and gastric outlet obstruction [2]. CT and MRI are useful for diagnosis, moreover, Endoscopic ultrasonography (EUS) and EGD provide very useful information regarding tumor characteristics [3].
Duodenal subepithelial lesions include lipomas, gastrointestinal stromal tumors, and carcinoids, meanwhile, mucosally-based duodenal lesions include Brunner’s gland tumors, solitary Peutz-Jeghers polyps, and non-ampullary and ampullary adenomas which can require removal and are typically amenable to endoscopic resection [4].
Not unexpectedly that the prevalence of a duodenal polyp on EGD is low, with a reported rate of less than 1% to 5% [5, 6]. Gastrointestinal polyps are a heterogeneous group of lesions that could be divided into hyperplastic, juvenile, inflammatory, adenomatous, and hamartomatous polyps [7]. The duodenal hamartomas are histological malformations composed of abnormal tissue normally found in duodenal mucosa; it could be seen also macroscopically as a circumscribed tumor protruding through the mucosa into the lumen [8]. They may be solitary (solitary PJ polyp or solitary juvenile polyp) or multiple [1]. Endoscopic resection of duodenal lesions is challenging due to a narrow lumen; difficult endoscope position; a thin deep muscle layer that results in a higher rate of perforation; an extensive vascular network supplied by the gastroduodenal artery that increases the risk of bleeding, which can be severe and potentially life-threatening [9-11]. With advanced endoscopic and modern imaging techniques that are now existed, the resection of large mucosally-based duodenal lesions became possible with a low risk of complications [4].Surgical resection is reserved for difficult cases such as giant lesions exceeding 10 cm, multiple lesions, lesions close to the papilla of Vater, or complicated cases such as intussusception or intestinal obstruction [3]. To our knowledge, there are only a few reported cases of solitary duodenal hamartomatous polyps in adults [12].
Case presentation
We present a case of a 41 years old female patient who presented to us with upper GI symptoms in form of gradually progressive postprandial epigastric pain and dyspepsia for a one-year duration. There was no history of any GI bleeding, anorexia, weight loss, mucocutaneous pigmentation of the lips, or fingers suggestive of Peutz-Jegher’s syndrome in the patient or anyone in her family. No past significant medical or surgical illness. Her clinical examination was normal with a normal body mass index (BMI) and a normal laboratory profile. The patient received non-specific treatment in form of proton pump inhibitors and H2 blockers for a one-year duration with no improvement in her symptoms.
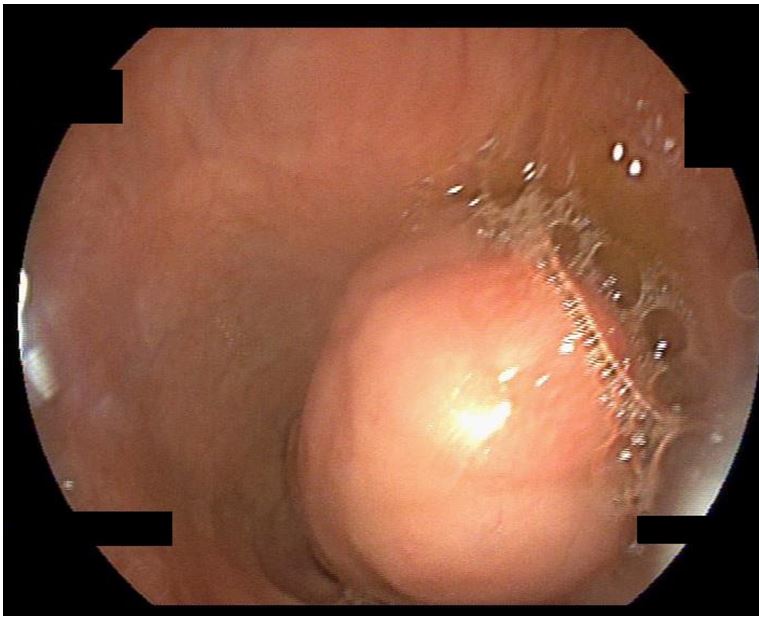
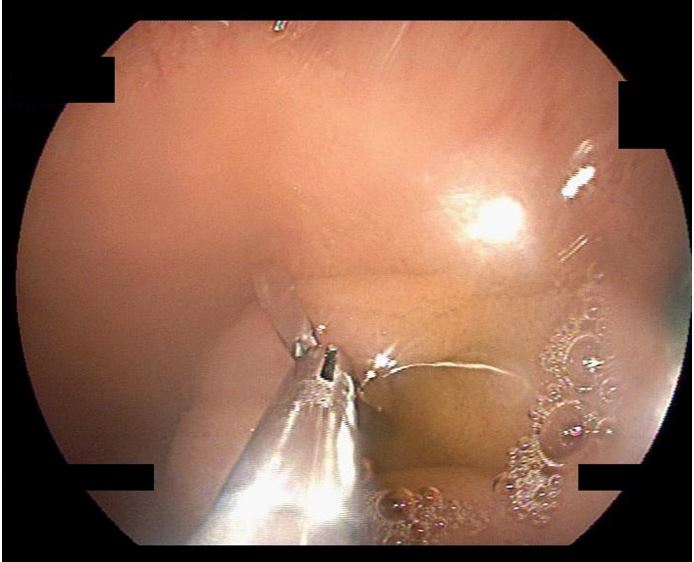
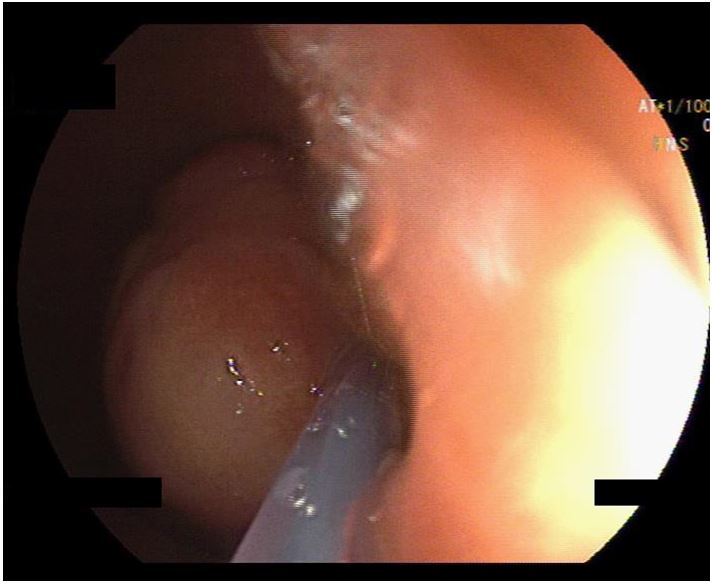
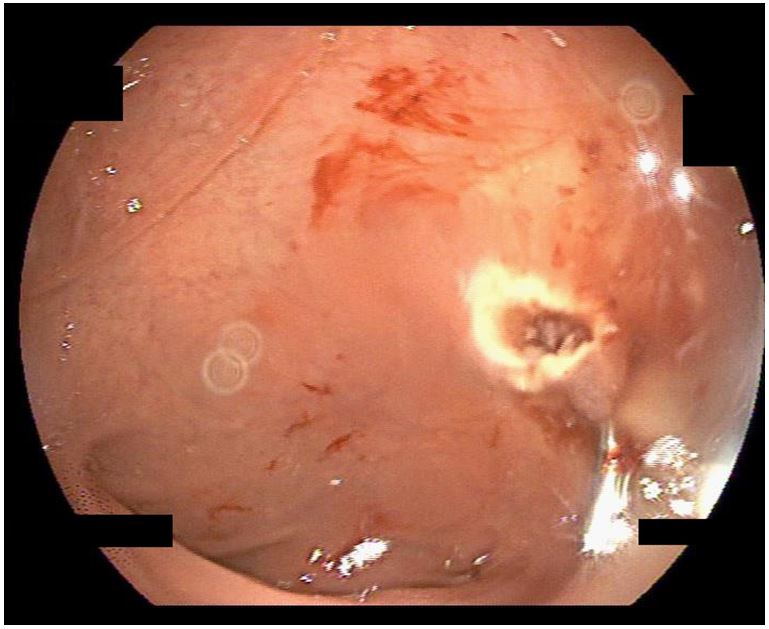
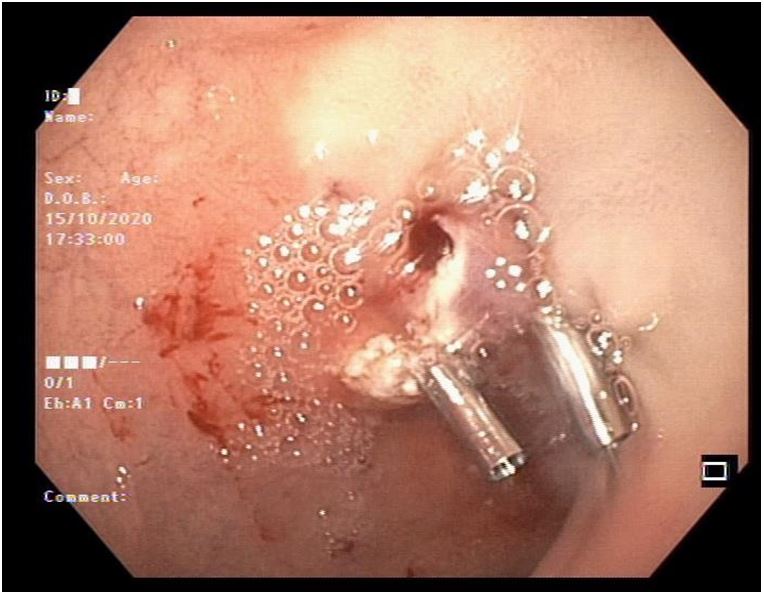
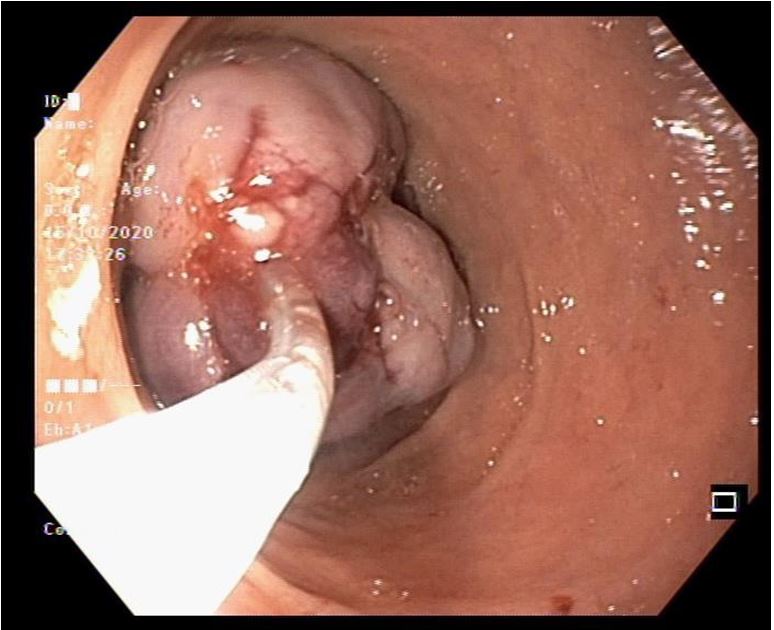
The patient underwent EGD which revealed an accidentally discovered huge polyp (about 4cm in diameter) arising from the posterior duodenal wall with normal overlying mucosa and a positive pillow sign (figure 1). A hemoclip was applied to the base of the polyp (figure 2) and then removed by polypectomy snare (figure 3). After the removal of the polyp, a small defect was seen (figure 4) that was closed successfully with 2 hemoclips (figure 5). Due to the large size of the polyp, it was impossible to extract it (figure 6), therefore, we decided to divide it into two halves and extract each half separately but unfortunately, they passed rapidly and distally and we could not catch it. There were no complications related to the procedure and the patient had immediate relief of symptoms post-procedure.
The patient was informed to monitor her stool and get the polyp and send it for histopathology after defecation. Finally, the histopathology revealed a polypoid lesion covered with focally ulcerated duodenal mucosa overlying lobules of Brunner’s gland hyperplasia separated by fibromuscular septa, hamartoma.
Follow-up endoscopy after one month revealed no residual or recurrent polyps, and the patient remained asymptomatic.
Figure 1: Solitary huge duodenal polyp arising from the posterior wall.
Figure 2: A hemoclip at the base of the polyp.
Figure 3: Resection of the polyp by the snare polypectomy.
Figure 4: A small defect after removal of the polyp.
Figure 5: Successful closure of the defect with 2 hemoclips.
Figure 6: After dividing the polyp, it was impossible to extract it through the pylorus.
Discussion
The duodenal polyps or lesions are uncommonly and accidentally found on EGD that are performed for other reasons with limited case reports present in literature. It could be a subepithelial or mucosally-based lesion. The type of lesion is the cornerstone for the determination of the work-up plan and the possible therapeutic options [5]. A solitary duodenal hamartomatous polyp is very rare, and only a few reports have described its characteristic endoscopic features [12]. Herby, we portray a case of a huge solitary duodenal hamartoma as being a rare and accidental finding in a 41 years old female patient who presented with upper GI symptoms of one-year duration that underwent a successful endoscopic polypectomy.
Being a benign finding; the duodenal polyps are usually asymptomatic and rarely present with complications, those could occur with large polyps (≥4 cm) as dyspepsia, abdominal pain, overt gastrointestinal bleeding, intussusception, and gastric outlet obstruction [2, 13].
Moreover, the rarity of duodenal hamartomatous polyp, it could also occur without an association with a mucocutaneous pigmentation or a family history of Peutz-Jeghers; in this case, it could be diagnosed as a clinical entity different from Peutz-Jeghers syndrome called solitary Peutz-Jeghers type hamartomatous polyp [1, 14].
Gonzalez A, et al. reported a very interesting and unique case report of a hamartomatous duodenal polyp that was associated with intestinal schistosomiasis in a 35-year-old woman who presented with dull abdominal pain [15].
In symptomatic cases, the management is usually not needed and they are observed unless symptomatic, which requires resection. Endoscopic options are available and challenging, surgery is reserved for difficult endoscopic cases or complications [2].
Obvious and critical factors for endoscopic resection of duodenal polyps or lesions include size, location (particularly in relation to major and minor papillae), and whether it is mucosally-based or subepithelial [4]. Snare polypectomy, unroofing, endoloop, submucosal dissection (also called mucosectomy) and endoscopic submucosal dissection (ESD) are the reported and well-established techniques for endoscopic therapy of GI lesions [4].
Success rates for complete endoscopic removal of duodenal adenomas range from about 70% to 100% in the reported literature [16-24].
Kedia et al reported the success rate of endoscopic mucosal resection (EMR) reaching up to 95% for polyps involving < 25% luminal circumference, compared to 46% for polyps involving 25% to 50% of the luminal circumference, and 0% for polyps encompassing > 50% of the luminal circumference [17].
Basford and Bhandari review of several studies reported that 80% of the cases were completed within one session, 17% within two sessions, and 3% in three sessions [16].
The literature review reveals that there have been documented cases of Brunner's gland hyperplasia varying in size from 0.7 to 12 cm, with an average size of 4 cm. However, there are only a few reported cases where the size exceeds 5 cm [25-28]. In our knowledge, it is not more than twenty seven cases of solitary type hamartomatous polyp in the duodenum reported in literatures, considering it is rarity [29].
Conclusion
Solitary hamartomatous duodenal polyps are extremely rare findings of the gastrointestinal tract that could be expressed as an incomplete or initial form of Peutz-Jeghers syndrome (PJ syndrome). Usually, patients remain asymptomatic until huge size or complicated such as gastrointestinal bleeding, intussusceptions, or bowel obstruction. The successful treatment depends on the size and location and could be resected either endoscopically or surgically.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Funding: Authors received no funding for this study
References
- Munghate G, Karkera P, Chavan S, Raj A, Bodhanwala M, Bendre P. Solitary hamartomatous duodenal polyp in an infant. Journal of Pediatric Surgery Case Reports [Internet]. Elsevier BV. 2021; 68: 101831. Available from: http://dx.doi.org/10.1016/j.epsc.2021.101831
- Tjandra D, Knowles B, Simkin P, Kranz S, Metz A. Duodenal Lipoma Causing Intussusception and Gastric Outlet Obstruction. ACG Case Rep J. 2019; 6(11): e00157. Published 2019 Nov 15. doi:10.14309/crj.0000000000000157
- Yoshii H, Izumi H, Tajiri T, Mukai M, Nomura E, Makuuchi H. Surgical Resection for Hemorrhagic Duodenal Lipoma: A Case Report. Tokai J Exp Clin Med. 2020; 45(2): 75-80. Published 2020 Jul 20.
- Gaspar JP, Stelow EB, Wang AY. Approach to the endoscopic resection of duodenal lesions. World J Gastroenterol. 2016;22(2):600-617. doi:10.3748/wjg.v22.i2.600
- Ghazi A, Ferstenberg H, Shinya H. Endoscopic gastroduodenal polypectomy. Ann Surg. 1984; 200: 175-180. [PMID: 6465972 DOI:10.1097/00000658-198408000-00010]
- Jepsen JM, Persson M, Jakobsen NO, Christiansen T, Skoubo-Kristensen E, Funch-Jensen P, et al. Prospective study of prevalence and endoscopic and histopathologic characteristics of duodenal polyps in patients submitted to upper endoscopy. Scand J Gastroenterol 1994; 29: 483-487. [PMID: 8079103 DOI: 10.3109/00365529409092458]
- Patil MV, Rathod U, Deshmukh M, Margam S, Kalgutkar AD. Spectrum of gastrointestinal polyps: a tertiary care hospital experience of five years. Indian J Pathol Oncol. 2018; 5(4): 656-62. https://doi.org/10.18231/2394-6792.2018.0125.
- Acea Nebril B, Taboada Filgueira L, Paraj´o Calvo A, Gayoso García R, G´omez Rodríguez D, S´anchez Gonz´alez F, et al. Solitary hamartomatous duodenal polyp; a different entity: report of a case and review of the literature. Surg Today. 1993; 23(12): 1074-7. 10.1007/BF00309096. PMID: 8118121.
- Honda T, Yamamoto H, Osawa H, Yoshizawa M, Nakano H, Sunada K, et al. Endoscopic submucosal dissection for superficial duodenal neoplasms. Dig Endosc. 2009; 21: 270-274 [PMID: 19961529 DOI: 10.1111/j.1443-1661.2009.00908. x]
- Oka S, Tanaka S, Nagata S, Hiyama T, Ito M, Kitadai Y, et al. Clinicopathologic features and endoscopic resection of early primary nonampullary duodenal carcinoma. J Clin Gastroenterol 2003; 37: 381-386. [PMID: 14564184 DOI: 10.1097/00 004836-200311000-00006]
- Endo M, Abiko Y, Oana S, Kudara N, Chiba T, Suzuki K, et al. Usefulness of endoscopic treatment for duodenal adenoma. Dig Endosc. 2010; 22: 360-365. [PMID: 21175499 DOI: 10.1111/j.1443-1661.2010.01014.x]
- Jamaludin AZ, Telisinghe PU, Yapp SK, Chong VH. Solitary duodenal hamartomatous polyp with malignant transformation: report of a case. Surg Today. 2009; 39(6):5 27-532. doi:10.1007/s00595-008-3873-9
- Gnanapandithan K, Aslanian HR, Jamidar PA, Muniraj T. Endoscopic Resection of a Giant Duodenal Lipoma. ACG Case Rep J. 2020; 7(3): e00327. Published 2020 Mar 17. doi:10.14309/crj.0000000000000327
- Suzuki S, Hirasaki S, Ikeda F, Yumoto E, Yamane H, Matsubara M. Three cases of Solitary Peutz-Jeghers-type hamartomatous polyp in the duodenum. World J Gastroenterol. 2008; 14(6): 944-947. doi:10.3748/wjg.14.944
- Gonzalez A, Gupta K, Rodriguez S, Wadhwa V, Bejarano P, Charles R. Unique Case of a Hamartomatous Duodenal Polyp Associated With Intestinal Schistosomiasis. ACG Case Rep J. 2021; 8(1):e 00485. Published 2021 Jan 29. doi:10.14309/crj.0000000000000485
- Basford PJ, Bhandari P. Endoscopic management of nonampullary duodenal polyps. Therap Adv Gastroenterol. 2012; 5: 127-138. [PMID: 22423261 DOI: 10.1177/1756283X11429590]
- Kedia P, Brensinger C, Ginsberg G. Endoscopic predictors of successful endoluminal eradication in sporadic duodenal adenomas and its acute complications. Gastrointest Endosc. 2010; 72: 1297-1301. [PMID: 20970793 DOI: 10.1016/j.gie.2010.07.039]
- Navaneethan U, Lourdusamy D, Mehta D, Lourdusamy V, Venkatesh PG, Sanaka MR. Endoscopic resection of large sporadic non-ampullary duodenal polyps: efficacy and long-term recurrence. Surg Endosc. 2014; 28: 2616-2622. [PMID: 24695983 DOI: 10.1007/ s00464-014-3512-z]
- Alexander S, Bourke MJ, Williams SJ, Bailey A, Co J. EMR of large, sessile, sporadic nonampullary duodenal adenomas: technical aspects and long-term outcome (with videos). Gastrointest Endosc. 2009; 69: 66-73. [PMID: 18725157 DOI: 10.1016/j.gie.2008.04.061]
- Hirasawa R, Iishi H, Tatsuta M, Ishiguro S. Clinicopathologic features and endoscopic resection of duodenal adenocarcinomas and adenomas with the submucosal saline injection technique. Gastrointest Endosc. 1997; 46: 507-513. [PMID: 9434217]
- Lépilliez V, Chemaly M, Ponchon T, Napoleon B, Saurin JC. Endoscopic resection of sporadic duodenal adenomas: an efficient technique with a substantial risk of delayed bleeding. Endoscopy. 2008; 40: 806-810. [PMID: 18828076 DOI: 10.1055/ s-2008-1077619]
- Abbass R, Rigaux J, Al-Kawas FH. Nonampullary duodenal polyps: characteristics and endoscopic management. Gastrointest Endosc 2010; 71: 754-759 [PMID: 20363416 DOI: 10.1016/j.gie.2009.11.043]
- Kim HK, Chung WC, Lee BI, Cho YS. Efficacy and long-term outcome of endoscopic treatment of sporadic nonampullary duodenal adenoma. Gut Liver. 2010; 4: 373-377. [PMID: 20981216 DOI: 10.5009/gnl.2010.4.3.373]
- Marques J, Baldaque-Silva F, Pereira P, Arnelo U, Yahagi N, Macedo G. Endoscopic mucosal resection and endoscopic submucosal dissection in the treatment of sporadic nonampullary duodenal adenomatous polyps. World J Gastrointest Endosc. 2015; 7: 720-727. [PMID: 26140099 DOI: 10.4253/wjge.v7.i7.720]
- Jung Y, Chung IK, Lee TH, et al. Successful Endoscopic Resection of Large Pedunculated Brunner's Gland Hamartoma Causing Gastrointestinal Bleeding Arising from the Pylorus. Case Rep Gastroenterol. 2013; 7(2): 304-307. Published 2013 Jul 18. doi:10.1159/000354138
- Satoh T, Matsubayashi H, Takizawa K, et al. Giant Brunner's Gland Hyperplasia of the Duodenum Diagnosed by Endoscopic Ultrasonography-guided Fine Needle Biopsy and Treated by Laparoscopic Endoscopic Cooperative Surgery. Intern Med. 2019; 58(14): 2009-2013. doi:10.2169/internalmedicine.2477-18
- Bojanapu S, Mangla V, Mehrotra S, Lalwani S, Mehta N, Nundy S. Brunner's gland hyperplasia: an unusual duodenal submucosal lesion seen in four patients. J Surg Case Rep. 2018; 2018(11): rjy305. Published 2018 Nov 30. doi:10.1093/jscr/rjy305
- Khosla M, Khosravi F, Cashman J, Das A. Giant Brunner's Gland Hamartoma as a Cause of Iron Deficiency Anemia. ACG Case Rep J. 2017; 4: e37. Published 2017 Mar 15. doi:10.14309/crj.2017.37
- Sekino Y, Inamori M, Hirai M, et al. Solitary Peutz-Jeghers type hamartomatous polyps in the duodenum are not always associated with a low risk of cancer: two case reports. J Med Case Rep. 2011; 5: 240. Published 2011 Jun 27. doi:10.1186/1752-1947-5-240