Research Article - Volume 3 - Issue 5
Photoelastic stress in mandibular overdenture retained by three implants
Julia Trevizam Campana; Mauro Antonio de Arruda Nobilo; Rafael Leonardo Xediek Consani*
Department of Prosthodontics and Periodontology, Division of Dental Prosthesis, State University of Campinas, Piracicaba Dental School, Piracicaba, SP, Brazil.
Received Date : July 19, 2023
Accepted Date : Aug 28, 2023
Published Date: Sep 04, 2023
Copyright: © Rafael Leonardo Xediek Consani 2023
*Corresponding Author : Rafael Leonardo Xediek Consani, Piracicaba Dental School, UNICAMP, 901 Limeira Ave. 13414-903 Piracicaba, SP, Brazil.
Email: rconsani@fop.unicamp.br
DOI: Doi.org/10.55920/2771-019X/1539
Abstract
Objectives: This study evaluated the photoelastic stress promoted by different load intensities exerted by the maxillary complete denture on the mandibular overdentures retained by three implants.
Materials and Methods: The median implant was placed in the mandibular stone model midline and the lateral implants 18 mm distant of each side of the median implant. Occlusal load with intensities of 10, 20 or 30 kgf were exerted in the mandibular photoelastic model by the maxillary complete denture in maximum intercuspation. Axial single loads with same intensities were also exerted on the first left or right molar of the overdenture. Qualitative analysis was made using polariscope and quantitative analysis with images obtained by the FRINGES program.
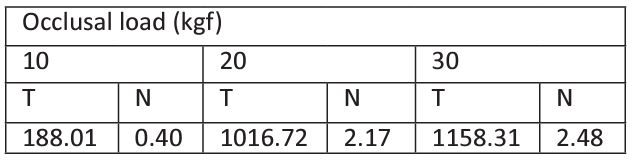
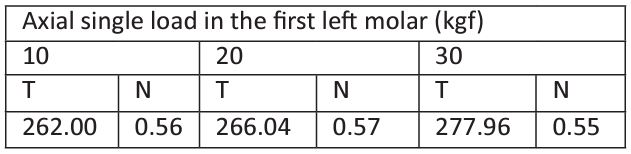
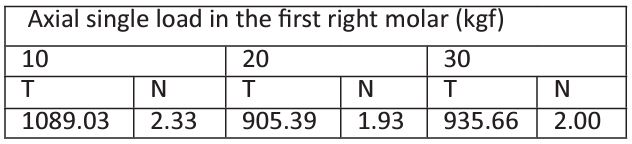
Results: Qualitative analysis: Occlusal force, similar stress in the apex of the median implant and in the posterior region of the lateral implants for all force intensities. Single force, stress in the apexes of the left or right implant and in the posterior region of the mandible that increased with load increase. Quantitative analysis for occlusal load: 10 kgf (T=188.01; N=0.40); 20 kgf (T=1016.72; N=2.17); 30 kgf (T=11585.40; N=2.48). Axial single load in the left molar: 10 kgf (T=262.00; N=0.56); 20 kgf (T= 266.04; N=0.57); 30 kgf (T=277.96; N=0.55). Axial single load in the right molar: 10 kgf (T=1089.03; N=2.33); 20 kgf (T=905.39; N=1.93); 30 kgf (T=935.66; N=2.00).
Conclusion: Different locations and stress levels occurred in the overdentures supported by three implants when submitted to occlusal or axial load on the first left or right molar.
Keywords: Overdenture; Dental implant; Occlusal load; Photoelastic stress
Introduction
Insufficient stability and retention are the main complaints of the conventional complete dentures users. This prosthetic rehabilitation is associated with several problems, such as lack of stability, support and retention. However, when mandibular complete denture is supported by implants an improvement could be seen in the patients' psychological and social well-being. This treatment also requires different types of attachment systems that connect the complete denture to the implant [1].
An option for this clinical problem is the oral rehabilitation with implant-supported prosthesis that promotes better retention, stability and chewing effort. One or several implants may retain the overdenture and the choice of the number of implants is associated to some factors, such as the anatomy of the alveolar arches and oral biomechanical conditions. Economic factors may also significantly affect the implant amount placed in each specific clinical case. However, a previous study showed that is not clear whether the bone loss, complication types and patient’s satisfaction are related to the number of implants needed to retain the overdenture [2].
Two to four implants placed in the anterior region of the mandible are feasible and clinically satisfactory to retain overdenture in prosthetic rehabilitaions . However, there are countless advantages and disadvantages related to load distribution on the implant in each specific treatment. In addition, the amount of the strain on the posterior residual ridge increases when the number of implants was reduced [3].
A three-dimensional finite element analysis showed that single-implant-retained mandibular overdentures do not show damaging strain concentration in the alveolar bone around the single implant and may be a cost-effective treatment option for edentulous patients. A third implant can be placed between the original two when patients rehabilitated by two-implant overdentures report obvious and constant denture rotation around the fulcrum line [4].
Deformities in the peri-implant region, microfractures and bone resorption are caused by stress exceeding the physiological limit of the alveolar bone. The bone density and the bone-to-implant mineralized interface are higher around of the lateral loaded implant when compared to the inactivated side. Therefore, it is possible that static load applied to implant in the lateral direction promotes a structural adaptation of the peri-implant bone [5].
In mechanical therms, the implant number probably establisches different relations when placed in different regions of the alveolar arch. In addition, previous study showed that the prosthetic design is dependent on the number and location of the implants. On the other hand, the implants number that can be placed will also determine the choice of prosthesis type, since the treatment planning is also related to individual anatomic-morphologic conditions of the maxilla and mandible [6].
Retention of complete mandibular denture can be successfully achieved by means of an implant-retained or natural tooth-retained bar and clip systems in the anterior segment of the mandible. The same design principles are true for both methods of anchoring the retentive bar. These retentive elements must allow some freedom of movement around a fulcrum line designed to be perpendicular to the sagittal plane [7].
Masticatory forces are transmitted directly to framework and osseointegrated implant and consequently to the surrounding alveolar bone, and damage may occur due to stress concentrated in the peri-implant region causing undesirable bone loss. By other hand, indirect comparison provided no evidence to support the assertion that there are differences in marginal peri-implant bone loss between single implant prostheses and multiple screw-retained prostheses [8].
The amount of bone loss in the maxillary anterior region compared to the mandibular posterior region was significantly more. This could possibly be due to the greater vertical cantilever and offset loads in the anterior compared to the posterior region. However, the presence of pocket in the mandibular posterior distal and maxillary anterior palatal regions would be related to deficient oral hygiene [9].
Figure 1: Mandibular photoelastic model with three implants.
Photoelastic analysis allows observing the stress distribution on the model providing a visual display obtained by the polariscope. The method reveals two types of fringes (stress): Colored patterns (clear) denominated isochromatic fringes representing the stress intensity; and dark lines called isoclinic, which overlap the colored fringes and are associated with stress direction. In dentistry, the location and intensity of stress are the major data required for this analysis that may be measured and/or photographed [10].
The aim of this study was to evaluate the photoelastic stress promoted by loads with different intensities applied by maxillary complete denture on mandibular overdenture retained by three implants. The study hypothesis was that different loads would promote different stresses in the mandibular overdentures retained by three implants.
Materials and Methods
Materials and methods used in the current investigation were based in previous study [11]. Complete maxillary denture and mandibular overdentures were made traditionally with thermo-activated acrylic resin (QC-20; Dentsply, Petropolis, RJ, Brazil). Acrylic resin record bases (Vipi Flash; Vipi, Pirassununga, SP, Brazil) and wax occlusion rims (Kota, Sao Paulo, SP, Brazil) were used to relate the maxillary and mandibular stone models in semi-adjustable articulator (A7 Plus; Bioart, Sao Carlos, SP, Brazil).
Arrangements of the artificial teeth (Vivadent PE and Orthosit PE; Ivoclar Vivadent, Barueri, SP, Brazil) were made on the maxillary and mandibular occlusion wax rims. Both hexagon external implants and O’ring analogs (Conexao Prosthesis System; Aruja, SP, Brazil) were placed in the mandibular stone model, and the analogs were screwed in the impression copy using a resin tray fabricated with an access opening for the impression screws. The stone model with the components was replicated with impression material (Silibor; Classico Dental Products, Sao Paulo, SP, Brazil). After 24h, the impression copy was released from the fixation screws, the implants placed on the silicone mold (Median implant in the mandibular model midline and the lateral implants at a distance of 18 mm of each side), which was used to make the photoelastic model (Araldite; Huntsman, Sao Paulo, SP, Brazil).
The photoelastic model (Figure 1) was submitted to axial occlusal load (10, 20 or 30 kgf) exerted by the maxillary denture in maximum intercuspation with the mandibular overdenture [11,12]. The stress was evaluated in front, and left and right sides of the photoelastic model. Axial single loads were also individually exerted on the first right or left molar to verify the alveolar ridge effect in the photoelastic stress, since laterality movements are different in each ridge and influenced by the patient's normal or parafunctional habits.
A circular polariscope (PTH-A-01 model; Federal University of Uberlandia, MG, Brazil) was used for stress analysis and images were taken with digital camera (Canon EOS XSI; New York, NY, USA). The color pattern versus fringe order analysis was made according to the schematic demonstration of the isochromatic fringe order for maximum shear stress using the Fringes program (MatLab environment, Federal University of Uberlandia).
The most relevant positions for each load were analyzed in the points R1 to R11 selected along the mandible model. Three positions were considered for the occlusal load (P1, P3 and P5), two for the right molar (P1 and P3) and two for left molar (P3 and P5). The regions evaluated in each position were standardized so as not to change the location between one image and another. In this way, it was possible to choose standard points for analysis of the maximum shear stress (T) based in the comparison among fringe orders.
The images of the photoelastic model and the optical constant (Kσ=0.468 kgf/mm) of the photoelastic resin were inserted in the FRINGES program. Based on the equations inserted and the fringe orders informed by the examiners, the FRINGES program provided the maximum shear stress (T) of each predetermined point. The load was applied so that fringe orders in each position did not exceed the order 4. After loading, the image was analyzed and the values of the fringe orders and shear stress obtained for each point. Following, the mean values for each position and load intensity were calculated.
The following conditions were considered in the study: 1) Single photoelastic model for each group [13,14], and 2) Adobe Photoshop 7.0 software for photoelastic image analysis. The method allowed verifying the structure passivity after implant placement and when the force was applied [15,16]. Resultant fringe orders (N) and the direction of stress propagation were photographed, quantitatively evaluated and recorded. Two examiners recorded the results. When there was no agreement between the two examiners in relation to the data, a third examiner evaluated the results to solve the doubts.
Results
Qualitative analysis
Occlusal load
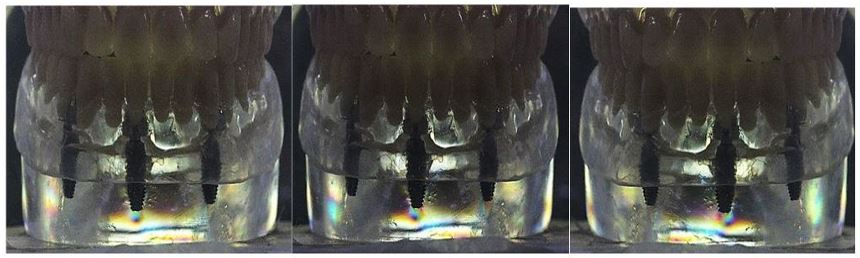
Figure 2 shows the anterior view of the photoelastic model with three implants submitted to occlusal load. Similar stress occurred in the apex of the median implant and in the anterior region of the model for the three load intensities.
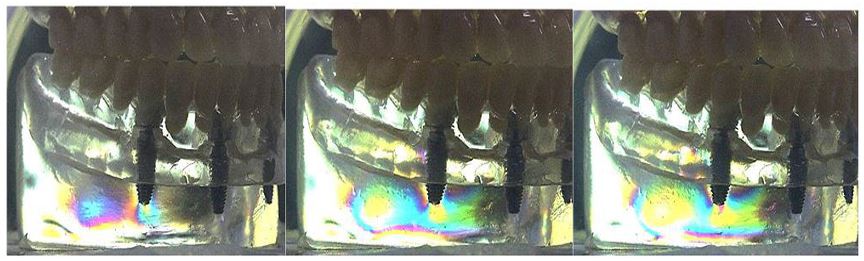
Figure 3 shows the left side view of the photoelastic model with three implants submitted to occlusal load. Stress occurred in the apex of the left implant and in the posterior region of the mo
Figure 4 shows the right side view of the photoelastic model with three implants submitted to occlusal load. Stress occurred in the apex of the right implant and in the posterior region of the model that increased with the load increase.
Load in the left molar
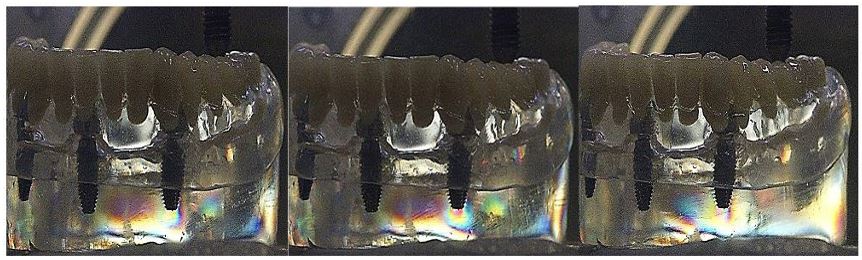
Figure 5 shows the photoelastic model with three implants submitted to axial single load in the left molar. Stress occurred in the apex of the left implant and in the posterior region of the model with the three loads that increased with the load increase.
Load in the right molar
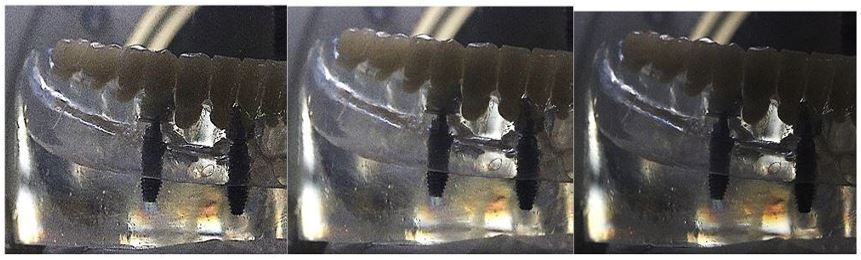
Figure 6 shows the photoelastic model with three implants submitted to axial single load in the right molar. Stress between the median and right implants, and the posterior region of the model did not show stress. Quantitative analysis
Table 1 shows the means of the shear stress (T) and fringe
Figure 2: Anterior view of the photoelastic model with three implants submitted to occlusal load (10, 20 and 30 kgf, respectively).
Figure 3: Left side view of the photoelastic model with three implants submitted to occlusal load (10, 20 and 30 kgf, respectively).
Figure 4: Right side view of the photoelastic model with three implants submitted to occlusal load (10, 20 and 30 kgf, respectively).
Figure 5: Left side of the photoelastic model with three implants submitted to axial single load in the left molar (10, 20 and 30 kgf, respectively).
Figure 6: Right side of the photoelastic model with three implants submitted to axial single load in the right molar (10, 20 and 30 kgf, respectively).
Table 1: Means of shear stress (T) and fringe order (N) for overdenture retained by three implants submitted to occlusal load.
Table 2: Means of shear stress (T) and fringe order (N) for overdenture retained by three implants submitted to axial single load in the first left molar.
Table 3: Means of shear stress (T) and fringe order (N) for overdenture retained by three implants submitted to axial single load in the first right molar.
order (N) for overdenture retained by three implants submitted to occlusal load. The shear stress (T) and fringe order (N) increased with the load increase.
Table 2 shows the means for shear stress (T) and fringe order (N) for overdenture retained by three implants submitted to axial single load in the first left molar. Similar shear stress (T) and fringe order (N) values occurred for the three load intensities.
Table 3 shows the means for shear stress (T) and fringe order (N) for overdenture retained by three implants submitted to axial single load in the first right molar. Similar shear stress (T) and fringe order (N) values occurred with the three load intensities.
Discussion
Photoelastic analysis was used in the current study to evaluate the stress occurred in the mandibular overdenture retained by three implants submitted to load exerted by the maxillary denture or axial single force in the first molars. The different loads and force intensities caused different stresses in the mandibular overdenture retained by three implants; therefore, the study hypothesis was accepted.
The biomechanical behavior of implant-supported prostheses during the occlusal loading was verified in studies using the photoelastic model method. Some of these studies investigated the following variables: Screw-and cement-retained implant prostheses [13], stress in oral obturator prosthesis [14], stress of bar-clip and short coping overdenture attachments [15], number of supporting implants [16], different prosthetic connections [17] and different attachment systems and soft relining [18].
The current study showed that different occlusal loads with different intensities caused different stresses in the alveolar ridge region of the photoelastic mandibular models similarly manufactured. For occlusal load, similar stress occurred in the apex of the median implant and in the anterior region of the mandibular model for the three load intensities (Figure 2). Stress occurred in the apex of the lateral implants and in the posterior region of the mandibular model with the three loads, and increased with the load increase in both sides of the photoelastic model (Figure 3 and 4). For single load in the molar, stress in the apex of the left implant and in the posterior region of the mandibular model with the three loads, and increased with the load increase (Figure 5). Stress occurred between the median and right implants, and the posterior region of the mandibular model did not show stress concentration (Figure 6).
Stress around and in the apex indicates that the implant acts as a stress concentrator. In addition, the concentrated stress intensity would depend of the location and slope of the applied force. The oblique loading increased the number of photoelastic fringes in all models; however, the internal hexagon implant exhibited better biomechanical behavior for the 3-unit implant-supported fixed partial prosthesis [17].
A previous study showed that different loading locations promoted significant differences among the overdenture attachment systems. In general, the moment and force on the implant were greater when the load was directly applied over the implant or between implants in the mid-anterior region [19]. On the other hand, attachment systems promoted different stress distribution, showing greater stress concentration surrounding the implants and homogenous distribution in the photoelastic model without implants [18].
These aforementioned reports seem to corroborate the findings of the current study in relation to the force intensity and consequent different stress concentration in the overdenture supported by three implants. Similar stress concentration occurred in the mandibular overdenture with the three occlusal loads. In this case, the occlusal force exerted by the maxillary denture in maximum intercuspation with the mandibular overdenture was not able to increase the stress concentration level with load increase.
Different load types and force intensities promoted different stress concentrations in the alveolar ridge of the photoelastic models. The shear stress (T) and fringe order (N) increased with the occlusal load intensity (Table 1). Similar shear stress (T) and fringe order (N) values occurred with single load in the left or right molar for the three loads (Tables 2 and 3).
A photoelastic study showed that the number of implants had no significant effect in the stress value around the implants when the axial force was exerted in the central fossa of the first right molar [16]. This result seems to indicate that the stress resulting of the axial force on the first molar would have greater difficulty reaching regions farther from the implant, regardless the implant number. In mechanical terms, this condition would be more damaging to the long-term survival of the implant and consequent alveolar bone loss when compared to the forces distributed homogeneously with greater extension in alveolar bone. The 3-D in vivo force measurements in mandibular implant supported overdentures showed that chewing and grinding resulted in lower vertical forces compared to maximum biting [20].
Besides, there is no evidence to support the assertion that differences exist in the marginal peri-implant bone loss between single implant prostheses and multiple screw-retained prostheses [8]. By other hand, it cannot be affirm that the stress occurred in the overdenture of the current study would not result in some damage to the osseointegration process over the long term. In addition, axial single load applied to the first right or left molar caused different stress levels in each posterior side of the photoelastic model (Figure 5 and 6). The cause of this undesirable result would be verified in studies using finite element analysis to clarify the different stresses between the left and right sides of the photoelastic model.
A previous report showed that stresses were observed on the loaded side of the photoelastic model, and the lowest photoelastic stress was found with the Locator and bar attachments that transmitted little or no discernible stress around the implants [21]. Moreover, overdenture retained by implants provide stronger bite force causing hydrostatic stress within the mucosa and bone resorption of the residual ridge [22]. It was also claimed that the hydrostatic pressure in the mucosa signifies a critical indicator and correlated with clinically measured bone resorption, pointing to severe posterior mandibular ridge resorption in implant-retained overdenture [23].
On the other hand, an increment in implant number tends to cause lower stresses and seems to be a safe and sufficient solution for the treatment of mandibular edentulism with overdenture [24]. In addition, a finite element study showed that the cortical and cancellous bone regions are the least stressed, while ball attachment produced higher stress [25].
The number and the implant position submitted to diferente biting forces influence the movement of the mandibular implant-supported overdenture; however, overdentures retained with three or more implants showed minimal movement [26], and the stress in mandibular overdenture under various loading and dislodging conditions showed that three implants promoted the highest lateral resistance force [27]. Rotational movement of mandibular overdentures is also influenced by the implant numbers, anchoring location and mastication region. During chewing with anterior teeth, the use of 2 implants increased the denture base rotation compared to 1 or 3 implants, and the horizontal movement was small compared to the vertical. However, denture movement under the occlusal force in the molar region was smaller than that in the anterior region [28]. This earlier study showing that the occlusal force in the molar region was smaller compared to anterior region seems did not corroborate with the photoelastic images obtained in the current study with higher stress concentration in the lateral of the models (Figure 3 and 4) compared to anterior region (Figure 2).
Additionally, the existence of a possible inequality between the two sides of the photoelastic model would be considered as a study limitation. Therefore, it would be timely that further studies verified the correlation between the variables of the current investigation and the biomechanical failures in overdenture retained by three implants.
Conclusion
The following conclusion are considered: Different load intensities promoted different stress levels in overdenture retained by three implants submitted to the occlusal load or single axial on the first left or right molar.
Acknowledgements: Coordination for the Improvement of Higher Education Personnel (CAPES) for the assistance to Master Program at Piracicaba Dental School, State University of Campinas, SP, Brazil.
Conflict of interest: The authors declare that there is no conflict of interest known.
References
- Warreth A, Alkadhimi AF, Sultan A, Byrne C, Woods E. Mandibular implantsupported overdentures: Attachment systems, and number and locations of implants - Part I. J Irish Dental Assoc. 2015; 61: 93-7.
- Roccuzzo M, Bonino F, Gaudioso L, Zwahlen M, Meijer HJA. What is the optimal number of implants for removable reconstructions? A systematic review on implant supported overdentures. Clin Ora Implant Res. 2012; 23: 229-37.
- Abe M, Yang TC, Maeda Y, Ando T, Wada M. Support ratio between abutment and soft tissue under overdentures: A comparison between use of two and four abutments. Int J Prosthodont. 2017; 30: 242-4.
- Liu J, Pan S, Dong J, Mo Z, Yubo Fan Y, Feng H. Influence of implant number on the biomechanical behaviour of mandibular implant-retained/supported overdentures: A three-dimensional finite element analysis. J Dent. 2013; 41: 241-9.
- Gotfredsen K, Berglundh T, Lindhe J. Bone reactions adjacent to titanium implants subjected to static load. A study in the dog (I). Clin Oral Implants Res. 2001; 12: 1-8.
- Mericske-Stern RD, Taylor TD, Belser U. Management of the edentulous patient. Clin Oral Implants Res. 2000; 11: 108-125.
- Bem-Ur Z, Gorfil C, Shifman A. Anterior implant-supported overdentures. Quintessence Int. 1996; 27: 603-6.
- Firme CT, Vettore MV, Melo M, Vidigal GM, Jr. Peri-implant bone loss around single and multiple prostheses: Systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014; 29: 79-87.
- Arora V, Rao J, Singh SV, Mishra N, Singh K, et al. An in vivo 24-month study to compare crestal bone loss and pocket depth of platform-switched implants placed in maxillary anterior and mandibular posterior regions. J Prosthodont. 2015; 25: 371-4.
- Machado AC, Cardoso L, Brandt WC, Henriques GE, de Arruda Nóbilo MA. Photoelastic analysis of the distribution of stress in different systems of overdentures in osseous-integrated implants. J Craniofac Surg. 2011; 2: 2332-6.
- Pereira IP, Consani RL, Mesquita MF, Nóbilo MA. Photoelastic analysis of stresses transmitted by complete dentures lined with hard or soft liners. Mater Sci Eng C Mater Biol Appl. 2015; 1: 181-6.
- Campana JT, Mesquita MF, Barão VA, Nobilo MA, Peifer CS, et al. Effect of different force magnitudes on the photoelastic stress in overdenture retained by single implant. Indian J Dental Sci. 2019; 11: 143-9.
- Lee JI, Lee Y, Kim NY, Kim YL, Cho HW. A photoelastic stress analysis of screw and cement-retained implant prostheses with marginal gaps. Clin Implant Dent Relat Res. 2013; 15: 735-49.
- Pesqueira AA, Goiato MC, Santos DM, Haddad MF, Andreotti AM, Moreno A. Stress analysis in oral obturator prosthesis: Part II photoelastic imaging. J Biomed Opt. 2014; 066012.
- Dwivedi A, Vyas R, Gupta A. Quantitative evaluation and comparison of stress transmission characteristics of bar-clip and short coping overdenture attachments under dynamic loading: A photoelastic stress analysis. J Contemp Dent Pract. 2013; 14: 287-92.
- Celik G, Uludag B. Effect of the number of supporting implants on mandibular photoelastic models with different implant-retained overdenture designs. J Prosthodont. 2014; 23: 374-80.
- Tonella BP, Pellizzer EP, Falcon-Antenucci RM, Ferraço R, Faria-Almeida DA. Photoelastic analysis of biomechanical behavior of single and multiple fixed partial prostheses with different prosthetic connections. J Craniofac Surg. 2011; 22: 2060-3.
- Prado Ribeiro P, Goiato MC, Pellizzer EP, Pesqueira AA, Haddad MF, et al. Photoelastic analysis of implant-retained and conventional obturator prostheses with different attachment systems and soft relining. J Craniofac Surg. 2011; 22: 797-800.
- Porter JA, Petropoulos VC, Brunski JB. Comparison of load distribution for implant overdenture attachments. Int J Oral Maxillofac Implants. 2002; 17: 651-62.
- Mericske-Stern R, Piotti M, Sirtes G. 3-D in vivo force measurements on mandibular implants supporting overdentures. A comparative study. Clin Oral Implants Res.1996; 7: 387-96.
- Tokar E, Uludag B, Karacaer O. Load transfer characteristics of three-implantretained overdentures with different interimplant distances. Int J Oral Maxillofac Implants. 2017; 32: 363-31.
- Ahmad R, Chen J, Abu-Hassan MI, Li Q, Swain MV. Investigation of mucosa induced residual ridge resorption under implant-retained overdentures and complete dentures in the mandible. Int J Oral Maxillofac Implants. 2015; 30: 657-66.
- Chen J, Ahmad R, Suenaga H, Li W, Swain M, Li Q. A comparative study on complete and implant retained denture treatments: A biomechanics perspective. J Biomech. 2015; 48: 512-9.
- Arat Bilhan S, Baykasoglu C, Bilhan H, Kutay O, Mugan A. Effect of attachment types and number of implants supporting mandibular overdentures on stress distribution: A computed tomography-based 3D finite element analysis. J Biomech. 2015; 48: 130-7.
- El-Anwar MI, El-Taftazany EA, Hamed HA, ElHay MAA. Influence of number of implants and attachment type on stress distribution in mandibular implant-retained overdentures: Finite element analysis. Open Access Maced J Med Sci. 2017; 5: 244-9.
- Zhang X, Liu W, Qing H, Pei X, Chen J, Wang J. Effect of implant number on the movement of mandibular implant-supported overdentures under biting force: An in vitro study. Quintessence Int. 2018; 49: 709-717.
- Yalikun K, Kanazawa M, Tanoue M, Minakuchi S. In vitro variation measurement of mandibular denture displacement resistance involving 1 to 3 implants. J Prosthet Dent. 2019; 121: 492-7.
- Oda K, Kanazawa M, Takeshita S, Minakuchi S. Influence of implant number on the movement of mandibular implant overdentures. J Prosthet Dent. 2017; 117: 380-5.