Case Report - Volume 3 - Issue 5
Otitis media can also complicate neurosurgically
Patricia Alejandra Garrido Ruiz1*; Marta Román Garrido2*
1Neurosurgery Department, Hospital Universitario de Salamanca, Spain.
2Primary Care Department, Hospital Universitario de Salamanca, Spain.
*These authors have equally contributed to this work and both should be considered as first author.
Received Date : July 20, 2023
Accepted Date : Sep 01, 2023
Published Date: Sep 08, 2023
Copyright: © Marta Román Garrido 2023
*Corresponding Author: Marta Román Garrido, Primary Care Department, Hospital Universitario de Salamanca, Spain.
Email: agrjandri_92@hotmail.com
DOI: Doi.org/10.55920/2771-019X/1543
Abstract
A 59-year-old woman came to the clinic for moderate left earache and low-grade fever of two days’ duration. Personal history of hypercholesterolemia, arterial hypertension and depression. Closed tympanoplasty in the left ear in childhood due to chronic otitis media. Smoker of 25 cigarettes/day and habitual drinker.
Keywords: Otitis; Cholesteatoma; Abscess; Brain; Otologic infection; Computed tomography.
Introduction
Physical examination: afebrile, conscious and oriented. Left otoscopy: minimal whitish-yellowish discharge, crust with tympanic retraction is observed. Right otoscopy without alterations. The rest of the physical examination was unremarkable. Given the clinical findings and the patient's comorbidities, we started antibiotic treatment with amoxicillin-clavulanic acid and she was called to assess again in 48 hours, after which she presented with feverish spikes of up to 40ºC and abundant otorrhea. To conscious exploration, disoriented in time and space. Otoscopy disabled by pain. On neurological examination, she presented predominantly motor aphasia and right homonymous hemianopsia. Given these new clinical data and torpid evolution, we were referred to the hospital emergency room where urgent analysis and cranial CT were performed, describing findings compatible with intracranial extension of the otic process, presenting an area of cerebritis in the left temporal region. Chronic otitis media is an inflammatory process in the middle-ear space that results in long-term, or more often, permanent changes in the tympanic membrane including atelectasis, perforation, tympanosclerosis, retraction pocket development, or cholesteatoma [1,2]. Long-term Eustachian tube dysfunction with a poorly aerated middle-ear space, multiple bouts of acute otitis media, persistent middleear infection, or other chronic inflammatory stimuli are some of the etiological factors of otitis media. The microbiological picture shows the involvement of organisms such as Pseudomonas aeruginosa, very rare in acute otitis media. Once the infection spreads beyond the confines of the lining mucoperiosteum of the middle-ear cleft, it opens door to various complications among which a brain abscess is being dealt with in this report [3,4]. Most of the authors have delineated the location of otogenic brain abscesses in the cerebrum (temporal lobe) than in the cerebellum; however, it's an interesting observation that majority of cerebellar abscesses are associated with middle ear infections [5-8]. Nevertheless, Murthy and Dubey found the occurrence of otogenic abscesses frequently in the cerebellum. Despite diagnostic and therapeutic achievements, mortality from otogenic brain abscesses is still relatively high and usually requires combined neurosurgical and otolaryngological surgery.

Figure 1: Axial brain CT revealed a left temporal area of cerebritis.
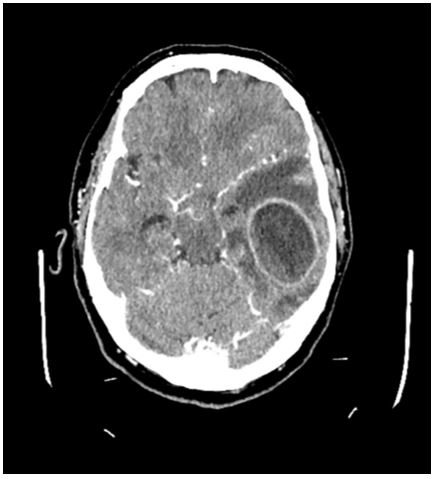
Figure 2: Axial brain CT with contrast after 9 days revealed a left temporal abscess.
Material and methods
We present the case of a 59-year-old patient with cerebritis secondary to middle ear infection. During his hospital admission, she required intervention by the Otorhinolaryngologist for open tympanoplasty due to findings suggestive of chronic cholesteatomatous otitis media. Despite antibiotic therapy, she presented with neurological deterioration after 9 days. A new urgent brain CT revealed an encapsulated abscess, requiring neurosurgical intervention for drainage. Differential diagnosis of brain abscess must always include meningitis and encephalitis. Final diagnosis was cerebral abscess secondary to exacerbated chronic cholesteatomatous otitis media. Subsequently, she continued antibiotic treatment presenting good clinical-radiological evolution.
Conclusions and Discussion
Chronic cholesteatomatous otitis media affects 0.5% of people over 15 years of age, its complication being a rare condition nowadays. Intracranial complications are threatening diseases that have a high rate of morbidity and mortality and we must take them into account in patients with ear infections and a torpid evolution [5,6]. Although rare, otogenic brain abscess may occur as a complication of acute and chronic suppurative otitis media. Otolaryngologists should have a high index of suspicion for otogenic abscesses in patients with a history of chronic ear disease and new symptoms of fever, headache, and nausea. Where warranted, prompt imaging may aid in more rapid diagnosis and treatment of otogenic brain abscess. Conflict of Interest: The authors declare no conflicts of interest.
References
- AL Rhoton. Rhoton’s Cranial Anatomy and Surgical Approaches. Oxford University Press. Congress of Neurological Surgeons (CNS). 2019.
- M Greenberg. Handbook of Neurosurgery, Thieme. 9th Edition. 2019.
- JM González Darder. Abordajes Neuroquirurgicos de la Patología Craneal y Cerebral. Elsevier España. 2015.
- Youmans. Neurological Surgery. 7th Edition. October 11, 2016. Saunders Company.
- Campos-Navarro LA, Barrón-Soto M, Fajardo G. Otitis media aguda y crónica, una enfermedad frecuente y evitable. Rev Facultad Med UNAM. 2014; 57.
- Diego Navarro A, Jorge H, et al. Colesteatoma de oído con complicación intracraneana en contexto de pandemia COVID-19: Reporte de caso clínico y revisión de literatura. Rev Otorrinolaringol. Cir. Cabeza Cuello. 2021; 81: 40-45.
- Sennaroglu L, Sozeri B: Otogenic brain abscess: review of 41 cases. Otolaryngol Head Neck Surg. 2000, 123:751-5.
- Smith JA, Danner CJ. Complications of chronic otitis media and cholesteatoma. Otolaryngol Clin North Am. 2006; 39: 1237-55.

