Research Article - Volume 3 - Issue 5
Role of Superoxide Dis-Mutase in Sera of Iraqi Lung Cancer Patients
Zubaida Haitham Salman*; Firas Hassan
Al-Nahrain University, College of Science, Dept. of chemistry, Jadriya, Baghdad, Iraq.
Received Date : July 20, 2023
Accepted Date : Sep 04, 2023
Published Date: Sep 11, 2023
Copyright: © Zubaida haitham salman 2023
*Corresponding Author: Zubaida haitham salman, Al-Nahrain University, College of Science, Dept. of chemistry, Jadriya, Baghdad, Iraq.
Email: salmanzt54@gmail.com
DOI: Doi.org/10.55920/2771-019X/1544
Abstract
Background: Lung cancer is characterized by uncontrolled cell growth in the lungs, with the potential to spread and affect other tissues and organs if untreated. Adenocarcinomas are the most prevalent subtype of Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC). The prevalence of squamous-cell carcinoma has declined due to reduced smoking rates and changes in cigarette compositions. Cigarette smoking, radon gas exposure, asbestos exposure, exposure to specific chemicals or minerals, diesel exhaust, and air pollution are all potential causes of lung cancer.
Methods: One hundred individuals were divided into two groups. Group 1 had sixty individuals with lung cancer (thirty nonsmokers and thirty smokers), while Group 2 had forty individuals (twenty smokers and twenty nonsmokers). The study evaluated antioxidant enzymatic activities in relation to smoking status.
Results: our research shows lower vitamin levels (E, C, D3) among both smokers and non-smokers with lung cancer compared to healthy individuals. Similarly, individuals with lung cancer tend to have lower levels of the superoxide dismutase enzyme compared to healthy individuals.
Conclusion: our study found that individuals with lung cancer, whether smokers or non-smokers, had lower levels of vitamins (E, C, D3) compared to healthy individuals. Particularly, their vitamin D levels were significantly below average. Additionally, lung cancer patients, especially smokers, showed reduced levels of the superoxide dismutase enzyme compared to healthy individuals. This suggests a potential connection between lower vitamin levels, especially vitamin D, and decreased superoxide dismutase enzyme levels in lung cancer patients.
Keywords: Lung cancer; Superoxide dis-mutase; Vitamin D3; Vitamin E; Vitamin C.
Introduction
An unrestrained growth of cells in the lungs characterizes lung cancer, a harmful tumor. Without proper treatment, this cancerous growth has the potential to progressively spread into nearby tissues or even affect other parts of the body [1]. Primary lung cancer can be categorized into two main types [2]: Non-Small Cell Lung Cancer (NSCLC), which accounts for approximately 85 percent of all diagnosed cases, and Small Cell Lung Cancer (SCLC) are the two main types of lung cancer. Among NSCLC subtypes, adenocarcinomas are the most commonly observed. The prevalence of squamous-cell carcinoma, which used to be the most frequent histological type, has significantly decreased over time. This decline can be partially attributed to decreased smoking rates in high-income nations and variations in cigarette compositions [3].
The risk factors associated with lung cancer are multifaceted, involving the interaction of various variables. These factors include tobacco use, exposure to radon gas, asbestos, radioactive materials like uranium, inhalation of certain chemicals or minerals such as beryllium, cadmium, chromium compounds, diesel exhaust, and air pollution. Additionally, having a family history of lung cancer can also heighten the risk of developing the disease [4].
The lungs can be directly exposed to various factors including elevated oxygen pressure, irritants in the environment, and pollutants. Among these are oxidant gases, ultrafine particulate matter, nanoparticles from industrial pollution, automobile exhaust emissions, and smoking. These exposures result in the lungs producing free radicals. As a result of these factors, the lungs and other organs in the body encounter oxidative stress [5].
The occurrence of lung cancer is connected to nutrition, including the consumption of antioxidants. Antioxidants possess the ability to counteract free radicals and hinder oxidation processes, and this includes vitamins C and E, as well as other phytochemicals. An increased intake of foods rich in antioxidants, Things like fruits and vegetables, has been linked to a reduced risk of cancer, particularly lung cancer [6].
Materials and methods
Patients
The procedure involves collecting a total of 100 blood samples from both normal individuals and patients. These individuals were divided into two groups: Smokers and non-smokers. In the patient group, there were 30 smokers and 30 non-smokers, while in the control group, there were 20 smokers and 20 non-smokers. The blood samples were obtained from Alamal National Hospital for cancer treatment and Baghdad Teaching Hospital, during the period between October 2022 and April 2023. The control group consisted of healthy individuals who did not have diabetes, hypertension, or any history of cancer in their family. To collect the samples, Blood was drawn from each subject using a heparinized catheter and allowed to coagulate at room temperature for 20 minutes. Then, using a micropipette, the serum was transferred to a separate vessel after 10 minutes of centrifugation. The transferred serum was then frozen at -20 degrees Celsius.
Enzymatic activity of SOD
SOD (superoxide dismutase) activity was assessed using a commercially available ELISA kit (Abcam, USA, Cat No: ab119520). This kit enables the accurate measurement of human Cu/Zn SOD levels. Utilizing a Cu/Zn SOD-specific antibody pre-coated on a plate, followed by the addition of a Cu/Zn SOD-specific HRP-conjugated antibody constitutes the assay. Unbound proteins were subsequently removed by washing. Then, a substrate known as TAB was added, which, in the presence of HRP (horseradish peroxidase), catalyzed a reaction resulting in the production of a blue color. Each well was treated with an acidic stop solution, causing a color change from blue to yellow. Using a plate reader, the absorbance of the yellow pigment was measured at 450 nm. (PowerWave STM, BioTek®, USA). The amount of SOD in the samples (measured in ng/mL) is directly related to how bright the yellow color is [7].
Vitamin D 25-hydroxylase immunoassay
Abcam UK's 25 OH Vitamin D Enzyme-Linked Immunosorbent Assay (ELISA) kit provides a convenient way to evaluate 25 OH Vitamin D3 and 25 OH Vitamin D2 concentrations in human plasma and serum. These two vitamin D isomers provide the basis for the assay's detection and quantification. Parent vitamin D3 is synthesized when 7-dehydrocholesterol is exposed to sunlight. This precursor molecule is altered to produce vitamin D3. Vitamin D is also easily accessible from food sources, either naturally occurring or fortified, in the form of parent Vitamin D2. Once these precursor molecules have entered the body, they are taken to the liver, where they are hydroxylated to produce vitamin D 25 OH. The kidneys are responsible for the final step in this metabolite's transformation into 1,25 OH 2 Vitamin D. This last metabolite is vitamin D's active form in the body. The exact assessment of 25 OH Vitamin D3 and 25 OH Vitamin D2 levels in plasma and serum samples is made possible by the 25 OH Vitamin D ELISA kit, which provides important insight into vitamin D status in the body [8].
Human Vitamin E
Mybiosource USA's kit makes use of the ELISA sandwich method using two different antibodies. The kit's pre-coated antibody is a monoclonal anti-human VE antibody, while the detection antibody is a biotinylated polyclonal antibody. After adding samples and biotinylated antibodies to the wells of an ELISA plate and washing with PBS or TBS to eliminate unbound compounds, the plate is read. The wells of the human Vitamin E ELISA kit are then incubated with avidin-peroxidase conjugates. TMB substrate is used for color development after a thorough washing in PBS or TBS to eliminate any unbound enzyme conjugates. The addition of the stop solution (color reagent C) causes the blue product formed by the TMB reaction with the peroxidase activity to change color to yellow. The intensity of the color produced is proportional to the concentration of the target analyte in the sample [8].
Statistical analysis
The data was analyzed using GraphPad Prism 6 (GraphPad Software Inc., La Jolla, CA).Mean and standard deviation (mean SD) were used to represent the data.A t-test was used to compare the two groups statistically.Statistical significance was assumed when the P-value was less than 0.05 [9].
Results
The findings from our study, as depicted in the table and figure below, can be summarized as follows: There was a significant statistical difference (p ≤ 0.0001) in the levels of the Superoxide Dismutase (SOD) enzyme between lung cancer patients who did not smoke (5.38±1.32) and a control group consisting of smokers (10.66±2.0). Additionally, noteworthy variations in SOD enzyme levels were observed when comparing non-smoker individuals within both the patient group (5.38±1.32) and the control group (10.28±2.14), as well as between smoker patients (5.20±1.4) and the smoker control group (10.66±2.0). However, no significant differences were found when comparing the enzyme levels between smokers and non-smokers within the control group or patient group.
In regard to vitamin D3 levels, our study demonstrated a significant statistical difference (p ≤ 0.0001) between non-smoker lung cancer patients () and a control group consisting of smokers (67.74±18.3). Notable variations in vitamin D3 levels were also observed when comparing non-smoker individuals within both the patient group (29.72±15.1) and the control group (78.42±21.3), as well as between smoker patients (26.9±17.5) and the smoker control group (67.74±18.3). However, no significant differences were found when comparing vitamin levels between smokers and non-smokers within the control group or patient group.
Our findings indicate a significant and notable difference (P≤ 0.05) in the concentration of vitamin E solely between lung cancer patients who smoke (12.55±SD) and healthy non-smokers (22.10±SD). However, our study did not reveal any significant differences when comparing vitamin levels between non-smokers in the patient group and the healthy group, smokers within the healthy group and the patient group, or between non-smoking healthy individuals and smoking patients.
Table 1: mean ( SD) serum concentrations of superoxide dismutase (SOD) enzyme, vitamin D3 (ng/mL), vitamin E (g/mL) , and vitamin C (ng/mL) in healthy controls and lung cancer patients who smoked and did not smoke, respectively.
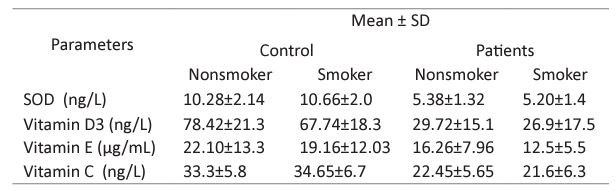
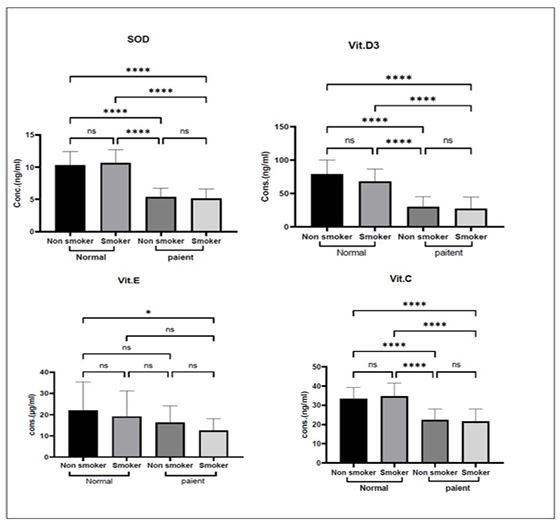
Figure 1: Concentrations of the antioxidant enzyme superoxide dismutase (SOD), vitamin D3 (ng /mL), vitamin E (g /mL), and vitamin C (ng /mL) are depicted graphically for both healthy controls and patients with lung cancer, broken down by smoking status.
NS: non-significant. ***: p ≤ 0.001,**: p ≤ 0.01, *: p ≤ 0.05.
Similarly, we observed a significant statistical difference (p ≤ 0.0001) in the levels of vitamin C between non-smoker lung cancer patients (22.45±5.65) and a control group consisting of smokers (34.65±6.7). Notable variations in vitamin C levels were observed when comparing non-smoker individuals within both the patient group (22.45±5.65) and the control group (33.3±5.8), as well as between smoker patients (21.6±6.3) and the smoker control group (34.65±6.7). However, no significant differences were found when comparing vitamin levels between smokers and non-smokers within the control group or patient group.
Discussion
SODs are the body's primary line of defense versus ROS-induced damage [10] , Catalytically converting oxygen into hydrogen peroxide is the job of SOD, an anti-oxidant enzyme [11]. SOD declines with age, and that means more disease-inducing free radicals [12]. However, the fact that SOD activity was found to be lower than expected in the study hints at a greater consumption of antioxidative enzymes due to elevated oxidative stress [13].
In contrast to our study, previous research conducted by Islam et al. demonstrated reduced activities of CuZn-SOD and Mn-SOD in cancer cells, indicating a potential role for SOD in promoting the reversal of cancer cell phenotypes. These findings suggested that endogenous antioxidant enzymes could potentially regulate cancer development and be targeted for cancer treatment [14]. Similarly, Balaky et al. conducted a study that frequently documented the overexpression of Superoxide dismutase 1 (SOD1) in lung cancers. The study highlighted the essential role of SOD1 in the development of lung disease. These studies present contrasting results to our findings regarding the SOD enzyme levels in lung cancer patients who smoke and non-smoke [15].
Cholesterol-derived vitamin D3 regulates the epigenome and transcriptome in many different human tissues and cells, including cancerous tumor cells. The metabolite 1,25(OH)2D3 and its high-affinity receptor VDR (Vitamin D receptor) are responsible for this control [16].
Vitamin D's effect on cancer has been studied in a number of in vitro and in vivo experiments. These studies have demonstrated that vitamin D exhibits anti-metastatic effects, particularly in lung cancer, as well as other cancer types. Vitamin D has been found to suppress cell growth and reduce invasiveness in lung cancer cells during in vitro investigations. Furthermore, research has established a correlation between vitamin D levels and overall survival in individuals with lung cancer [17]. A lack of vitamin D has been linked to a higher chance of acquiring cancer and a greater probability of dying from the condition, according to research by [J. B. Gibbons et al.,] [18]. A study conducted by (Muller DC) found no evidence of a relationship between the levels of vitamin D in the bloodstream with the possibility of lung cancer at a later stage [19]. This suggests that circulating vitamin D concentrations may not be indicative of the likelihood of a subsequent lung cancer diagnosis.
Apart from its role as an antioxidant that helps reduce oxidative stress and inhibit lipid oxidation, vitamin D3 also plays a crucial role in various physiological processes. These include cell differentiation, regulation of growth and reproduction, support for the immune system, protection against DNA damage in cells, as well as the suppression and prevention of cancer cells [20].
Vitamin E consists of eight naturally occurring compounds that share similar chemical structures. It serves as a crucial dietary antioxidant, found in vegetable sources, nuts, and oils. The antioxidant properties of vitamin E have been associated with numerous health benefits, including its ability to reduce inflammation, fight against cancer, and provide neuroprotective effects [21].
Our study suggests that individuals who are smokers or have lung cancer tend to exhibit lower levels of vitamin E compared to healthy individuals. This finding aligns with the research conducted by (Zabłocka-Słowińska K,) which reported a reduction in vitamin E levels among all patients diagnosed with lung cancer [22].
Vitamin E is essential because it prevents further oxidative damage by neutralizing lipid peroxyl radicals and breaking the chain reaction of peroxidation. The significant decrease in serum levels of vitamin E observed may be attributed to oxidative stress, which can be affected by the presence of cancer and/or metabolic changes. Another possible explanation for the lower concentration of vitamin E is a change in the distribution of alpha-tocopherol. Alpha-tocopherol is predominantly found in the LDL-C fraction of the blood, and as serum lipid levels increase, it tends to move from cellular membranes to circulating lipoproteins. Insufficient levels of vitamin E can make individuals more susceptible to dyslipidemia-related factors [22].
L-ascorbic acid, commonly known as vitamin C, has been identified as a crucial element in the management of scurvy [23]. Vitamin C has several significant functions, with its most notable roles including neutralizing free radicals, regenerating vitamin E, acting as a cofactor for hydroxylase enzymes involved in collagen and neurotransmitter synthesis, and regulating gene expression [24]. Those with active inflammation and cancer, particularly haematological malignancies, have been found to have lower levels of plasma and cellular ascorbate, according to research by (L. Zhu and L. Chen). Ascorbate levels drop when a person is sick, and this is thought to be due to increased turnover brought on by oxidative and metabolic stress [25].
Conclusions
our study indicates that smoking status is associated with significant differences in vitamin levels, including the Superoxide Dismutase (SOD) enzyme, vitamin D3, vitamin E, and vitamin C, in relation to lung cancer. However, no significant differences were found when comparing vitamin levels between smokers and non-smokers within the same group. These findings underscore the importance of considering smoking status when studying the relationship between vitamins and lung cancer risk.
Acknowledgements: Zubaida expresses gratitude to everybody who assisted in the completion of this research.
Conflict of interest: The authors report no relevant financial relationships to declare.
Finance: No financial information is being shared in this study.
Confirmation of Article Submission Exclusivity: I am writing to confirm that the article titled "[Role of superoxide dis-mutase in sera of Iraqi lung cancer patients]" has not been published elsewhere and has not been submitted to any other journal for publication consideration.
References
- N Akhtar, JG Bansal. “Risk factors of Lung Cancer in nonsmoker,” Curr Probl Cancer. 2017; 41: 328-339.
- ASG. Abdel-Salam, M Mollazehi, D Bandyopadhyay, AM Malki, Z Shi, et al. Assessment of lung cancer risk factors and mortality in Qatar: A case series study. Cancer Rep. 2021; 4: 1-7.
- Thai, BJ. Solomon, L. V Sequist, J. F. Gainor, and R. S. Heist, “Seminar Lung cancer,” Lancet. 2021; 398: 535-554.
- AA Jasim, BH Bahir. Assessment of Risk Factors of Lung Cancer Patients in Babylon Governorate Assessment of Risk Factors of Lung Cancer Patients in Babylon Governorate , Iraq. 2020; 1-6.
- M Zalewska-Ziob, et al. Activity of Antioxidant Enzymes in the Tumor and Adjacent Noncancerous Tissues of Non-Small-Cell Lung Cancer. Oxid Med Cell Longev. 2019; 2019.
- S Antioxidants, S Trial. Association between Dietary and Supplemental Antioxidants Intake and Lung Cancer Risk : Evidence from a Cancer Screening Trial. 2023.
- SB Mohamed, FA Hassan. The evaluation of Paclitaxel effects on the Caco-2 cell line of colon cancer patients. J Pharm Negat Results. 2022; 13: 459-463.
- MY Thabeet. “No Title”, neuroquantology. 20: 5562-5568.
- MY Thabeet, PFA Hassan. Antioxidant Status And The In Vitro Effect Of Amylase And Lipase Enzymes On Iraqi Pancreatic Cancer Patients. 2022.
- H Younus. Therapeutic potentials of superoxide dismutase. Int J Health Sci. (Qassim). 2018; 12: 88-93.
- Y Tang, et al. Metabolic Adaptation-Mediated Cancer Survival and Progression in Oxidative Stress. 2022; 1-26.
- S George, H Abrahamse. Redox potential of antioxidants in cancer progression and prevention, Antioxidants. 2020; 9: 1-21.
- X Zhu, E Blanco, M Bhatti, A Borrion. Sci Total Environ. 2020; 143747.
- MN Islam, et al. Superoxide dismutase: An updated review on its health benefits and industrial applications. Crit Rev Food Sci Nutr. 2021; 1-19.
- HM Balaky. Evaluating the Levels of Oxidative DNA Damage, Antioxidant Profile and Pro-inflammatory Cytokines in Lung Cancer Patients. 2023; 64: 45-55.
- C Carlberg, E Velleuer. Vitamin D and the risk for cancer: A molecular analysis. Biochem Pharmacol. 2022; 196: 2022.
- M Gaudet, M Plesa, A Mogas, N Jalaleddine, Q Hamid, et al. Recent advances in vitamin D implications in chronic respiratory diseases. Respir Res. 2022; 23: 1-14.
- JB Gibbons, et al. Association between vitamin D supplementation and COVID-19 infection and mortality. Sci Rep. 2022; 12: 1-12.
- DC Muller, et al. No association between circulating concentrations of vitamin D and risk of lung cancer : an analysis in 20 prospective studies in the Lung Cancer Cohort Consortium ( LC3 ) Original article. 2018; 1468-1475.
- T Ao, J Kikuta, M Ishii. The Effects of Vitamin D on Immune System and Inflammatory Diseases. 2021; 1-9.
- J Donnelly, A Appathurai, H Yeoh, K Driscoll, W Faisal. Vitamin E in Cancer Treatment : A Review of Clinical Applications in Randomized Control Trials. 2022; 1-13.
- K Zabłocka-Słowińska, et al. Oxidative stress in lung cancer patients is associated with altered serum markers of lipid metabolism. PLoS One. 2019; 14.
- M Dosed, et al. Vitamin C-Sources, Physiological Role, Kinetics, Deficiency, Use, Toxicity, and Determination. 2021; 1-34.
- M Villagran, J Ferreira, M Martorell, L Mardones. The role of vitamin C in cancer prevention and therapy: A literature review, Antioxidants. 2021; 10: 1-15.
- A Ang, JM Pullar, MJ Currie, MCM Vissers. Vitamin C and immune cell function in inflammation and cancer. Biochem Soc Trans. 2018; 46: 1147-1159.

