Case Report - Volume 3 - Issue 5
Successful treatment of cystoid macular edema in central retinal vein occlusion with retinitis pigmentosa: A case report and literature review
Esmaeil Babaei1; Abdulrahman Pordel1; Mohammad Shiravani2; Mohammad Mohammadi1; Alireza Attar2; Mohsen Gohari1*
1Poostchi Ophthalmology Research Center, Department of Ophthalmology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
2Geriatric Ophthalmology Research Center, Shahid Sadoughi University of medical sciences, Yazd, Iran.
Received Date : July 22, 2023
Accepted Date : Sep 05, 2023
Published Date: Sep 12, 2023
Copyright: © Mohsen Gohari 2023
*Corresponding Author: Mohsen Gohari, Geriatric Ophthalmology Research Center, Shahid Sadoughi University of medical sciences, Yazd, Iran.
Email: goharimo@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1545
Abstract
We present a case of a 41-year-old man with a known history of retinitis pigmentosa who experienced severe vision loss in the left eye due to Central Retinal Vein Occlusion (CRVO). The patient sought medical attention one day after the onset of vision loss, with all systemic workups yielding normal results. Anterior segment examination revealed no abnormalities, and a dilated fundoscopic examination of the left eye showed a congested optic nerve, dilated retinal veins, and hemorrhages. Fluorescein angiography confirmed an ischemic CRVO. The initial Central Macular Thickness (CMT) measured 787um. Following three doses of intravitreal anti-VEGF (bevacizumab) over one week, CMT decreased to 183um, resolving central macular edema and improving visual acuity. This case represents the fourth reported instance of retinitis pigmentosa with CRVO. Intravitreal anti-VEGF treatment appears efficacious for addressing cystoid macular edema secondary to retinitis pigmentosa with CRVO.
Keywords: Retinitis pigmentosa (RP); Central retinal vein occlusion (CRVO); Anti-VEGF (vascular endothelial growth factor); Cystoid macular edema (CMT).
Abbreviations: CRVO: Central Retinal Vein Occlusion; CMT: Central Macular Thickness; VEGF: Vascular Endothelial Growth Factor; IRD: Inherited Retinal Dystrophy; RP: Retinitis Pigmentosa; CME: Cystoid Macular Edema; BCVA: Best Corrected Visual Acuity; IOP: Intraocular Pressure; SD-OCT: Spectral Domain Optical Coherence Tomography; FFA: Fundus Fluorescein Angiography; BP: Blood Pressure, CBC: Complete Blood Cell Count; ESR: Estimation Sedimentation Rate; CRP: C-Reactive Protein, LDL-C: Low-Density Lipoprotein Cholesterol; RBC: Red Blood Cell; PS: Protein S.
Introduction
Inherited Retinal Dystrophy (IRD) is a diverse range of diseases characterized by the degeneration of retinal cells due to genetic factors. Among these, Retinitis Pigmentosa (RP) is the most prevalent and is a leading cause of visual impairment in most countries [1]. RP is a clinically and genetically heterogeneous group of retinal degenerations primarily affecting the peripheral photoreceptors. The estimated prevalence is approximately 1 in 3000 individuals [2]. It is characterized by a progressive loss of vision, initially presenting as night blindness, followed by the gradual decline of peripheral visual fields. It is often accompanied by central vision deterioration [3]. Furthermore, RP patients may also experience infrequent ocular problems, such as Central Retinal Vein Occlusion (CRVO) [4]. The occurrence of Cystoid Macular Edema (CME) in RP patients with CRVO is exceptionally rare. Considering the limited studies on the use of intravitreal anti-Vascular Endothelial Growth Factor (anti-VEGF) medications for managing CME secondary to RP, we present a case of CME in RP with CRVO that was successfully treated with bevacizumab.
Case Presentation
A 41-year-old man with no remarkable past medical and family history, known to have retinitis pigmentosa, presented to the outpatient department of ophthalmology at XXX hospital affiliated with XXX. He complained of blurred vision in his left eye that had persisted for one day. Upon examination, his Best Corrected Visual Acuity (BCVA) was hand motion in the left eye and 2-meter finger count in the right eye. Intraocular Pressure (IOP) was 12 mmHg in the left eye and 11 mmHg in the right eye. The anterior segment examination of both eyes revealed clear corneas and a normal anterior chamber. Relative Afferent Pupillary Defect (RAPD) was positive in the left eye. Color fundus photography using Zeiss Clarus 500 (Germany) showed mild peripheral hyperpigmentary spots resembling bone-spicules in the left eye. Additionally, congested optic nerve with tortuous and dilated veins scattered throughout the fundus, along with dot, blot, and flame-shaped hemorrhages, were observed. A few yellowish-white cotton-wool spots were also noted (Figure 1).
Spectral Domain optical coherence tomography (SD-OCT) using Spectralis OCT (Heidelberg Engineering, Germany) revealed a central macular thickness (CMT) of 787 μm in the left eye, indicating cystoid macular edema with sub-foveal fluid (Figure 2).
Fundus Fluorescein Angiography (FFA) with Heidelberg Retina Angiograph (Heidelberg Engineering, Germany) in the left eye exhibited marked hypo fluorescence in the macula, consistent with the blocking effect of retinal hemorrhages and an area of capillary non-perfusion (Figure 3).

Figure 1: Dot, blot, and flame-shaped hemorrhages with cotton-wool spots and congested optic nerve in fundoscopic examination of the left eye.
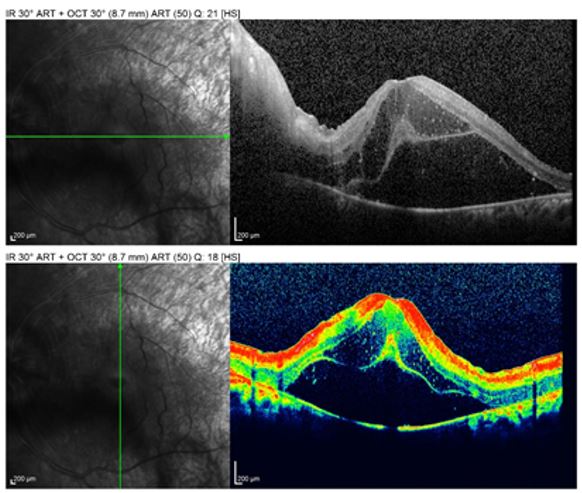
Figure 2: Cystoid macular edema with subfoveal fluid in patient’s left eye.
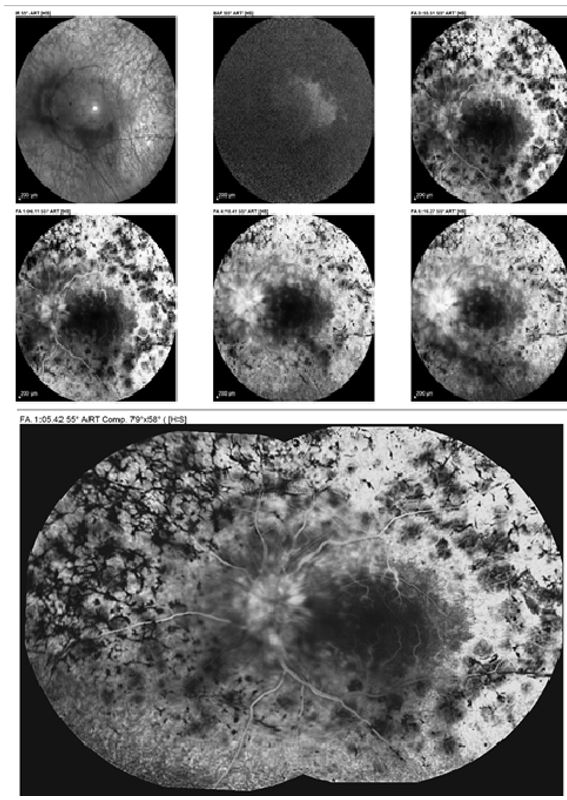
Figure 3: Marked hypo fluorescence in macula, consistent with the blocking effect of retinal hemorrhages and the area of capillary non perfusion in angiography of the left eye.
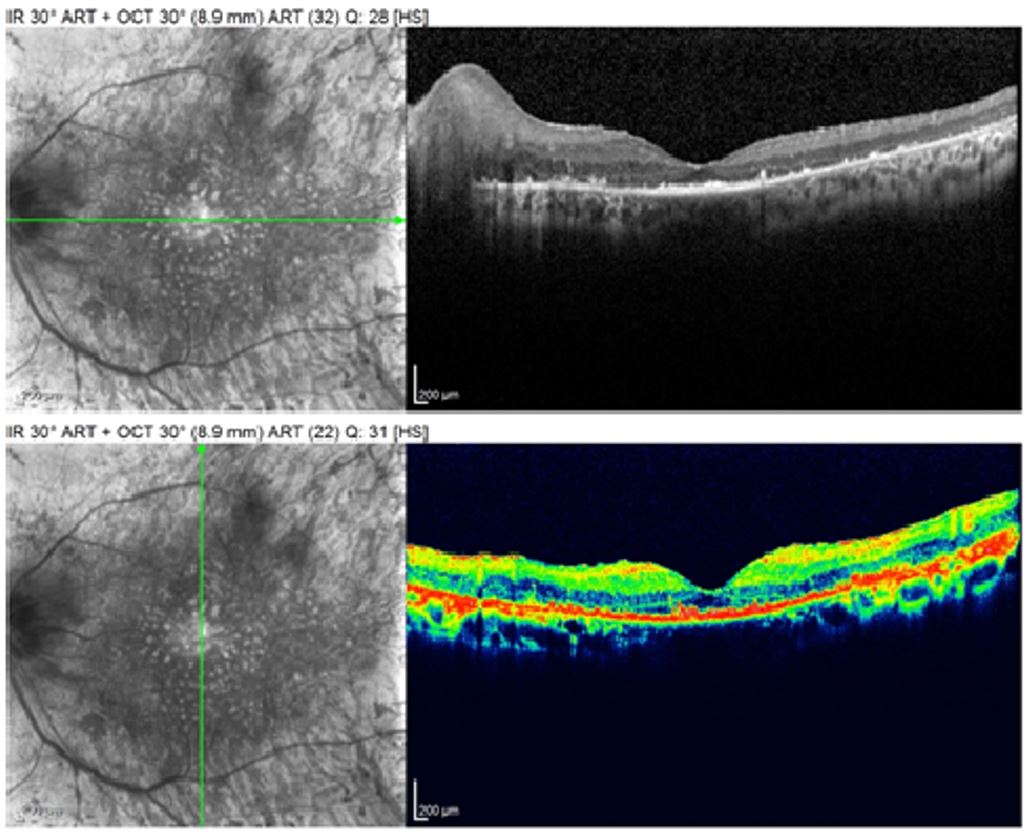
Figure 4: Regressive edema cystoid macular after 3-time Anti-VEGF injection.
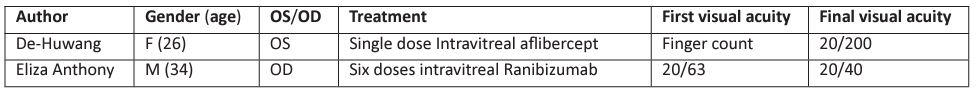
Table1: Case reports of CRVO in RP (2022-2023).
Further systemic examinations, including chest X-ray, arterial Blood Pressure (BP), Complete Blood Cell Count (CBC), Estimation Sedimentation Rate (ESR), C-Reactive Protein (CRP), blood sugar level, hemoglobin, Low-Density Lipoprotein Cholesterol (LDL-C), and the detection of parameters indicating inflammatory and infectious diseases, were performed. No systemic diseases were found, and the results of laboratory investigations were within normal limits. Based on the above findings, the patient was diagnosed with CRVO secondary to retinitis pigmentosa with macular edema in the left eye. The patient underwent three intravitreal injections of off-label Anti-VEGF bevacizumab (1.25 mg/0.05 mL Avastin) over a period of one month. One week after completing the three doses of intravitreal bevacizumab, OCT scan showed a significant decrease in CMT (183 μm), and macular edema completely resolved. The patient's BCVA improved to 3-meter finger count (Figure 4).
Discussion
To date, only three previous cases of retinitis pigmentosa (RP) with ischemic central retinal vein occlusion (CRVO) have been reported [5,6,7];that we summarize in (Table 1).
Previous studies have indicated that RP is associated with a decline in retinal and choroidal blood flow [8,9]. In a study by Yang et al., they investigated the blood characteristics in nonsyndromic RP and observed that RP induces Red Blood Cell (RBC) aggregation and platelet activation, resulting in blood stasis, that further triggers apoptosis [10]. Additionally, certain mutations associated with thromboembolic disorders have been reported in RP patients [11,12]. Bushehri et al. identified homozygous mutations in the Protein S (PS) gene, responsible for vitamin K-dependent anticoagulant plasma PS synthesis. It is described as a potential candidate gene for juvenile RP [11,13,14]. However, Ghribeh et al. reported no significant difference in the presence of thrombophilic mutations between RP patients and controls [15]. Another probable explanation for CRVO in RP could be the migration of retinal pigment epithelium cells into the inner retina, forming a continuous monolayer around thin-walled venules or capillaries. This leads to the deposition of extracellular matrix between the retinal pigment epithelium and vascular endothelial cells, resulting in vascular wall thickening and subsequent vessel occlusion [16]. This mechanism could potentially explain the occurrence of CRVO and subsequent CME in RP. Macular Edema (ME) is a significant complication of retinal vein occlusion, greatly impacting patients' vision [17]. Cystoid Macular Edema (CME) is observed in 10-50% of RP patients when assessed using optical coherence tomography (OCT) [18,19]. Currently, there is no definitive treatment to halt or reverse photoreceptor degeneration. However, complications such as CME have been managed using various approaches. Treatment options for CME secondary to retinitis pigmentosa include oral and topical carbonic anhydrase inhibitors, intravitreal steroids, oral corticosteroids, grid laser photocoagulation, pars plana vitrectomy, ketorolac, and intravitreal anti-Vascular Endothelial Growth Factor (anti-VEGF) agents such as ranibizumab and bevacizumab [20]. In recent years, inhibition of Vascular Endothelial Growth Factor (VEGF) has garnered attention [21]. Artunay et al. conducted a study assessing the anatomical, clinical, and visual acuity response following intravitreal ranibizumab injection in patients with CME due to RP. Their findings suggested that intravitreal ranibizumab may offer a novel therapeutic approach for treating CME secondary to RP, with no associated adverse events reported. Further experience with intravitreal ranibizumab in this population will help establish its long-term efficacy [22]. Another study by Yuzbasioglu et al. evaluated the effectiveness and outcomes of intravitreal bevacizumab injections in RP patients. They demonstrated that intravitreal bevacizumab administration effectively reduced CME in RP, as evidenced by a decrease in central macular thickness following treatment [23].
In the presented case, Cystoid Macular Edema (CME) secondary to Central Retinal Vein Occlusion (CRVO) was successfully treated with monthly intravitreal injections of bevacizumab for three times. There were no signs of relapse or anterior segment neovascularization during the two-year follow-up period. further, in a previous case report where macular edema in CRVO patients was treated with a single dose of aflibercept. However, in that specific case, the macular edema relapsed after three months following the treatment [5]. It's remarkable that in all cases of CRVO in patients with Retinitis Pigmentosa (RP) neovascularization was not observed during follow-up. also, there was an improvement in Best-Corrected Visual Acuity (BCVA) observed in all cases after the administration of anti-VEGF (vascular endothelial growth factor) injections.
Conclusions
Central retinal vein occlusion secondary to retinitis pigmentosa is a rare condition. However, it is necessary for ophthalmologists to be aware of the condition in order to provide timely management. The use of intravitreal anti-vascular endothelial growth factor drugs has shown effectiveness in treating cystoid macular edema associated with RP and CRVO. Therefore, considering this potential treatment option can significantly contribute to the successful management of CME in RP patients with CRVO.
Conflict of interest: The authors declare no potential conflicts of interest for this article.
Acknowledgment: None.
References
- Verbakel SK, van Huet RA, Boon CJ, den Hollander AI, Collin RW, et al. Non-syndromic retinitis pigmentosa. Progress in retinal and eye research. 2018; 66: 157-86.
- Bundey S, Crews SJ. A study of retinitis pigmentosa in the City of Birmingham. I Prevalence. Journal of medical genetics. 1984; 21: 417-20.
- Bird AC. Retinal photoreceptor dystrophies LI. Edward Jackson memorial lecture. American journal of ophthalmology. 1995; 119: 543-62.
- Paxhia Mj, Daniel Ting T, Fekrat S. Ischemic Central Retinal Vein Occlusion And Retinitis Pigmentosa: Lower Risk of Neovascularization? RETINA. 2001; 21: 179-80.
- Wang DH, Gu C, Yuan YZ. Case Report: A Case of Cystoid Macular Edema in Retinitis Pigmentosa With Central Retinal Vein Occlusion. Front Med (Lausanne). 2022; 9: 877429.
- Anthony E, Baskaran P, Rajamani A, Rajendran A. Bilateral Occlusive Vasculitis Associated with Retinitis Pigmentosa - A Case Report. Ocul Immunol Inflamm. 2023; 31: 215-9.
- Paxhia MJ, Ting TD, Fekrat S. Ischemic central retinal vein occlusion and retinitis pigmentosa: lower risk of neovascularization? Retina. 2001; 21: 179-80.
- Cellini M, Strobbe E, Gizzi C, Campos EC. ET-1 plasma levels and ocular blood flow in retinitis pigmentosa. Canadian journal of physiology and pharmacology. 2010; 88: 630-5.
- Falsini B, Anselmi GM, Marangoni D, D'Esposito F, Fadda A, et al. Subfoveal choroidal blood flow and central retinal function in retinitis pigmentosa. Investigative ophthalmology & visual science. 2011; 52: 1064-9.
- Yang Y, Deng Y, Tian Y, Yao Z, Zhou Y, Wang Y, et al. Investigation of blood characteristics in nonsyndromic retinitis pigmentosa: A retrospective study. Journal of Ophthalmology. 2019; 2019.
- Bushehri A, Zare-Abdollahi D, Alavi A, Dehghani A, Mousavimikala M, et al. Identification of PROS1 as a Novel Candidate Gene for Juvenile Retinitis Pigmentosa. Int J Mol Cell Med. 2019; 8: 179-90.
- Al-Khersan H, Shah KP, Jung SC, Rodriguez A, Madduri RK, et al. A novel MERTK mutation causing retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2017; 255: 1613-9.
- Castoldi E, Hackeng TM. Regulation of coagulation by protein S. Current opinion in hematology. 2008; 15: 529-36.
- Pintao MC, Garcia A, Borgel D, Alhenc-Gelas M, Spek C, et al. Gross deletions/duplications in PROS1 are relatively common in point mutation-negative hereditary protein S deficiency. Human genetics. 2009; 126: 449-56.
- Gharaibeh AM, Awidi AS, Ababneh OH, Abu-Ameerh MA, Awidi MA, et al. Prevalence of thrombophilic genetic factors among patients with retinitis pigmentosa. Retina. 2014; 34: 2147-50.
- Milam AH, Li Z-Y. Retinal pathology in retinitis pigmentosa: Considerations for therapy. Degenerative diseases of the retina. 1995: 275-84.
- Loskutova E, Nolan J, Howard A, Beatty S. Macular pigment and its contribution to vision. Nutrients. 2013; 5: 1962-9.
- Amato A, Arrigo A, Aragona E, Manitto MP, Saladino A, et al. Gene therapy in inherited retinal diseases: An update on current state of the art. Frontiers in Medicine. 2021; 1860.
- Strong S, Liew G, Michaelides M. Retinitis pigmentosa-associated cystoid macular oedema: pathogenesis and avenues of intervention. British journal of ophthalmology. 2017; 101: 31-7.
- Bakthavatchalam M, Lai FHP, Rong SS, Ng DS, Brelen ME. Treatment of cystoid macular edema secondary to retinitis pigmentosa: a systematic review. Surv Ophthalmol. 2018; 63: 329-39.
- Stewart MW, editor The expanding role of vascular endothelial growth factor inhibitors in ophthalmology. Mayo Clinic Proceedings; Elsevier. 2012.
- Artunay O, Yuzbasioglu E, Rasier R, Sengul A, Bahcecioglu H. Intravitreal ranibizumab in the treatment of cystoid macular edema associated with retinitis pigmentosa. J Ocul Pharmacol Ther. 2009; 25: 545-50.
- Yuzbasioglu E, Artunay O, Rasier R, Sengul A, Bahcecioglu H. Intravitreal bevacizumab (Avastin) injection in retinitis pigmentosa. Curr Eye Res. 2009; 34: 231-7.

