Case Report - Volume 3 - Issue 5
Acute traumatic tentorial subdural hematoma: A diagnostic challenge
Hakan Ak*; Yener Çakir; Onur Burgucu
Kırşehir Ahi Evran University, faculty of medicine, Department of Neurosurgery, Kırşehir/Turkey.
Received Date : July 26, 2023
Accepted Date : Sep 06, 2023
Published Date: Sep 13, 2023
Copyright: © Hakan AK 2023
*Corresponding Author: Hakan AK, Kırşehir Ahi Evran University,
Faculty of medicine, Department of Neurosurgery, Kırşehir/Turkey.
Email: nrsdrhakanak@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1546
Abstract
Acute subdural hematoma is a complication of head trauma with high mortality and morbidity rates. Sometimes, subdural hematomas are named according to the location. Tentorial subdural hematoma is one of these hematoma types and is rarely seen. It mostly has a benign course, and surgery may be required very rarely. In this report, a 47 years old male patient who was diagnosed with tentorial subdural hematoma as a complication of head trauma due to fall is presented. The patient was followed with conservative treatment. As a result, close clinical, neurological and radiological follow-up may be sufficient for tentorial subdural hematoma.
Introduction
Subdural hematomas are mostly located on the frontal, temporal and parietal surfaces over convexity [1]. However, there are also subdural hematoma types, which are called by various names according to the location like peritentorial, and pure tentorial vs vs [2,3]. However, the main classification of subdural hematomas is based on the bleeding time as acute, subacute and chronic [4,5-9]. Acute tentorial subdural hematomas are rare among these types. Although it generally has a benign course, sometimes it may be complicated [6,7].
In this presentation, a case of acute tentorial subdural hematoma due to falling in a 47-year-old male patient is presented in the light of the literature.
Case Presentation
A 47-year-old male patient was brought to the emergency department with complaints of headache and altered consciousness as confused due to falling from the same level. He was inclined to sleep. Glasgow Coma Score was 15. The patient had no history of additional diseases such as hypertension or diabetes mellitus. He had no history of using any anticoagulant or antiaggregant drugs. A 7mm hyperdense area was detected in the left tentorial area on brain Computed Tomography (CT) (Figure 1). Although hematoma was initially considered in the first plane, a brain Magnetic Resonance Imaging (MRI) was performed for the differential diagnosis (Figure 2a,b,c). According to these findings, acute tentorial hematoma was diagnosed and the patient was admitted to the ward. The patient was given mannitol and furosemide for three days. The patient's level of consciousness returned to normal, and he did not have a tendency to sleep. CT angiography was performed for the differential diagnosis of possible accompanying lesion such as fistula or aneurysm. Any accompanying lesion was not detected. The patient, whose general condition was good, was discharged. On the 10 day after dischage, complete resolution of the hematoma is detected on control CT (Figure 3).
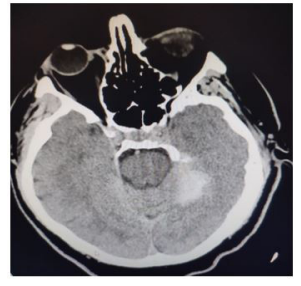
Figure 1: Brain CT of the patient at the admission showing a left sided hyperdense lesion on axial plane.
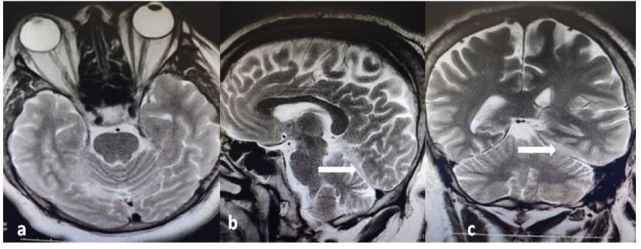
Figure 2a,b,c: Axial, sagittal and coronal plane images of MRI showing tentorial hematoma.
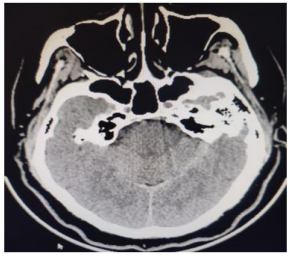
Figure 3: Brain CT of the patient at the admission showing complete resolution of the hematoma.
Discussion
Subdural hematomas are clinically classified as acute, subacute and chronic, mostly according to bleeding time. Acute hematomas are hyperdense on CT, subacute ones are isodense, and chronic ones are hypodense [4,5,9]. Since subdural hematomas develop due to bleeding of the bridging veins, they are mostly located on the frontal, temporal and parietal surfaces over the convexity [1]. However, interhemspheric, peritentorial, parafalcine and pure tentorial localizations have also been reported in the literature [2,3,6,10-13].
Tentorial hematomas, which are among them, are rarely seen and the literature mostly consists of case reports [11]. Although the exact mechanism of tentorial subdural hematomas is not known exactly, it develops due to bleeding of the bridging veins adjacent to the tentorium into the straight sinus or tentorial sinus [11]. However, Ciochon et al reported a case of acute tentorial hematoma due to posterior cerebral artery rupture following minor trauma in 2020 [6]. Moreover, Bhogal et al. published a case of tentorial subdural hematoma due to dural arteriovenous fistula in [7].
Although CT is usually sufficient in the diagnosis of subdural hematoma, it is possible that the diagnosis may be difficult in some cases as in tentorial hematomas [4,9]. In our case, a left sided hyperdense lesion was seen on brain CT at the admission and it was considered as bleeding, however MRI was performed due to lack of experience with tentorial subdural hematoma. Bleeding was clearly demonstrated on MRI, especially in sagittal and coronal sections. When the differential diagnosis is in doubt due to the inability to perform coronal and sagittal reformats in most centers in tomography, cross-sectional MRI, especially in the coronal and sagittal plane may be helpfull in the diagnosis and differential diagnosis.
Although the generally accepted treatment for acute subdural hematomas is surgical treatment, when the recent literature is examined in detail, it is seen that it may be sufficient in selected cases in close follow-up without surgery [9]. Tentorial subdural hematomas generally have are benign course and surgical intervention is usually not required. However, in two studies reported in the literature, surgical intervention was performed due to accompanying pathologies to tentorial subdural hemorrhages [6,7]. In our case, surgical intervention was not required because of the good clinical and neurological course and the absence of additional intracranial pathology.
Conclusion
Although tomography is usually sufficient in the diagnosis of subdural hematoma, it is possible that the diagnosis may be difficult in cases where there is no eye familiarity, as in tentorial hematomas. Therefore, MRI with cross-sections, especially in the coronal and sagittal planes, will be helpful in the diagnosis of suspected cases.
Conflict of interest: It has no affiliation or involvement with any organization or person with a financial interest in the topics or materials discussed in the article. All authors have read and approved the final version of the article.
References
- Aromatario M, Torsello A, D’Errico S, Bertozzi G, Sessa F, et al. Traumatic Epidural and Subdural Hematoma: Epidemiology, Outcome, and Dating. Medicina. 2021; 57:125
- Ak H, Daltaban İS, Albayrak L, Çaltekin İ. Atipik şikayetlerle prezente olan akut travmatik interhemisferik subdural hematom. Bozok Tıp Dergisi. 2018; 8: 100-103.
- AMİN O. Acute interhemispheric subdural hematomas: A report of 3 cases and review of the literature. Çukurova Üniversitesi Tıp Fakültesi Dergisi. 2014; 39: 137-142.
- Şanlı D, Ünal Ö, Bora A, Beyazal M, Yavuz A, et al. Diffusion-weighted MRI in the diagnosis of intracranial hematomas. Eastern journal of medicine. 2013; 18: 185-194.
- Alves JL, Santiago JG, Costa G, Mota Pinto A. A Standardized Classification for Subdural Hematomas- I. Am J Forensic Med Pathol. 2016; 37: 174-8.
- Ciochon UM, Steuble Brandt EG, Stavngaard T. Acute tentorial subdural hematoma caused by rupture of the posterior cerebral artery after minor trauma-A Case Report. Diagnostics (Basel). 2020; 10: 175.
- Bhogal P, Yeo LL, Söderman M. Dural Arteriovenous Fistula Presenting as Tentorial Subdural Hemorrhage : Case Report and Review of theLiterature. ClinNeuroradiol. 2019; 29: 555-561.
- Kim J. Enlarging acute tentorial subdural hematoma evacuated by surgery. Int Med Case Rep J. 2019; 12: 103-107.
- Alshora W, Alfageeh M, Alshahrani S, Alqahtani S, Dajam A, et al. Diagnosis and management of subdural hematoma: a review of recent literature. Int J Community Med Public Health. 2018; 5: 3709-3714.
- Ahn JM, Lee KS, Shim JH, Oh JS, Shim JJ, et al. Clinical Features of Interhemispheric Subdural Hematomas. Korean J Neurotrauma. 2017; 13: 103-107.
- Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Yatsushige H, et al. Traumatic peritentorial subdural hematomas: A study of 32 cases. TurkNeurosurg. 2012; 22: 305-8.
- Cragun BN, Noorbakhsh MR, Hite Philp F, Suydam ER, Ditillo MF, et al. Traumatic parafalcine subdural hematoma: A clinically benign finding. J Surg Res. 2020; 249: 99-103.
- Kim SW, Kang HG. Delayed-onset subdural hematoma after mild head injury with negative initial brain imaging. J Integr Neurosci. 2022; 21: 69.

