Case Report - Volume 3 - Issue 5
Secondary syphilis presenting as pulmonary nodules: A case report and review of the literature
Yinan Li1; Lantao Li2; Bin Ding1; Ye Wang3; Lili Liu1*
1Department of pathology, Affiliated Qingdao Central Hospital of Qingdao University, Qingdao Cancer Hospital, Qingdao, 266000,China.
2Department of radiology, Affiliated Qingdao Central Hospital of Qingdao University, Qingdao Cancer Hospital, Qingdao, 266000,China.
3Department of pathology, The Affiliated Hospital of Qingdao University, Qingdao, 266000, China
Received Date : August 21, 2023
Accepted Date : Sep 21, 2023
Published Date: Sep 28, 2023
Copyright: © Lili Liu 2023
*Corresponding Author : Lili Liu, Department of pathology, Affiliated
Qingdao Central Hospital of Qingdao University, Qingdao Cancer Hospital, Qingdao, 266000, China.
Email: lili2005027@126.com
DOI: Doi.org/10.55920/2771-019X/1557
Abstract
Background: Syphilis is a chronic infectious disease caused by Treponema pallidum (TP). However, pulmonary involvement of syphilis is rare. In addition, HIV infection may lead to secondary syphilis, in which the clinical symptoms are not typical and difficult to diagnose.
Case presentation: A 39-year-old man visited our hospital because of cough for one month. A chest computed tomography (CT) scan showed multiple pulmonary nodules, suggesting the possibility of a benign tumor. Serum tests showed that syphilis spiral antibody and human immunodeficiency virus (HIV) were positive. This patient was diagnosed with secondary syphilis based on medical history, imaging manifestations and pathological findings.
Conclusions: We report a case of pulmonary nodules caused by syphilis secondary to HIV infection. As the symptoms are not typical, auxiliary examination has some limitations in addition to the complexity of the pathological basis, and there are still difficulties in clinical diagnosis.
Keywords: Treponema pallidum, Lung, Syphilis, pathological characteristics.
Abbreviations
TP: Treponema pallidum
CT: Computed tomography
HIV: Human immunodeficiency virus
TSGF: Tumor-specific growth factor
HU: Hounsfield unit
Introduction
Syphilis is a chronic infectious disease caused by Treponema pallidum (TP). It is mainly transmitted through sexual intercourse. Syphilis can also infect fetuses through mother-to-fetus transmission. Syphilis can invade the genitals and skin in the early stage. It often invades the central nervous system or cardiovascular system in the late stage but rarely affects the lungs [1, 2]. The prevalence of the disease has increased all over the world in recent years [3]. In addition, HIV infection usually results in secondary syphilis due to immune deficiency, and clinical manifestations are usually nonspecific, which poses a challenge for clinical diagnosis [4]. Here, we report a case of pulmonary nodules in an HIV-positive patient diagnosed with secondary syphilis.
Case description
A 39-year-old man visited our hospital because of cough for one month. A CT scan showed multiple pulmonary nodules, and the larger nodule was located on the left side of the esophagus, suggesting the possibility of a benign tumor. The patient had no weight loss or gastrointestinal symptoms and no family history. Physical examination revealed that the body temperature was 36.4°C, blood pressure was 110/78 mmHg, respiration rate was 23 breaths/min and pulse rate was 100 beats/min. There were no skin rashes or erythema. No abnormal lung sounds, heart sounds, neurological findings or enlarged lymph nodes were noted.
Laboratory tests showed the following: white blood cell count was 6.51*109/L (1.80-6.30*109/L) with 77% neutrophils and 12.8% monocytes. The red blood cell count was 4*1012/L (4.30-5.80*1012/L), and the hemoglobin content was 108 g/L (120-160 g/L). The carcinoembryonic antigen level was 1.96 ng/mL (standard value: 0-5.09 ng/mL), and the tumor-specific growth factor (TSGF) level was 73 U/mL (standard value: 0-64 U/mL). Human immunodeficiency virus (HIV) and anti-tp testing were positive.
CT showed that the nodules were adjacent to the mediastinum in the left and right lower lobes of the lung with smooth margins. The size of the left nodule was 54*32*22 mm, and that of the right nodule was 45*21*23 mm. The CT value was approximately 35 HU on the plain scan, 64 HU in the arterial phase, and 55 HU in the venous phase. There was no pleural effusion or enlarged lymph nodes (Figure 1)
Differential diagnosis and treatment
The patient was clinically suspected to have a benign lung tumor. Thus, thoracoscopic resection of the pulmonary mass was performed. Intraoperative exploration revealed that the tumor was grayish-yellow, with clear boundaries and a slightly tough texture.
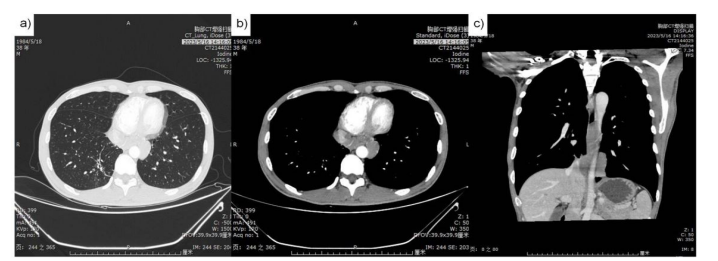
Figure 1: Chest computed tomography.
a) Two nodules around to mediastinum in left (S7+8) and right (S7) lower lobes of the lung with smooth margins.
b) Arterial phase images of the nodules (CT value was about 64HU).
c) Venous phase images of the nodules (CT value was about 64HU).
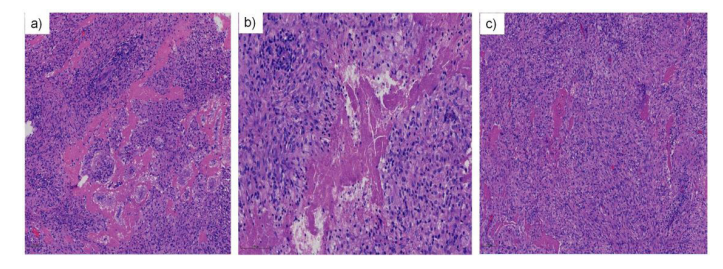
Figure 2: Representative pictures of histological results. (original magnification×40, hematoxylin and eosin staining).
a) Hromboangiitis obliterans and periarteritis could be seen in the center of the necrosis.
b) Multifocal coagulative necrosis, but less complete than tuberculous necrosis.
c) A certain number of plasma cells were infiltrated around the necrosis.
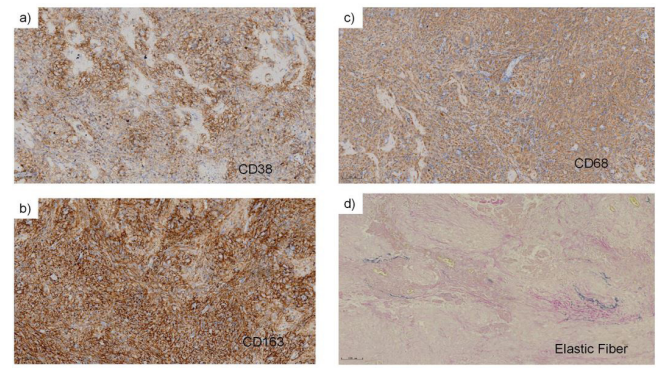
Figure 3: Immunohistochemistry and specific stain examinations (original magnification×40).
a) & b) Immunohistochemistry of CD38 and CD163 showed infiltration of histiocytes around the necrosis.
c) CD68 showed infiltration of plasmocyte. d) Elastic fiber staining showed the outline of residual blood vessels.
Histopathological examinations were as follows: pulmonary nodules showed chronic granulomatous inflammation. Coagulative necrosis was visible; however, it was not as complete as tuberculosis, and the shape of necrosis was irregular. There were abundant epithelioid cells around the necrosis, and a certain amount of plasma cells and histiocytes infiltrated, accompanied by a small amount of multinucleated giant cells and Langhans giant cells. In addition, thromboangiitis obliterans and periarteritis could be found easily (Figure 2). Immunohistochemistry revealed that histiocytes were CD68- and CD163-positive, and plasmocytes were CD38-positive. CD1α, Langerin or HHV8 was negative, and gG4/IgG<1%. Moreover, elastic fiber staining can show the outline of residual blood vessels. No fungal or acid-fast bacillus infections were observed (Fig. 3). Finally, we diagnosed the patient with secondary syphilis with pulmonary involvement based on the immunostaining results and HIV and anti-tp testing.
Treatment and outcome
The patient received intramuscular benzathine benzylpenicillin (2.4 million units) once a week for 3 weeks.
Discussion and conclusions
Syphilis is a sexually transmitted disease that mostly occurs in the skin, mucosa, liver, bone marrow or testis. Syphilis can also cause systemic damage through blood circulation. In the late stage, cutaneous syphilis and neurosyphilis are common, while pulmonary syphilis is rare [5-8]. Moreover, there are few descriptions of the pathological morphology of pulmonary syphilis. In addition, HIV infection and syphilis have the same transmission mode, and the high-risk populations are similar [4]. Syphilis can increase the probability of HIV infection and the risk of transmission, while HIV can also affect the progression and response to treatment of syphilis at the same time. Moreover, it was reported that syphilis could stimulate the immune system, which leads to increased HIV replication and decreased CD4 counts [9, 10].
Symptoms of lung lesions associated with syphilis coinfection with HIV are variable, and imaging findings can be asymptomatic. In this report, lung lesions adjacent to the esophagus were well circumscribed and should be differentiated from lymphoma, esophageal or bronchial cysts and neurogenic tumors (such as schwannoma and neurofibroma) on imaging. Patients with pulmonary syphilis may have no respiratory symptoms or specific imaging manifestations, and tuberculosis, fungi and tumors should be excluded. Compared with other case of pulmonary syphilis [10], the histological features of this case were typical of chronic granulomatous inflammation with coagulative necrosis, plasma cell infiltration and endarteritis obliterans. However, plasma cell infiltration is relatively rare compared with classic gumma in the current case, which is considered to be caused by immunodeficiency caused by coinfection with HIV. Meanwhile, immunohistochemistry and special staining also supported the diagnosis of syphilis. Lung lesions associated with syphilis, especially coinfection with HIV, may be asymptomatic and still need to be differentiated from granulomatous lesions, such as tuberculosis, rheumatic granulomas, rheumatoid granuloma, typhoid granuloma, and vasculitic granulomatous disease. The constant plasma cell infiltration around coagulative necrosis and serologic findings support the diagnosis of syphilis.
A proportion of patients with HIV infection are asymptomatic syphilis infected. These patients are usually found with syphilis infection accidentally in routine physical examinations. There are also a certain number of AIDS patients complicated with secondary syphilis infection, and they have a high probability of neurological complications and poor prognosis. Clinically, the diagnostic criteria for pulmonary syphilis include the following: typical signs and symptoms, serological test positive for syphilis, pulmonary abnormalities on imaging examinations and response to anti-syphilis treatment. In this report, according to the patient’s medical history, laboratory findings and pathological features, we finally diagnosed pulmonary involvement of syphilis.
In summary, we report a case of secondary pulmonary syphilis with HIV coinfection. The imaging findings of this patient were atypical. If serological testing indicates syphilis infection, lung biopsy could be performed first to confirm the diagnosis along with appropriate treatment. In addition, HIV infection and syphilis promote each other and lead to diverse clinical symptoms, and clinicians should strengthen the ability to recognize the clinical characteristics and pathological changes in different stages of the disease.
Authors’ contributions
YL managed the case as well as redaction and correction of the manuscript. LL assisted with the clinical management of the case and correction of manuscript. LL, BD and YW assisted with manuscript correction and redaction of comments from the illustrations. All authors read and approved the final manuscript.
References
- Alison U, Zahraa A, Tina Dwivedi, Zana L, Justin CK. Syphilis in pregnancy: The impact of the Great Imitator. European journal of obstetrics, gynecology, and reproductive biology. 2021; 259: 207-10.
- Geremew H, Geremew D. Sero-prevalence of syphilis and associated factors among pregnant women in Ethiopia: a systematic review and meta-analysis. Syst Rev. 2021; 10(1) :223.
- Melody R, Thomas D, Sharon W. The Intersection of HIV and Syphilis: Update on the Key Considerations in Testing and Management. Current HIV/AIDS reports. 2021; 18(4): 280-8.
- Dhirendra G, Christopher J, Dharshnee C. Syphilitic Pulmonary Inflammatory Pseudotumor: A Diagnostic Challenge. International journal of surgical pathology. 2021; 29(1): 90-6.
- Goda K, Katsurada M, Doi T, Saga N, Maniwa Y, Kenzaka T. Pulmonary syphilis with a cicatricial variant of organizing pneumonia: a case report. BMC Pulm Med. 2023; 23(1): 170.
- Suttichai V, Nuntra S, Anucha A, Pansachee D. A case of secondary syphilis with pulmonary involvement and review of the literature. International journal of STD & AIDS. 2018; 29(10): 1027-32.
- Ohta A, Furusyo N, Kishihara Y, Eiraku K, Murata M, Kainuma M, et al. Secondary Syphilis with Pulmonary Involvement. Intern Med. 2018; 57(1): 121-6.
- Li NF, Ai PY, De FZ, Zi YW, Ping M. Consequences of HIV/Syphilis Co-Infection on HIV Viral Load and Immune Response to Antiretroviral Therapy. Infection and drug resistance. 2021; 14: 2851-62.
- Chan P, Tang THC, Kwong RTS, Chan L, Chan HSY, Lam KW, et al. Effects of syphilis infection among HIV-1-positive individuals on suppressive antiretroviral therapy. AIDS research and therapy. 2022; 19(1): 69.
- Se JK, Ju-Han L, Eung-Seok L, Il-Hwan K, Hyung JP, Chol S, et al. A case of secondary syphilis presenting as multiple pulmonary nodules. The Korean journal of internal medicine. 2013; 28(2): 231-5.

