Research Article - Volume 3 - Issue 5
Evaluation of treatment regimens of human brucellosis
Fatma Hammami*; Makram Koubaa*; Fatma Smaoui; Khaoula Rekik; Chakib Marrekchi; Mounir Ben Jemaa
Infectious Diseases Department, Hedi Chaker University Hospital, University of Sfax, Tunisia.
Received Date : Aug 24, 2023
Accepted Date : Sep 25, 2023
Published Date: Oct 04, 2023
Copyright: © Makram Koubaa and
Fatma Hammami 2023
*Corresponding Author : Makram Koubaa and Fatma Hammami, Infectious Diseases Department, Hedi Chaker University Hospital, University of Sfax, Tunisia.
Email: koubaa_makram@medecinesfax.org
DOI: Doi.org/10.55920/2771-019X/1559
Abstract
Background: Brucellosis, also known as « Mediterranean undulant fever », remains the most common zonoosis worldwide. Its myriad presentation and various symptoms explain the diagnostic delay. The cornerstone of treatment includes effective antibiotics for an adequate length of time which varies according to the clinical presentation and the associated complications. We aimed to evaluate treatment regimens of human brucellosis.
Materials and methods: We conducted a prospective study including all patients hospitalized in the infectious diseases department for brucellosis between 1992 and 2021. The diagnosis was confirmed by either isolation of Brucella bacteria from body fluids or the presence of positive titers (above 1/160) in Wright standard agglutination test.
Results: During the study period, we included 223 patients, among which 145 were males (65%). The mean age was 40±17 years. There were 106 cases of acute brucellosis (47.5%), 108 cases of sub-acute brucellosis (48.5%) and 9 cases of chronic brucellosis (4%). Among patients with acute or sub-acute brucellosis, the combination of DOX-RIF was significantly associated with a favorable evolution of the disease (OR=3.8 ; p=0.025), a lower risk of complications (OR= 0.2 ; p<0.001) and side effects (OR=0.1 ; p<0.001). Among patients with sub-acute brucellosis, treatment with the combination of DOX-RIF-cotrimoxazole was significantly associated with a lower risk of death (OR=0.3 ; p=0.038), while the combination of DOX-RIF-ciprofloxacin was significantly associated with a higher risk of relapse (OR=8 ; p=0.023). Treatment regimens based on triple-antibiotic therapy were significantly associated with a higher risk of complications (OR=3.7; p=0.016) and adverse effects (OR=4; p=0.034).
Conclusion: Brucellosis remains a public health problem. The disease evolution depend on the combination of antibiotics used. In addition to measures aimed to eradicate animal brucellosis, human prophylaxis is essential to avoid Brucella contamination pending effective human vaccination.
Keywords: Human brucellosis ; Doxycycline-rifampicin-cotrimoxazole ; Ciprofloxacin ; Disease evolution
Evaluation of treatment regimens of human brucellosis Background
Brucellosis, also known as “Mediterranean undulant fever”, remains the most common zonoosis worldwide [1]. It is caused by Gram-negative coccobacillus bacteria belonging to the genus Brucella which include 12 species [2]. Its myriad presentation and various symptoms explain the diagnostic delay and the evolution of the disease to the sub-acute cases of brucellosis with the occurrence of osteoarticular, cardiovascular and neurological complications [3]. In front of clinical suspicion of brucellosis, laboratory tests will confirm the diagnosis when indicating the presence of the organism or a specific immune response to its antigens [4, 5]. The cornerstone of treatment include effective antibiotics for an adequate length of time which varies according to the clinical presentation and the associated complications [4]. In this perspective, the aim of our work was to evaluate treatment regimens of human brucellosis.
Methods
Study design
We conducted a prospective study including all patients hospitalized in the infectious diseases department for brucellosis between 1992 and 2021.
Data collection and case definitions
Data were collected from the medical records of patients on pre-established sheets. We included all cases of brucellosis. We specified socio-demographic characteristics, including age, gender, and urbanity of residence. Previous medical history, the revealing symptoms, physical examination signs and laboratory investigations were recorded. Treatment regimens and the disease evolution were noted.
Clinical presentation of the disease included acute, sub-acute and chronic brucellosis. Acute brucellosis was defined by undulant or intermittent fever accompanied by malaise, anorexia and prostration. Sub-acute brucellosis was defined by the occurrence of complications including osteoarticular, cardiovascular, urogenital or neurological complications. Chronic brucellosis, also known as “chronic fatigue syndrome”, was defined by the long-term persistent fatigue or a fever, physical, psychological, sexual asthenia and general malaise or psychoneurosis. The diagnosis was suspected in front of clinical signs and symptoms suggestive of brucellosis, especially with a previous exposure to Brucella (consumption of unpasteurized dairy products or close contact with livestock). Its was confirmed by either isolation of Brucella bacteria from body fluids (blood, cerebrospinal fluid (CSF), abscess, joint fluid) or the presence of positive titers (above 1/160) in Wright standard agglutination test (SAT).
Statistical analysis
Statistical analysis was performed using the SPSS 20 software. Categorical variables were presented as numbers and percentages. Continuous variables were expressed as means and standard deviations (SD), if they were normally distributed. For non-normally distributed data, we used median and interquartile ranges. Chi square and Fisher exact test were used to compare two frequencies when applicable. The odds ratio was used to measure the association between an exposure and an outcome. The difference between the groups was considered significant when p<0.05.
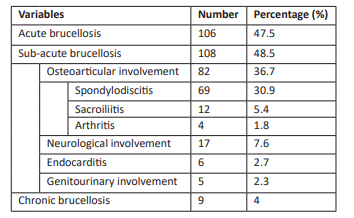
Table 1: Clinical presentations of cases of brucellosis.
Results
Patients’ characteristics
During the study period, we included 223 patients, among which 145 were males (65%). The mean age was 40±17 years. Rural origin was noted in 183 cases (82%). In total, 188 patients consumed unpasteurized dairy products (84.3%) and 160 patients had a close contact with livestock (71.7%). There were 106 cases of acute brucellosis (47.5%), 108 cases of sub-acute brucellosis (48.5%) and 9 cases of chronic brucellosis (4%) (Table 1). Patients consulted after a mean delay of 30[15-80] days. The revealing symptoms included fever (83.4%), night sweats (70.9%) and arthralgia (54.7%). Physical examination signs included fever (32.3%), spinal tenderness (26%) and splenomegaly (9.9%) (Table 2). Blood cultures, performed in 169 cases (75.7%), were positive for Brucella in 38 cases (22.5%). Cultures for CSF and abscess were positive for Brucella species in 29.4% and 36.3% of the cases, respectively. As for SAT, it was positive with a titer of ≥1/640 in 57 cases (25.6%), ≥1/1280 in 50 cases (22.5%), ≥1/320 in 43 cases (19.2%) and ≥1/2560 in 26 cases (11.7%). Treatment regimens varied according the clinical presentation and complications. Patients with acute brucellosis received oral doxycycline (DOX) 200 mg daily and oral rifampicin (RIF) 15 mg/kg daily in 100 cases (94.3%) for a mean duration of 45±23 days. Patients with sub-acute brucellosis received the combination of DOX and RIF
Table 2: Revealing symptoms and physical examination signs of patients with brucellosis.
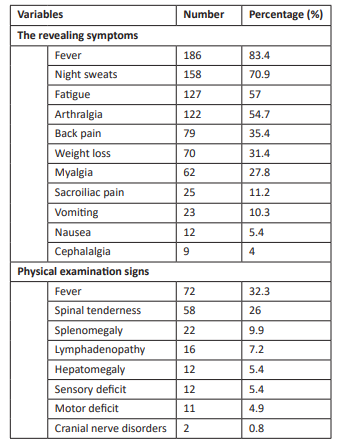
Table 3: The disease evolution of patients with brucellosis.
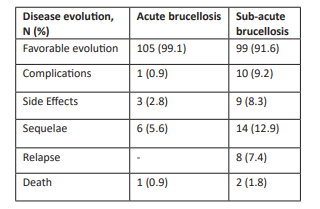
N : Number, %: Percentage
Table 4: Disease evolution of acute or sub-acute brucellosis cases treated with doxycycline and rifampicin.
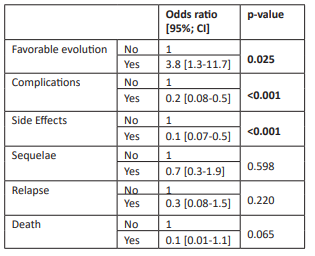
CI : Confidence interval
Table 5: Disease evolution of sub-acute brucellosis cases according to the treatment regimens prescribed.
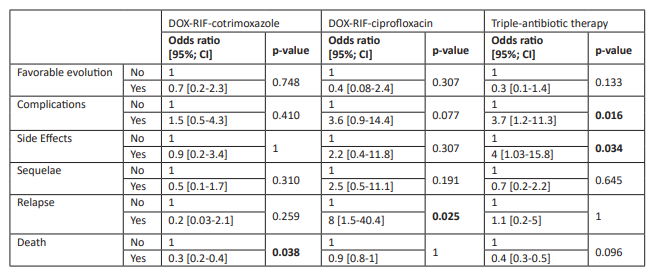
DOX : Doxycycline ; RIF : Rifampicin ; CI : Confidence interval
57 cases (52.7%), DOX-RIF-cotrimoxazole in 37 cases (34.2%) and DOX-RIF-ciprofloxacin in 10 cases (9.2%). Patients with chronic brucellosis received symptomatic treatment based on analgesics and nonsteroidal anti-inflammatory drugs with a favourable evolution of the disease in all cases.
Comparative analysis of treatment regimens
Among patients with acute or sub-acute brucellosis, the combination of DOX-RIF was significantly associated with a favorable evolution of the disease (OR=3.8 ; p=0.025), a lower risk of complications (OR= 0.2 ; p<0.001) and side effects (OR=0.1 ; p<0.001) (Table 4).
Among patients with sub-acute brucellosis, treatment with the combination of DOX-RIF-cotrimoxazole was significantly associated with a lower risk of death (OR=0.3 ; p=0.038), while the combination of DOX-RIF-ciprofloxacin was significantly associated with a higher risk of relapse (OR=8 ; p=0.023). Treatment regimens based on triple-antibiotic therapy were significantly associated with a higher risk of complications (OR=3.7; p=0.016) and adverse effects (OR=4; p=0.034) (Table 5).
Discussion
Our study highlighted the myriad presentations and various manifestations of brucellosis, upon which treatment regimens might differ. Among patients with acute or sub-acute brucellosis, the combination of DOX-RIF was significantly associated with a favorable evolution of the disease, a lower risk of complications and side effects. Among sub-acute brucellosis cases, the combination of DOX-RIF-cotrimoxazole was significantly associated with a lower risk of death, while the combination of DOX-RIF-ciprofloxacin was significantly associated with a higher risk of relapse.
Brucellosis is a multisystem disease that might affect any organ. The revealing symptoms included fever (87%), fatigue (63%), arthralgia (62%) sweats (55%) and vomiting (26%) [1], which was similar to our results. The absence of fever might be explained by the undulant type of fever or the administration of non-steroidal anti-inflammatory drugs or antipyretics. In front of clinical suspicion of brucellosis, laboratory investigations should be ordered. Bacterial isolation is the gold standard. The sensitivity of blood cultures is high during the acute phase of brucellosis, while it is usually low during the sub-acute phase. Blood cultures offer the benefit of confirming the diagnosis even at en early stage of the disease when the infection is not clinically suspected, since brucellosis is known as the « great imitator » [6]. In the absence of a positive culture, the diagnosis relies on serological tests [7]. Although it does not provide direct evidence of the presence of the microorganism, serological tests remain an indispensable diagnostic tool for human brucellosis, especially in countries of endemicity [6].
The main goal of treatment is to shorten the duration of symptoms and to prevent complications, relapse, chronicity and mortality [8]. It is based on the administration of effective antibiotics, which have activity in vitro against Brucella species, for an adequate length of time. Complicated cases might require the addition of surgical treatment or/and corticosteroids [4]. Treatment of acute cases of brucellosis is based on a dual therapy due to the high relapse rate with monotherapy. The World Health Organization recommended the association of oral DOX (100 mg twice a day) and oral RIF (600 to 900 mg daily) for 6 weeks since 1986 [9]. This regimen is still prescribed by the most infectious diseases specialists not only because DOX-RIF is an all-oral regimen, but also because of the low price and the availability of rifampicin in all countries including the developing ones [10]. Several regimens were proposed including the association of DOX for 6 weeks and aminoglycosides : gentamicin for 7 to 10 days or streptomycin for 2 or 3 weeks (48), the combination of quinolones and RIF for 6 weeks and the combination of cotrimaxazole and RIF (especially for children and pregnant women) for 6 weeks [11]. A previous systematic review and meta-analysis concluded that the regimen combining DOX and streptomycin were superior to combined DOX-RIF in terms of both relapse rate and treatment failure. Also, no significant difference was noted with combined DOX-gentamicin and combined DOX-streptomycin [12]. An other study reported that the combination of cotrimoxazole-RIF among children with brucellosis showed failure and relapse rate that was not significantly different from the combination of DOX-RIF [9]. To conclude, among patients with acute brucellosis, the association of DOX and aminoglycosides was the preferred treatment with the lower rate of relapse and treatment failure. In our study, none of our patients received this combination and 94.3% of patients with acute brucellosis received DOX-RIF with a favourable evolution of the disease in 99.1% of the cases.
Regimens prescribed for sub-acute brucellosis cases varies according to the associated complications. As for osteoarticular brucellosis, the combination of DOX-RIF or DOX-streptomycin were the most prescribed regimens. The DOX-streptomycin combination was more effective but less tolerated because of the intramuscular injections [13, 14]. Due to its high bone penetration, ciprofloxacin was prescribed in association with RIF, and compared to DOX-streptomycin. No significant difference concerning clinical response was noted, but the cost of ciprofloxacin plus RIF therapy was higher [15]. In our study, DOX-RIF-ciprofloxacin was significantly associated with a higher risk of relapse.
The treatment of neurobrucellosis is not yet consensual. However, recent studies have recommended a therapeutic regimen based on the combination of 3 or even 4 antibiotics which have good central nervous system penetration [16, 17]. Erdem et al studied the efficacy and tolerance of a triple therapy containing ceftriaxone. Three groups including the combination of DOX-RIF-ceftriaxone, DOX-RIF- cotrimoxazole and DOX-RIF-Ceftriaxone relayed by DOX-RIF-cotrimoxazole on discontinuation of ceftriaxone. This study had shown that treatment regimens containing ceftriaxone were more effective with less treatment failure and fewer relapses compared to the DOX-RIF-cotrimoxazole regimen [18]. None of our patients received ceftriaxone for neurobrucellosis. However, the disease evolution was favorable in 91.6% of the cases of sub-acute brucellosis. According to the European Society of Cardiology guidelines, treatment of brucellar endocarditis is based on a combination of DOX-RIF-cotrimaxazole for ≥3-6 months [19]. However, other regimens were prescribed such as DOX-RIF-ceftriaxone, DOX-RIF-streptomycin, DOX-RIF- cotrimoxazole et DOX-streptomycin-ceftriaxone. The mortality rate was lower in patients receiving streptomycin [20].
Conclusion
Brucellosis remains a public health problem. The disease evolution depend on the combination of antibiotics used. In addition to measures aimed to eradicate animal brucellosis, human prophylaxis is essential to avoid Brucella contamination pending effective human vaccination.
References
- Zheng R, Xie S, Lu X, Sun L, Zhou Y, Zhang Y, et al. A Systematic Review and Meta-Analysis of Epidemiology and Clinical Manifestations of Human Brucellosis in China. Biomed Res Int [Internet]. 2018 Apr 22 [cited 2022 Dec 30]; 2018. Available from: https://pubmed.ncbi.nlm.nih.gov/29850535/
- Nejad RB, Krecek RC, Khalaf OH, Hailat N, Arenas-Gamboa AM. Brucellosis in the Middle East: Current situation and a pathway forward. PLoS Negl Trop Dis [Internet]. 2020 May 1 [cited 2022 Dec 30]; 14(5): 1-17. Available from: /pmc/articles/PMC7241688/
- Dean AS, Crump L, Greter H, Hattendorf J, Schelling E, Zinsstag J. Clinical manifestations of human brucellosis: a systematic review and meta-analysis. PLoS Negl Trop Dis [Internet]. 2012 Dec [cited 2022 Dec 30]; 6(12). Available from: https://pubmed.ncbi.nlm.nih.gov/23236528/
- WHO. Brucellosis in humans and animals [Internet]. 2006 [cited 2022 Dec 30]. Available from: https://apps.who.int/iris/handle/10665/43597
- Wang W, Wang Z, Jia K, Tang J, Wang L. Clinical and Laboratory Characteristics of Childhood Brucellosis in High-Risk Area of Western China. Jpn J Infect Dis [Internet]. 2022 [cited 2023 Feb 3]; 75(2): 127-32. Available from: https://pubmed.ncbi.nlm.nih.gov/34470971/
- Yagupsky P, Morat P, Colmenero JD. Laboratory Diagnosis of Human Brucellosis. Clin Microbiol Rev [Internet]. 2019 Jan 1 [cited 2023 Jan 5];33(1). Available from: https://pubmed.ncbi.nlm.nih.gov/31722888/
- Shakir R. Brucellosis. J Neurol Sci [Internet]. 2021 Jan 15 [cited 2023 Jan 4]; 420. Available from: http://www.jns-journal.com/article/S0022510X2030616X/fulltext
- Bosilkovski M, Keramat F, Arapović J. The current therapeutical strategies in human brucellosis. Infection [Internet]. 2021 Oct 1 [cited 2023 Jan 5]; 49(5): 823-32. Available from: https://pubmed.ncbi.nlm.nih.gov/33650077/
- Alavi SM, Alavi L. Treatment of brucellosis: a systematic review of studies in recent twenty years. Casp J Intern Med [Internet]. 2013 [cited 2023 Jan 6]; 4(2): 636. Available from: /pmc/articles/PMC3755828/
- Ariza J, Bosilkovski M, Cascio A, Colmenero JD, Corbel MJ, Falagas ME, et al. Perspectives for the Treatment of Brucellosis in the 21st Century: The Ioannina Recommendations. PLOS Med [Internet]. 2007 Dec [cited 2023 Jan 6]; 4(12): e317. Available from: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0040317
- Yousefi‐Nooraie R, Mortaz‐Hejri S, Mehrani M, Sadeghipour P. Antibiotics for treating human brucellosis. Cochrane Database Syst Rev [Internet]. 2012 Oct 17 [cited 2023 Jan 6]; 2012(10). Available from: /pmc/articles/PMC6532606/
- Solís García del Pozo J, Solera J. Systematic review and meta-analysis of randomized clinical trials in the treatment of human brucellosis. PLoS One [Internet]. 2012 Feb 29 [cited 2023 Jan 6]; 7(2). Available from: https://pubmed.ncbi.nlm.nih.gov/22393379/
- Turgut M, Turgut AT, Koşar U. Spinal brucellosis: Turkish experience based on 452 cases published during the last century. Acta Neurochir (Wien) [Internet]. 2006 Oct 8 [cited 2023 Feb 3]; 148(10): 1033-44. Available from: https://link.springer.com/article/10.1007/s00701-006-0877-3
- Alp E, Doganay M. Current therapeutic strategy in spinal brucellosis. Int J Infect Dis [Internet]. 2008 Nov [cited 2023 Feb 3]; 12(6): 573-7. Available from: https://pubmed.ncbi.nlm.nih.gov/18539496/
- Alp E, Koc RK, Durak AC, Yildiz O, Aygen B, Sumerkan B, et al. Doxycycline plus streptomycin versus ciprofloxacin plus rifampicin in spinal brucellosis [ISRCTN31053647]. BMC Infect Dis [Internet]. 2006 Apr 11 [cited 2023 Feb 3]; 6. Available from: https://pubmed.ncbi.nlm.nih.gov/16606473/
- Nurgul Ceran, Recai Turkoglu, Ilknur Erdem, Asuman Inan, Derya Engin, Hulya Tireli PG. Neurobrucellosis: clinical, diagnostic, therapeutic features and outcome. Unusual clinical presentations in an endemic region - PubMed [Internet]. Braz J Infect Dis. 2011 [cited 2023 Feb 3]. Available from: https://pubmed.ncbi.nlm.nih.gov/21412590/
- Hasan Karsen, Suda Tekin Koruk, Fazilet Duygu, Kubilay Yapici MK. Review of 17 cases of neurobrucellosis: clinical manifestations, diagnosis, and management - PubMed [Internet]. Arch Iran Med. 2012 [cited 2023 Feb 3]. Available from: https://pubmed.ncbi.nlm.nih.gov/22827786/
- Erdem H, Ulu-Kilic A, Kilic S, Karahocagil M, Shehata G, Eren-Tulek N, et al. Efficacy and Tolerability of Antibiotic Combinations in Neurobrucellosis: Results of the Istanbul Study. Antimicrob Agents Chemother [Internet]. 2012 Mar [cited 2023 Feb 3]; 56(3): 1523. Available from: /pmc/articles/PMC3294949/
- Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F, et al. 2015 ESC Guidelines for the management of infective endocarditisThe Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J [Internet]. 2015 Nov 21 [cited 2023 Feb 3]; 36(44): 3075-128. Available from: https://academic.oup.com/eurheartj/article/36/44/3075/2293384
- Koruk ST, Erdem H, Koruk I, Erbay A, Tezer-Tekce Y, Erbay AR, et al. Management of Brucella endocarditis: results of the Gulhane study. Int J Antimicrob Agents [Internet]. 2012 Aug [cited 2023 Feb 3]; 40(2): 145-50. Available from: https://pubmed.ncbi.nlm.nih.gov/22727531/

