Mini Review - Volume 3 - Issue 5
Euthanasia and physician-assisted suicide: Most controversial issue in medical ethics; An overview
Abrar Hussain Azad1; Shaaray Abrar Umar2; Iram BiBi3
1Abrar Hussain Azad, Professor of Public Health Mohu din Islamic Medical College Mirpur AJK, Pakistan.
2Medical Officer Akbar Niazi Teaching Hospital Islamabad, Pakistan.
3Researcher Fatima Jinnah University for Women Rawalpindi, Pakistan.
Received Date : Sep 08, 2023
Accepted Date : Sep 27, 2023
Published Date: oct 06 2023
Copyright: © Shaaray Abrar Umar 2023
*Corresponding Author : Shaaray Abrar Umar, Medical Officer Akbar
Niazi Teaching Hospital Islamabad, Pakistan.
Email: drabrarumar@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1561
Abstract
Euthanasia and assisted killing are challenging issues being faced by medical sciences. It attracts moral, ethical and legal considerations. It is one of the most controversial issues in medical ethics. This article explores the concept and types of euthanasia and assisted killing. Article focuses on diversity in legality, attitudes and perceptions in practices regarding physician assisted suicide in different countries and cultures.
Keywords: Euthanasia;Physician assisted suicide;Legally, ethically.
Introduction
The root of the term euthanasia is Greek. It is derivative of two words “eu” and “thanatos” meaning “good death” or “easy death”. Another term used for this phenomenon is mercy killing. In other words to cause pain free death for a person who is otherwise suffering from a hopelessly incurable and agonizing disease is called euthanasia [1]. There are different sets of rights and wrongs associated with different forms of euthanasia. An illustration of active and passive euthanasia is as follows: There is yet another distinction called indirect euthanasia referred to as providing such treatment which usually reduces pain but its side effects accelerate the patient's death. Some
Table 1: An illustration of active and passive euthanasia.
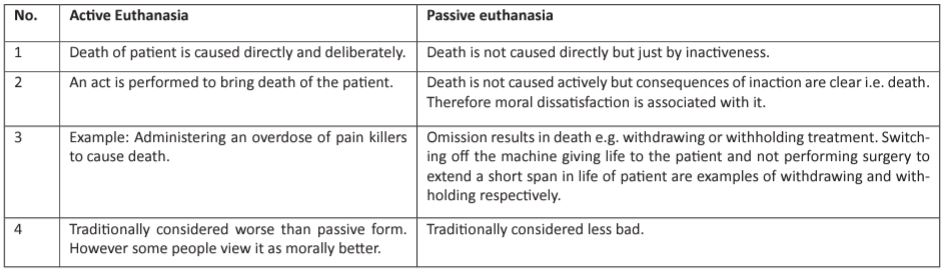
of the people, but not all consider it morally acceptable, as underlying intention is not to kill. Such moral justifications are formally called the doctrine of double effect [2]. In doctor assisted suicide, a person is provided with information, guidance and ways of ending his or her own life. In other words the patient is equipped with medical knowledge for enabling him/ her to take his/her own life. This knowledge pertains to painless and useful medical ways of committing suicide. If a doctor helps another person in killing him/herself this is referred to as physician assisted suicide [3].
Literature Review
Participation of physicians in assisted suicide or euthanasia has been denounced by the ethical guidelines of Norwegian Medical Association
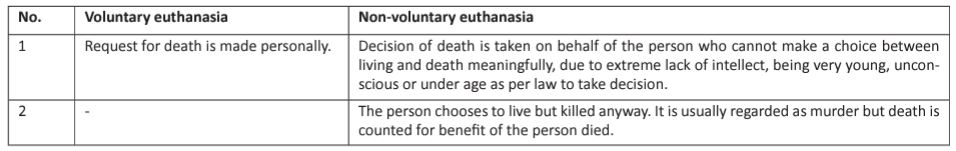
Table 2: Voluntary and non-voluntary is another division of euthanasia, which along with its moral considerations is explained as under.
However a Norwegian study to explore the attitudes of their physicians towards end life dilemma indicates that a considerable part of population is open minded in this regard. There was a sample of 1476 participants. Data was collected through postal questionnaires. 66% of the sample responded. The findings revealed broadly restrictive attitudes of physician towards euthanasia. The question regarding having an opportunity for actively ending the life of a patient with terminal illness and great pain, who also requests for it, was responded positively by 17% of the sample. However a question regarding chronic illness, accompanying pain and deteriorated quality of life of the patient and having a similar option was agreed upon by 4% of the sample, despite the fact that he may otherwise have several years to live. Certain actions aimed at accelerating the death process of the patient were performed by 6%. Treatment was provided at least once by 76% to the patients, for whom even they felt it should have been discontinued. A multiple logistic regression analysis indicated that medicine specialists, surgeons and psychiatrists significantly held more restive views as compared to laboratory specialties, physicians educated abroad and those with negative attitudes towards patient autonomy, who were more liberal in their views towards euthanasia [4]. Finding of a study suggests that assisted suicide is unethical. There are studies indicative of the fact that either depression or any other mental illness impairs the ability to judge in most of suicidal people. Prevalence of an actually “rational suicide” is rarer than the devastating majority of suicide. Assisted suicide can contribute to heighten suicide rate in general population, more specifically in younger people. The underlying factor in it would be de-stigmatization of suicide and contagion effect [5]. In a USA based survey, 1902 completed questionnaires (responded by 61%), it was found that 11% of the physicians were willing to hasten the death of a patient under certain circumstances by prescribing medications under existing legal constraints. 7% consented for administering a lethal injection. However 36% and 24 % respectively agreed for the same but at the condition of legality. A request for assisted suicide by the patient was received by 18.3 % of the physicians whereas request for lethal injection was received by 11.1 % .16% of the responding physicians who received such requests, 3.3 % of the whole sample, reported having written a prescription to be used to accelerate death at least once. 4.7% reported administering at least one lethal injection [6]. In the Netherlands the concept of euthanasia and physician assisted suicide although remained technically illegal but there has been increased openness in its practice. A nationwide study (1990-1991) was conducted on euthanasia and other life ending medical practices. It was commissioned by a governmental committee chaired by Professor Jan Remme, the attorney general of the Dutch Supreme Court. It gave a complete overview of the medical decisions in the country, related to ending life hence attracted much attention [7, 8]. There is a probability that increase in reported euthanasia cases from 486 in 1990 to 1466 in 1995 is attributive to introduction of a new reporting procedure of euthanasia and physician assisted suicide. To evaluate the new procedure an almost identical nationwide study (1995-1996) was conducted. It was commissioned by the ministers of health and justice. The purpose of 1995 study was; to have authentic estimation of the incidence of euthanasia and other life ending medical practices and changes in them from 1990 to 1995, and to describe the involved patients, physicians, and circumstances as well. Both studies revealed similar results regarding incidence pertaining to most of the practices. There was a 37% increase from 1990 in the requests for euthanasia at a later time in the course of disease, comprising 34,500. There was a 9 percent increase from 1990 in explicit requests for euthanasia or physician assisted suicide at a particular time, comprising 9700. 2.3% and 2.4% of all deaths resulted from euthanasia, found in the interview and death certificate study respectively. However these rates were 1.9% and 1.7% respectively in 1990. Instance of assisted suicide was 0.4% and 0.2% of all deaths in the interview and death-certificate study respectively, whereas it was 0.3% and 0.2 % respectively, in 1990. There were 0.7% of deaths which involved ending the patient’s life without his explicit, concurrent request, as reported in both 1995 studies. However 0.8% of deaths in the death-certificate study were reported to occur in this way in 1990 [9, 10]. Physician assisted suicide was legalized for the first time in Oregon State in November, 1994, when ballot initiative, the Oregon Death with Dignity Act was approved by voters [11]. A Federal district judge ruled the measure unconstitutional in August 1995 [12]. A survey was conducted in Oregon. Its sample was physicians, eligible for prescribing a lethal medicine under the new law of the State. Objectives of the survey were to describe association between personal and professional characteristics and particular attitudes towards physician assisted suicide, existing practices for caring the patients with terminal illness, including assessment of responses to assisted suicide requests and contact with other health care professionals and issues of concern pertaining to implementation of Oregon Death with Dignity Act. 70% of the sample responded to the questionnaire of the survey. It was thought by 60% of the respondents that in certain cases physician assisted suicide should be legal. In case of being legal, 46% might be willing to prescribe a lethal dose of medication. Unwillingness was shown by 31% in doing so on moral grounds. Requests for assisted suicide were received by 21% of respondents among whom 7% complied with. Half of the respondents were not certain about prescribing what in this regard. 83 % attributed financial constraints as a possible factor for requesting as such. The respondents had concerns regarding complications of suicide attempts and their own ability in predicting survival at six months accurately [13]. In a study (1995-1996), 405 Dutch physicians were interviewed who were selected randomly nationwide and were stratified by specialty and region. Structured questionnaire was used for interviewing. The interview was conducted by 30 experienced and trained physicians. It was responded by 89% of the sample. In response to patient’s explicit request for ending his life, administration of drugs with the intention to do so was referred to as Euthanasia. However prescription or supply of drugs with explicit intention to equip the patient to end his/her own life was called as assisted suicide. 134 physicians had a most recent case of granted request, whereas 148 physicians had their most recent case of a refused request. Those whose requests were refused included; female patients over the age of 80, patients having less chances of cancer, predominant depression patients, patients with probability of having a life span of more than 6 months, those whose requests were less explicit and those who were suffering less severely and had an access to alternative forms of treatment. In both the refused and the granted requests “avoiding loss of dignity” 42% (95% confidence interval 31.6% to 52.4%) and 56% (46.3% to 66.2%) respectively and “unbearable or hopeless suffering” 39% (29.0% to 48.8%) and 74% (64.9% to 82.6%) were mentioned as the patient's reason for requesting euthanasia or physician assisted suicide mostly. Only two reasons were mentioned more often in refused requests than in granted requests; “weariness of life” 40% (29.8% to 50.5%) and 18% (10.2% to 25.5%) respectively and “not wanting to become a burden on the family” 23% (14% to 32.3%) v 13% (5.8% to 19.2%)). The reasons most often given by physicians for refusal of the request were “suffering was not unbearable” (35%); “still alternatives for treatment” (32%); “the patient was depressed or had psychiatric symptoms” (31%); and “the request was not well considered” (19%) [14]. Assistance in dying by physician is also legally regulated in other countries. The Oregon Death with Dignity Act was enacted into law in 1997 to legalize physician-assisted suicide. In 2002 Belgium adopted a law largely similar to the Dutch law on euthanasia [15, 16]. As regards large-scale research to ascertain insight into the practices of euthanasia/assisted suicide and their utilization in end of life decision making, the Netherlands is the 1st country. Data regarding frequency and characteristics of euthanasia, physician assisted suicide and other medical acts for accelerating death process has been provided by large scale nationwide studies of 1990, 1995 and 2001 [17, 18, 19]. The importance of decision making regarding end-of-life in current medical practice has been proved in these studies. They have influenced national policy making for end-of-life care. In 2005, a follow-up study was conducted to evaluate the effects of the 2002 Dutch law and changes in end-of-life care. The reporting rates for euthanasia, assisted suicide and reasons for non-reporting as explained by the physicians need to be further assessed.
Conclusion
A clear cut controversy exists globally regarding the issue. The issue demands legal, moral, ethical and religious discussions. As the Hippocratic Oath does favor the opponents of euthanasia and assisted killing, others are in favor of modification in medical ethics advocating these practices. Autonomy of the patient is defined in different ways by both entities. One point of view being patient has a right to die and others argue that no one has right to take away the life of an individual not even individual him or herself. After decades of conflict resolution is still awaited.
References
- Reddy KSN. The essentials of Forensic medicine & Toxicology, 26th edition. 2007; 41.
- http://www.bbc.co.uk/ethics/euthanasia/overview/forms.shtml retrieved on 23-04-2015
- VijKrishan, The Textbook of Forensic Medicine& Toxicology, 4th edi. 2008; 488-490.
- Førde R, Falkum E, Aasland OG. The ethics of euthanasia Attitudes and practice among Norwegian physicians. Social Science & Medicine. 1997: 45(6) : 887-892.
- Callahan J. The Ethics of Assisted Suicide 1993; 19(4):237-244
- Meier D E, Emmons CA, Wallenstine S. A national survey of physician assisted suicide and euthanadisa in the United States Of America. The New England Journal of Medicine. 1998; 338(17).
- Van der Maas PJ, van Delden JJM, Pijnenborg L, Looman CWN. Euthanasia and other medical decisions concerning the end of life. Lancet. 1991; 338: 669-74.
- Van der Maas PJ, van Delden JJM, Pijnenborg L. Euthanasia and other medical decisions concerning the end of life. Health Policy. 1992; 22(1/2).
- Van der Wal G, Dillmann RJM. Euthanasia in the Netherlands. BMJ. 1994; 308: 1346-9.
- van der Wal G, van der Maas PJ, Bosma JM, et al. Evaluation of the notification procedure for physician-assisted death in the Netherlands. N Engl J Med. 1996; 335: 1706-11.
- Ballot measure 16. In: Oregon voters’ pamphlet. Portland, Oreg: Multnomah County Elections Division. 1994.
- Lee et al. v. State of Oregon, et al. U.S. District Court, Oregon, August 3, 1995. (No. 94-6467-HO)
- Melinda A, Lee, Heidi D. Legalising assisted suicide –views of phycians in Oregon. The new England journal of Medicine. 1996; 334(5): 310-315.
- Haverkate I, Onwuteaka-Philipsen BD, van der HeideA, Kostense PJ, van der Wal G, van der Maas PJ. Refused and granted requests for euthanasia and assisted suicide in the Netherlands: interview study with structured questionnaire. BMJ. 2000; 321: 865/66. (Full text: http://bmj.com/cgi/content/full/321/7265/865, accessed 24 January 2003)
- 15-Ganzini L, Nelson HD, Schmidt TA, Kraemer DF, Delorit MA, Lee MA. Physicians' experiences with the Oregon Death with Dignity Act. N Engl J Med. 2000; 342: 557-563. [Erratum, N Engl J Med. 2000; 342: 1538.
- Deliens L, Mortier F, Bilsen J, et al. End-of-life decisions in medical practice in Flanders, Belgium: a nationwide survey. Lancet. 2000; 356: 1806-1811.
- Van der Maas PJ, Van Delden JJM, Pijnenborg L, Looman CWN. Euthanasia and other medical decisions concerning the end of life. Lancet. 1991; 338: 669-674.
- Onwuteaka-Philipsen BD, van der Heide A, Koper D, et al. Euthanasia and other end-of-life decisions in the Netherlands in 1990, 1995, and 2001. Lancet. 2003; 362: 395-399.
- Van der Maas PJ, van der Wal G, Haverkate I, et al. Euthanasia, physician-assisted suicide, and other medical practices involving the end of life in the Netherlands, 1990-1995. N Engl J Med. 1996; 335: 1699-1705.

