Case Report - Volume 3 - Issue 5
Fetal MRI revealing a rare jejuno-ileal atresia: Apple peel intestinal atresia
Mribat M*; Izi Z; El Adioui G; El Haddad S; Allali N; Chat L
Pediatric teaching hospital, radiology department, Mohammed V University, Rabat, Morocco.
Received Date : Aug 28, 2023
Accepted Date : Sep 29, 2023
Published Date: Oct 10, 2023
Copyright: © Mribat Merieme 2023
*Corresponding Author : Mribat Merieme, Radiology Department, Mohammed V hospital, Mohammed V university Rabat, Morocco.
Email: meriememribat@gmail.com
DOI: Doi.org/10.55920/2771-019X/1563
Abstract
Apple peel intestinal atresia is a rare congenital malformation. Prenatal diagnosis can be done with obstetric ultrasound and confirmed by Fetal magnetic resonance imaging. We report a case of jejuno- ileal atresia (JIA) diagnosed during obstetric ultrasound showed small bowel dilation associated with hydramnios. Neonatal abdominal x-ray of the newborn confirmed the signs of intestinal occlusion. The aim of our work is to make a focus on this uncommon neonatal condition as well as the benefits of the antenatal diagnosis for adequate and timely management.
Keywords: Apple peel atresia, Congenital obstruction, Ileal atresia, Intestinal obstruction, Resection Abbreviation: JIA: jejuno- illeal atresia; MRI: magnetic resonance imaging; US: ultrasound
Introduction
Apple peel atresia is the rare form of atresia with an incidence of 0.7-0.8% in 10,000 live births accounting to 5-10 % of all intestinal atresias [1]. Premature newborns have a higher risk of developing atresia. It is formed up of a distal small bowel that spirals around its vascular supply strongly resembling an apple peel and a proximal jejunum that ends in a blind pouch. They hypothesized that jejunal and ileal atresia occur due to an intrauterine vascular assault due to placental vascular anomalies [1, 2]. We present a report of fetal MRI findings in JIA with corroborative postnatal radiologic and surgical examination.
Case report
A 27-year-old gravid woman without a significant medical history or personal history of substance abuse, was admitted to our hospital at 30 weeks’ gestation for the evaluation of polyhydramnios and bowel dilatation based on an outside US study (Figure 1). A fetal MRI was then performed at our institution to further characterize the bowel abnormalities and evaluate for any associated anomalies. It showed dilated loops of bowel throughout the fetal abdomen with polyhydramnios (Figure 2). The pregnancy progressed without complication, and a vaginal delivery was induced at 37 weeks. At birth the general physical examination concluded an alert baby, active and with good hydration. Abdomen was soft, distended and non tender. Anus was patent and the rectum was empty on digital rectal examination. In the evaluation of other systems, no notable findings were discovered. X-ray abdomen showed dilated stomach and small bowel loops with no rectal gas shadow (Figure 3A). A laparotomy was scheduled given that jejunal atresia was suspected. After stabilizing the patient, an exploratory laparotomy was carried out by transverse subumbilical mini-laparotomy approach which revealed type IIIb intestinal atresia with a substantially dilated distal duodenum and proximal jejunal atresia, with distal small intestine twisted on its axis giving an apple peel or pigtail-like aspect without necrosis (Figure 3B).
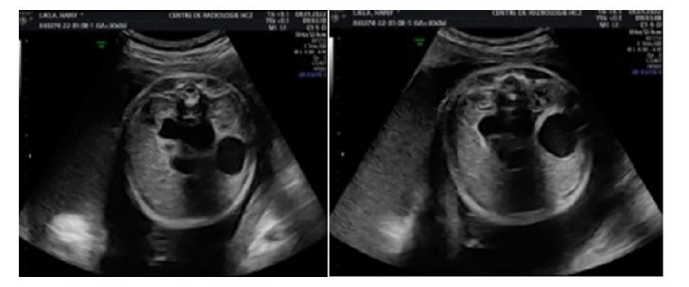
Figure 1: Fetal ultrasound of a 30-week-old female fetus with double cystic bubble suggesting intestinal atresia.
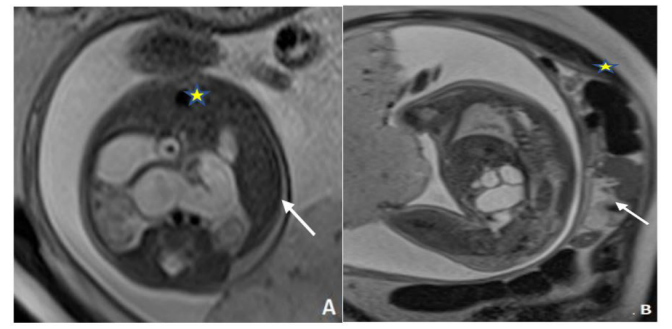
Figure 2: axial (A) and sagittal (B) Fast spin-echo T2 weighted magnetic resonance imaging of a 30-week-old female fetus with polyhydramnios (yellow stars) and double bubble sign (white).
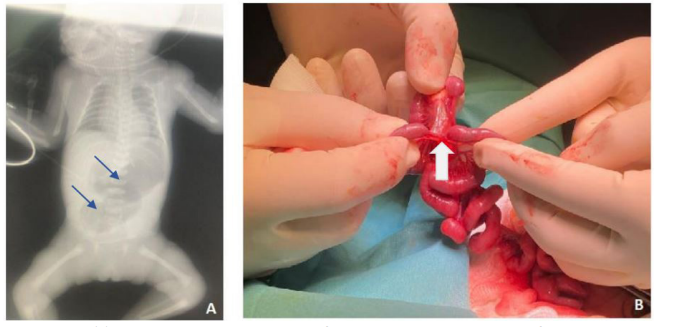
Figure 3: Post-natal: (A) X-ray Thoraco-abdominal shows an air-fluid level in the stomach, one more air-fluid level is evident to the right of the stomach. (B) Exploratory laparotomy showing the mesenteric defect (White arrow).
Discussion
Isolated apple peel atresia is extremely unusual and has a poor prognosis with mortality rate much higher than simple duodenal or jejunal atresia because of deficient collateral circulation to the small intestine. All gastrointestinal atresias often manifest earlier in life or at birth with signs of bowel obstruction. Such newborns presented with bilious vomiting, abdominal distention, inability to pass meconium, evident intestinal peristalisis, and respiratory distress as a result of significant abdominal distention. The identification of bowel obstruction by obstetric ultrasound varies according to the location of the lesion: 52% duodenal, 40% jejunal-ileal, and 29% bowel [3]. The pathognomonic "double bulla" sign and polyhydramnios in the 3 ed trimester are the best reported markers suggesting the JIA but they are not highly specific or sensitive. The prenatal detection of these congenital abnormalities has a significant impact on the post-natal management, it may influence the mode of delivery and the transfer to pediatric surgical services which can minimize the long-term effects of the anomaly [4]. Although, US continues to be the preferred method of screening for fetal anomalies, in recent years MRI has become an important tool in fetal diagnostics. It provided more accurate finding, it usually shows dilated loops of bowel fluid like throughout the fetal abdomen with a markedly distended stomach and polyhydramnios.
Postnatal diagnosis of intestinal atresias, including JIA, can be established using an X-ray and US scan. Due to the presence of air, the X-ray could reveal enlarged bowel. In addition to detecting atresias, the US scan can offer useful information on stomach movements [5] Intestinal atresias are classified by Grosfeld modified Low classification [6]:
- Type 1: has mucosal atresia,
- Type 2: connected by fibrous bands,
- Type 3: two separate bands with mesenteric defect, 3(a) only defect 3(b) apple peel atresia,
- Type 4: multiple atresia with mesenteric defects The present case is a type of apple peel atresia or Christmas tree atresia or pigtail-like syndrome. They are characterized by bowel occlusion, a mesenteric defect, and the encircling of minuscule bowel loops within an isolated vascular pedicle [7]. The outcome of isolated apple peel atresia is poor, with a complication incidence of 63% and a mortality rate of 54% [8]. After establishing the diagnosis, surgery is the recommended method of treating JIA. The initial step is to explore the abdominal cavity to confirm the diagnosis and exclude out further atresias or gastrointestinal abnormalities (intestinal malrotation and duplication) and the therapeutic objective is to conserve as much bowel as possible. The surgical treatment consists of excision of the dilated end of the bowel and anastomosis with the distal end [9]. Surgical examinations for our patient revealed no intestinal malrotation, duplication, or simultaneous atresia; a jejunal excision was performed with anastomosis. Conclusion Isolated apple peel atresia is extremely rare with poor prognosis, however, prenatal diagnosis of the condition and surgery for the newborn would reduce postsurgical morbidity while offering almost normal quality of life.
References
- Altokhais TI. Duodenal atresia with apple-peel jujenoilial deformity: Case report and review of the literature J Ped Surg Case Reports. 2014; 2: 156-8.
- Louw JH, Barnard CN: Congenital intestinal atresia observations on its origin. Lancet. 1955; 266: 1065-1067. 10.1016/S0140-6736(55)92852-X.
- John R, D’Antonio F, Khalil A, et al. Diagnostic accuracy of prenatal ultrasound in identifying jejunal and ileal atresia. Fetal Diagn Ther. 2015; 38:142-146.
- Virgone C, D’antonio F, Khalil A, Jonh R, Manzoli L. Accuracy of prenatal ultrasound in detecting jejunal and ileal atresia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015; 45: 523-529.
- Rich BS, Bott M, Spigland N: Multiple intestinal atresia with apple peel syndrome successfully treated with primary repair. J Pediatr Surg Case Rep. 2013; 1: 157-159. 10.1016/j.epsc.2013.05.015.
- Grosfeld JL, Ballantine TV, Shoemaker R: Operative management of intestinal atresia and stenosis based on pathologic findings. J Pediatr Surg. 1979; 14: 368-375. 10.1016/S0022-3468(79)80502-3
- Sahu S, Dhavala S S. Apple-peel syndrome" a case of malrotation with atresia of proximal small bowel. Indian J Radiol Imaging. 2006; 16: 189-90.
- Alnosair AA, Naga MI, Abdulla MR, Al-Salem AH. Congenital duodenal atresia with ‘apple-peel configuration’ of the small intestines and absent superior mesenteric artery: A case report and review of literature. J Ped Surg Case Reports. 2014 ;2: 215- 8.
- Lee SH, Cho YH, Kim HY, Park JH, Byun SY: Clinical experience of complex jejunal atresia. Pediatr Surg Int. 2012; 28: 1079-1083. 10.1007/s00383-012-3131-5

