Case Report - Volume 3 - Issue 5
Sudden onset unilateral proptosis in a 10-year-old female: Unique case of orbital vein varix management and treatment using bleomycin
Maria Rizk; Nahia Jalbout; Raghid Kikano; Roland Seif; Ama Sadaka
Department of Ophthalmology, Lebanese American University Medical Center-Rizk Hospital, Beirut, Lebanon
Received Date : Sep 29, 2023
Accepted Date : Oct 18, 2023
Published Date: Oct 25, 2023
Copyright:© Maria Rizk 2023
*Corresponding Author : Maria Rizk, Lebanese American University Medical Center - Rizk Hospital, Zahar Street, Beirut, Lebanon.
Email: Maria.rizk@laumcrh.com
DOI: Doi.org/10.55920/2771-019X/1573
Abstract
Keywords: Orbital varix, bleomycin, orbital varices thrombosis
Introduction
This report adhered to the ethical principles outlined in the Declaration of Helsinki as amended in 2013.
Orbital varices are venous malformations of the orbit caused by vascular dysgenesis. It is a rare condition, accounting for 0-1.3% of all histopathologically proven orbital masses [1]. They are usually diagnosed between the ages of 10-30 years. Most cases occur unilaterally. They most commonly involve the superior ophthalmic vein. Symptoms include intermittent proptosis associated with Valsalva maneuver. Complications include thrombosis of the varices, orbital hemorrhage, and decreased vision due to optic nerve compression [2]. To date there has been no definite standardization of treatment for orbital varices. Small lesions do not usually require treatment. However, recurrent thrombosis, severe proptosis, pain, or optic nerve compression are indications for intervention since they carry risks of vision loss. In this case report, we present a unique case of a previously healthy 7-year-old girl who presented with thrombosed left orbital venous varices and proptosis that did not resolve with time and needed intervention. Keywords: Orbital varix, bleomycin, orbital varices thrombosis
Case presentation
7-year-old girl previously healthy with intermittent reversible episodes of proptosis of the left eye (OS) years ago on Valsalva maneuvers. She was diagnosed with left orbital varices and was followed up in another ophthalmology center with regular exams without any intervention. On the day of presentation, the patient presented with acute and painful left eye proptosis, that unlike other episodes in the past, did not resolve spontaneously. On ophthalmic exam, best-corrected visual acuity was 20/20 in both eyes. Pupils were equal, reactive, and there was no relative afferent pupillary defect (RAPD). Intraocular pressures (IOP) were 18 in both eyes (OU). Anterior segment exam showed extensive chemosis and proptosis OS. Fundus exam was normal OU. She was admitted and MRI of the orbits (Orbital MRI protocol without and with IV contrast, MRI 3T GE Discovery 750) showed an extraconal orbital serpentine oblong structure, showing central clotting, with blood products in keeping with left thrombosed orbital varix (Figure 1A). The diagnosis was further confirmed by a brain and orbital diagnostic cerebral angiogram (DSA), with arterial and venous timing, and 3D post processing obtained on a separate workstation and sent for analysis (Siemens ArtisQ Biplane). The diagnostic imaging features on the MRI, and DSA angiogram showed no sign of abnormal arterial feeder or early venous drainage suggesting the absence of an arteriovenous fistula or arteriovenous malformation. The patient did not show any spontaneous improvement or worsening over the next three days after admission. Proptosis and pain were significant so decision was made to intervene. After reviewing the literature and discussing with the interventional radiology department, decision was made for a percutaneous intervention and sclerotherapy of the thrombosed varices, using direct puncture and injection of liquid sclerosing mixture of Bleomycin. Using ultrasound and fluoroscopy guidance, access was obtained into the thrombosed varix, through a transcaruncular approach, using a 25G needle. Aspiration was not able to drain significant fluid or venous blood. A mixture of bleomycin and Sotradecol Sodium Tetradecyl Sulfate (SSTS 3% sclerosing agent) was mixed into a foam solution and injected into the varix, under real time fluoroscopy demonstrating the sclerosing solution filling and stagnating within the thrombosed venous varix (Figure 1B), confirmed with a DynaCT scan obtained directly at the time of the procedure. A canthotomy and cantholysis was also performed at that moment to release some of the intra-orbital pressure. Patient did well after the procedure. Subsequent control CT-Scan, showed an interval decrease in the size of the thrombosed varix in the left orbit, with hyperattenuation of the center of the varix, consistent with sclerosing agent diffusing and filling the thrombus. The patient was monitored over time and showed progressive improvement of her symptoms consistent with control radiology imaging. She remains stable two years after follow up, with no recurrence, no side effects, and 20/20 vision (Figure 2A-2B).
Discussion
Modalities of treatment of orbital varices described in the literature are scarce because the disease itself is rare. Described techniques include surgical excision, endovascular embolization, percutaneous N-butyl cyanoacrylate glue embolization, percutaneous alcohol sclerotherapy, carbon dioxide laser surgery, and intralesional bleomycin.(1,3) A few reports describe the use of bleomycin in orbital varices so this case report comes to add further data on the efficacy of this agent in the management of these lesions [2, 4]. Bleomycin causes DNA breaks, induction of tumor necrosis factor, and apoptosis in rapidly dividing cells leading to endothelial damage and fibrosis. It acts on the endothelial lining of a lesion and therefore volume of the lesion is the major determinant in response. It is important to understand that intralesional bleomycin shrinks the lesion and does not remove it like surgery would. This case report proves that it is a safe treatment modality, if done properly, especially that surgical management of these cases is challenging and can cause uncontrollable bleeding. The other agents used in literature are either very expensive, or dangerous to ocular structures if extravasation occurs (alcohol, ethanol) [2, 4]. Also, we performed this procedure transcutaneously although it was a deep orbital lesion that is usually treated by orbitotomy [4]. Knowing that treatment modalities other than primary surgical intervention exist is important for patient safety. Sclerotherapy with Bleomycin can also act as a preparation step to facilitate future surgical excision if still needed. This report will hopefully help other physicians make a decision when confronted with this rare disease in order to safely help patients.
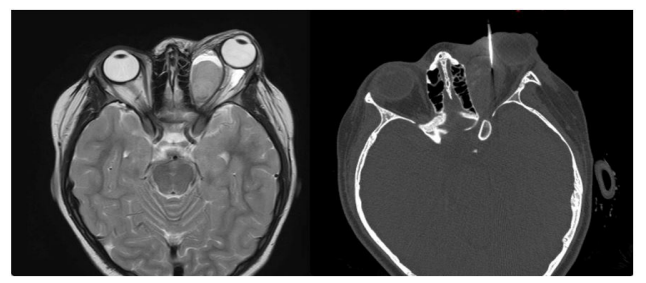
Figure 1: A- MRI orbits showing the left thrombosed venous varix in the medial left orbit.B- CT scan orbits at the time of the procedure with the Bleomycin being injected inside the lesion using a 25G needle.
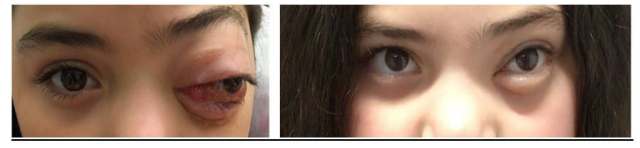
Figure 2: A- Left eye proptosis and chemosis.B- Appearacne of the left eye at last follow up 2 years after intervention.
References
- Vadlamudi V, Gemmete JJ, Chaudhary N, Pandey AS, Kahana A. Transvenous sclerotherapy of a large symptomatic orbital venous varix using a microcatheter balloon and bleomycin. 2015; 1-3.
- Yue H, Qian J, Elner VM, Guo J, Yuan YF, Zhang R, et al. Treatment of orbital vascular malformations with intralesional injection of pingyangmycin. Br J Ophthalmol [Internet]. 2013; 97(6): 739-45. Available from: https://pubmed.ncbi.nlm.nih.gov/23603483/
- Tsai ASH, Fong KS, Lim W, Al Jajeh I, Chuah CT, Rootman J. Bilateral orbital varices: An approach to management. Ophthal Plast Reconstr Surg [Internet]. 2008; 24(6): 486-8. Available from: https://pubmed.ncbi.nlm.nih.gov/19033851/
- Jia R, Xu S, Huang X, Song X, Pan H, Zhang L, et al. Pingyangmycin as first-line treatment for low-flow orbital or periorbital venous malformations: Evaluation of 33 consecutive patients. JAMA Ophthalmol [Internet]. 2014; 132(8): 942-8. Available from: https://jamanetwork.com/journals/jamaophthalmology/ fullarticle/1859727

