Case Report - Volume 3 - Issue 5
Comparison of clinical, functional, histologic and proteinuric parameters in the functional outcomes remission and ESRD in 170 patients with Glomerulonephritis (GN) and Nephrotic Syndrome (NS) and 190 patients with GN and Persistent Non-Nephrotic Proteinuria (PP)
Claudio Bazzi*
Retired from Nephrology and Dialysis Unit, San Carlo Borromeo Hospital, Via Pio II, 3, Milan, Italy
Received Date : Sep 30, 2023
Accepted Date : Oct 20, 2023
Published Date: Oct 27, 2023
Copyright:© Claudio Bazzi 2023
*Corresponding Author : Claudio Bazzi, MD, Via Ripa di Porta Ticinese,
71, 20143 Milan, Italy.
Email: "claudio.bazzi@alice.it"
DOI: Doi.org/10.55920/2771-019X/1574
Abstract
Background: The first aim of this study is to compare the clinical, functional. histologic and proteinuric parameters of patients with Remission or ESRD in 170 patients with glomerulonephritis (GN) and Nephrotic Syndrome (NS) and 190 GN patients with persistent non-nephrotic proteinuria (PP).
Methods: The parameters considered were: age, percentage of high blood pressure, baseline and last eGFR, baseline and last 24 hours proteinuria, percentage of global glomerular sclerosis (GGS%). Tubule-interstitial damage (TID) and Arteriolar Hyalinosis (AH) evaluated by a score; total urinary proteins, urinary IgG, α2macroglobulin (α2m), Albumin and α1microglobulin (α1m) were expressed per gram of urinary creatinine.
Results: Among the 170 patients with GN & NS 92 patients (54%) entered Remission and 38 (22%) progressed to ESRD. The patients with Remission shows lower percentage of high BP (52 vs 85%), higher values of baseline eGFR, lower values of TID and AH score, and lower values of all proteinuric parameters of last 24 h P. In 190 patients with GN and PP 129 patients entered Remission (68%) and 18 patients progressed to ESRD (9%). The patients with Remission in comparison with 18 patients progressing to ESRD show lower percentage of high BP (28% vs 94%), higher values of baseline eGFR, lower values of GGS%, TID score and AH score and lower values of all proteinuric parameters.
Conclusions: The patients with GN&NS and those with GN&PP are characterized by clinical outcomes Remission and ESRD significantly different for all the clinical, functional, histologic and proteinuric parameters.
Introduction
The etiopathogenesis of glomerulonephritis is not completely known and several different factors have been suggested as responsible of development of various types of glomerulonephritis (GN). Glomerulonephritis is a renal disease in which immune-mediated glomerular damage is the initiating factor. The hallmark of glomerulonephritis is increased permeability of the glomerular barrier. Proliferative glomerulonephritis is characterized by proliferation of the mesangial cells with influx of inflammatory cells. Membranous glomerulonephritis is characterized by accumulation of matrix and thickening of the glomerular basement membrane (GBM) and capillary wall. The patients with GN&NS and GN&PP are different for Remission and ESRD. The objective of my article is to compare the clinical, functional, histologic and proteinuric parameters in patients with functional outcomes (Remission and ESRD) in 170 patients with GN and NS and 190 patients with GN and PP; the functional outcome of these patients was assessed after a rather long follow up: 87±74 months in NS patients and 63±38 months in PP patients.
Patients
Between 1969 and 2006 469 patients were diagnosed by renal biopsy as glomerulonephritis in the Nephrology and Dialysis Unit of San Carlo Borromeo Hospital in Milan, Italy. 360 of these patients were followed over time and their functional outcome was assessed: 170 patients have glomerulonephritis (GN) and nephrotic syndrome (NS) and 190 patients have GN & Persistent non-nephrotic proteinuria (PP). Among the 170 patients with GN & NS n. 92 (54.1%) entered in Remission and 39 progressed to ESRD (38%). The patients with GN & NS entering Remission are significantly different from patients GN & NS progressing to ESRD (Table 2); the Remission patients show higher baseline and last eGFR (<0.0001) and significantly lower values of all histologic and proteinuric parameters. The patients with GN & NS progressing to ESRD show lower values of baseline and last eGFR and significantly higher values of GGS% (0.0016), TID score (0.00048), AH score (0.0001), TUP/C (<0.0001), IgG/C (0.0016), α2m/C (0.001), Alb/C (0.0001), α1m/C (0.0001) and last 24 hours proteinuria (<0.0001). The patients with GN and PP and ESRD show lower values of baseline and last eGFR and higher values of all histologic and proteinuric parameters (Table 5).
Table 1:
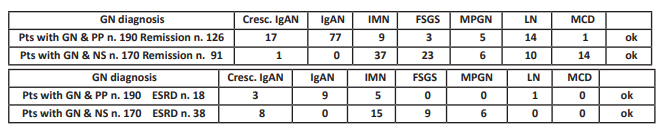
Table 2: Functional outcome of 170 patients with glomerulonephritis (GN) and nephrotic syndrome (NS).
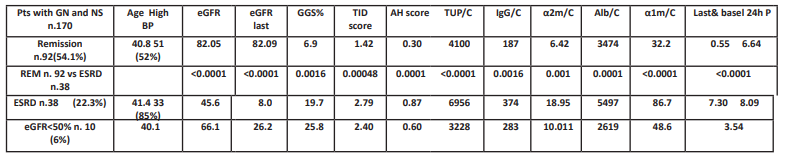
Table 3: Functional outcome of 190 patients with GN and PP.
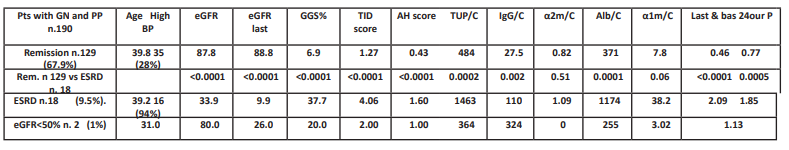
Table 4: Comparison between 123 remission patients with GN&PP and 100 remission patients with GN&NS.
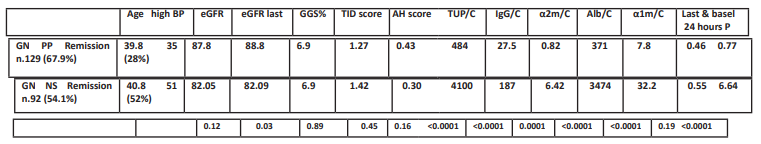
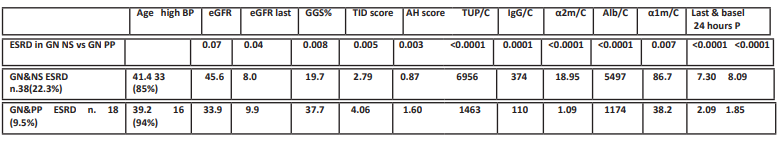
Table 5: Comparison between 38 patients with GN&NS and ESRD and 18 patients with GN&PP and ESRD.
Results
Among the 170 patients with GN & NS 91 (53.5%) entered in Remission and 38 progressed to ESRD (22.5%). The patients with GN & NS entering Remission are significantly different from patients GN & NS progressing to ESRD; the Remission patients show higher baseline and last eGFR (<0.0001) and significantly lower values of all histologic and proteinuric parameters. The patients with GN & NS progressing to ESRD show lower values of baseline and last eGFR and significantly higher values of GGS% (0.0016), TID score (0.00048), AH score (0.0001), TUP/C (<0.0001), IgG/C (0.0016), α2m/C (0.001), Alb/C (0.0001), α1m/C (0.0001) and last 24 hours proteinuria (<0.0001) (Table 2). In synthesis the patients GN & NS progressing to ESRD show lower values of baseline and last eGFR and higher values of all histologic and proteinuric parameters (Table 2). Among the 190 patients with GN & PP 126 patients (66.3%) entered Remission and 18 patients progressed to ESRD (9.5%). The patients GN and PP with Remission in comparison with patients progressing to ESRD show higher values of basal and last eGFR (<0.0001); the patients progressing to ESRD show higher values of GGS% (<0.0001), and TID score (<0.0001) and AH score (<0.0001) and higher values of all proteinuric parameters with exclusion of α2m/C (p=0.06). In conclusion the patients with GN & NS and remission show significantly higher values of baseline and last eGFR and significantly lower values of all histologic and proteinuric parameters in comparison with patients with ESRD. Conversely the patients with GN and PP and ESRD show lower values of baseline and last eGFR and higher values of all histologic and proteinuric parameters while the patients GN&PP and ESRD.
Conclusions
Remission: The patients with GN&PP are characterized by a little higher percentage of remission (66.3%) in comparison with GN&NS patients (53.5%). Conversely the GN&NS are characterized by higher percentage of ESRD (22.5%) in comparison with GN&PP patients (9.5%). The patients GN&NS with Remission are characterized by significantly higher values of all proteinuric parameters (UPT/C, IgG/C, α2m/C,. Alb/C and α1m/C), and low values of histologic parameters (GGS%, TID score, AH score). ESRD: The patients GN&NS with ESRD (22.3%) are characterized by significant higher values of all proteinuric parameters and low values of histologic parameters. The patients GN&PP with ESRD (9.3%) are characterized by low values of all proteinuric parameters and significant higher values of all histologic parameters (GGS%, TID score, AH score).The data reported in this study may be useful to assess in another study the responsiveness of the different outcomes to various types of therapy such as Steroids & Cyclophosphamide and Acei drugs alone and in combination.
References
- Bazzi C, Usui T, Napodano P, Nangaku M. Is the Amount of Proteinuria the Main Responsible of Renal Lesion and Renal Function Decline? Insights from Comparison between 204 Patients with Glomerulonephritis and Nephrotic Syndrome and 199 with Persistent Non-Nephrotic Proteinuria. Austing J Nephrol Hypertens. 2020; 7: 1.
- Abbate M, Zoja C, Remuzzi G. How Does Proteinuria Cause Progressive Renal Damage. J Am Soc Nephrol. 2006; 17: 2974-2982.
- Zoia C, Abbate M, Remuzzi G. Progression of renal injury toward interstitial inflammation and glomerular Sclerosis is dependent on abnormal protein filtration. Nephrol Dial Transplant. 2015; 30: 706-712.
- Gentile G, Remuzzi G. Novel Biomarkers for Renal Diseases ? None for the moment (but One). J Biomolecular Screening. 2016; 21: 655-670.
- Bazzi C, Bakoush O. Proteinuric biomarkers in Chronic Kidney Disease. In: Patel VB, Preedy VR (Ed). Biomarkers in Kidney Disease, Vol 1, London, UK, 2016; Chapter 23: 515-533.
- Menon MC, Chuang PY, He CJ. The Glomerular Filtration Barrier: Components and Crosstalk. Int J Nephrol. In: Special Issue: Proteinuria: From Molecular to Clinical Application in Glomerulonephritis. Bazzi C. Bakoush O, Gesualdo L (Ed). 2012: Article ID 74910, DOI: 10.1155/2012/749010.
- Menzel S, Moeller MJ. Role of the podocyte in Proteinuria. Pediatr Nephrol. 2011; 26: 1775-1780.
- Nangaku M. Mechanisms of tubulointerstitial injury in the kidney: final common pathways to end-stage renal failure. Intern Med. 2004; 43: 9-17.
- Nangaku M. Chronic hypoxia and tubulointerstitial injury: a final common pathway to end-stage renal failure. J Am Soc Nephrol. 2006; 17: 17-25,
- Bazzi C, Stivali G, Rachele G, Rizza V, Casellato D, Nangaku M. Arteriolar hyalinosis and arterial hypertension as possible surrogate markers of reduced interstitial blood flow and hypoxia in glomerulonephritis. Nephrology. 2015; 20: 11-17.
- Hostetter TH, Olson JL, Rennke HG, Venkatachalam MA, Brenner BM. Hyperfiltration in remnant nephrons: a potentially adverse response to renal ablation. Am J Physiol. 1981; 241(1): F85-F93.
- Van der Meer I, Cravedi P, Remuzzi G. The role of renin angiotensin system inhibition in kidney repair. Fibrogenesis Tissue Repair. 2010; 3: 7.
- Takeuchi A, Yoshizawa N, Kubota T, Niwa H. A clinicopathologic study of focal segmental glomerulosclerosis: comparison between nephrotic and non-nephrotic focal segmental glomerulosclerosis. Jpn I Med. 1989; 28: 577-584.
- Ellam TJ, El Nahas M. Proteinuria Thresholds Are Irrational: A call for Proteinuria Indexing. Nephron Clin Pract. 2011; 118: c217-c224.
- Ronda N, Cravedi P, Benozzi L et al. Early Proinflammatory Activation of Renal Tubular Cells by Normal and Pathologic IgG. Nephron Exp Nephrol. 2005; 100: e77-e84.
- Abbate M, Zoja C, Corna D, Capitanio M, Bertani T, Remuzzi G. In Progressive Nephropaties, Overload of Tubular Cells with Filtered Proteins Translates Glomerular Permeability Dysfunction into Cellular Signals of Interstitial Inflammation. J Am Soc Nephol. 1998; 9: 1213-1224.
- Thomas ME, Harris KPG. Walls J, Furness PN, Brunskill NJ. Fatty acids exacerbate tubulointerstitial injury in protein-overload proteinuria. Am J Physiol Renal Physiol. 1998; 173: 1286-1294.
- Ruggiero C, Elks CM, Kruger C, Cleland E et al. Albumin-bound fatty acids but not albumin itself alter redox balance in tubular epithelial cells and induce a peroxide-mediated redox-sensitive apoptosis. Am J Physiol Renal Physiol. 2014; 306: F896-F906.

