Clinical Image - Volume 3 - Issue 6
Doctor-patient communication: Content or process?
Jose Luis Turabian*
Specialist in Family and Community Medicine, Health Center Santa Maria de Benquerencia. Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain.
Received Date : Oct 09, 2023
Accepted Date : Nov 14, 2023
Published Date: Nov 21, 2023
Copyright:© Jose Luis Turabian 2023
*Corresponding Author : Jose Luis Turabian, Specialist in Family and Community Medicine, Health Center Santa Maria de Benquerencia. Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain.
Email: jturabianf@hotmail.com
DOI: Doi.org/10.55920/2771-019X/1584
Clinical Image
In the doctor-patient interview, there is a tendency to think of a dichotomy between content or background (the patient's complaint, his symptoms, medical decision-making subject to evidence -evidence-based medicine (EBM)-, drug prescription, etc.) and the process or form of the interview (the modality of the doctor-patient relationship, empathy/assertiveness, sympathy, compassion, transference and countertransference, the placebo effect, etc.). This approach is as reductionist as the usual mind-body dualism. And the problem is that, as in the bio-psychosocial (BPS) approach, the holistic content-process approach to doctor-patient communication has not been integrated into the daily practice of general practitioners (GPs) with little time, who care for most patients with acute and chronic, physical and mental illnesses [1, 2]. General Medicine (GM) presents special characteristics that differentiate it from other medical specialties. In GM it is necessary to evaluate the presentation of symptoms, in addition to the symptoms themselves. That is, the reason for the consultation initiates or emphasizes important issues for the pat ient, and not just symptoms, in a communication context [3, 4]. GPs often assume that in consultation the patient will ment ion the most important symptoms and signs in relation to it, and that patients will spontaneously report all their fears and worries; neither of these assumptions is true (5). When a pat ient comes to the office, the GP must face a certain amount of uncertainty about the evaluation and optimal treatment of it. Uncertainty is frequently represented in terms of probability or normative reasoning, and EBM. But, the reason for consultation expressed by the patient is only a manifest content. The GP must transform or complete those ideas that are latent or initially hidden [6, 7]. Symptoms are often "disorganized", not readily recognizable, and can be presented by symbols, as does the arrangement of notes in a musical score. Perhaps the family doctor has to approach the symptoms as if they were "music": like a mysterious constellation; seeking order in disorder, or better trying to understand some of the disorder [8]. The symptom is an indicator of a process that is not always fully visible. The loss of internal balance manifests itself in the body in the form of a symptom. In addition, the symptom is not an enemy whose destruction should be the main objective, but can be an ally to find the disease. In reality, the symptom indicates what the patient “misses” (9). The GP try of knowing the latent material by means of “reading the patient’s manifest signs and symbols”. The messages of our patients contain “facts” and “feelings”, and we must be attent ive and understand the emotional messages. The reason for consultation / symptom / manifest problem that the patient initially expresses is a “symbolic representation” (with universal and particular symbols); and in addition, the doctor looks for what seems to be the cause of the patient's problem in the doctor-patient relationship itself [10]. The process of communication or presentation of the reason for the visit that the patient makes to the doctor is itself a content of the health problem, it gives information about the psychic life, and it can be a signal that tells the doctor which direction to take [11-13]. In order to fully understand the symptom we must distance ourselves from the usual valuations. It is convenient to replace an excessively analytical and rational thought, with another plastic, symbolic and analogical one. Illness is a system of interpretation; and to understand disease we have to see a system of relationships. The emotional response expressed by the patient has the effect of a linguistic transfer from social complexity to psychic complexity. Illness is expressed as a contrast –not as its own unequivocal entity, but as a contrast between relationship systems-, as in painting a contour, a line, appears from the contrast between two colours instead of how a line is actually drawn [14].
Figure 1: Process and content feed back.
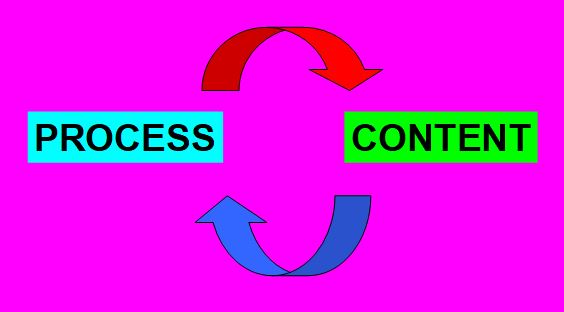
On the other hand, the doctor's communication with the pat ient implies a technical content: informative, or persuasive or reflective communication. The doctor gives advice, or gives support and encouragement, or in this meeting, the doctor and patient talk in such a way that the patient gains confidence in her ability to find solutions to problems [15]. Likewise, the medical decision (for example, pain management, hypertension, diabetes, asthma, anxiety, depression COPD, musculoskeletal or genitourinary problems, cancer, migraine, etc.), the request for complementary tests and the pharmacological prescription, may seem to be elements of true technical content, neutral or alien with respect to the doctor-patient relationship and to emotional or psychological factors; however that is false. All these decisions are emotional (they have a large percentage of emotional and contextual factors). The doctor-patient communication is the distinctive fact of the GP, and where the therapeutic, educational or health promotion intervention is installed. The GP relationship process has a positive or negative therapeutic role in all consultations [16]. So, it is important to recognize the implication of the therapeutic potential of the doctor-patient communication or interview [17], as well as the fact that there is a strong association between communication skills and the content of the consultation [18]. The physician's care in this process lays the foundations of the therapeutic alliance [19]. The words and attitudes of the GP have enormous significance for patients and relatives during the consultation process. They will pay close attention to what is said to them and how it is said to them, and will often remember those words throughout their lives [20]. As in the BPS model, where biological, psychological and social processes are integrated and inseparable, and as it happens with verbal and nonverbal communication that are inseparable and they occur together, and that likewise, the function and meaning of behaviors in a sequence of communication between doctor-patient can be better understood by analyzing their relationship with the social and physical situation in which they are embedded, that is, taking into account the context in which they occur [21], technical content and the communication process go hand in hand and cannot be separated. In short, for purely pedagogical reasons one can speak of form and content. But in reality both elements are connected: the form manifests content, and the content gives meaning to the form. For example, in a painting, the material components of the painting, such as canvas and colours, are carriers and transmitters of an idea or inner image of the artist. The canvas and the colours (content) allow the visualization of the latent or invisible, and therefore, they are a physical expression of content. In the doctor's and patient's office, the phrase "The medium is the message" should be applied, coined by Marshall McLuhan, which means that the shape of a medium is embedded in any message it transmits or transports, creating a symbiotic relationship in which the medium influences how the message is perceived. What is important in doctor-patient communication is not the process or the content; it is the process and the content; and both feed back (FIGURE 1). It is not a question of giving less value to the traditional medical technical skills of the EBM and of the doctor's expert centered on classic contents, but to be aware that this necessarily implies a certain communicative process; and that a certain communicative form implies a medical content.
References
- Fricchione G. Mind body medicine: a modern bio-psycho-social model forty-five years after Engel. BioPsychoSocial Med. 2023; 17(12). https://doi.org/10.1186/s13030-023-00268-3. https://bpsmedicine.biomedcentral.com/articles/10.1186/s13030-023-00268-3#citeas
- Turabian JL. “Empathies” Rather than “Empathy” in The Clinical Context Of General Medicine: Acute Or Chronic Diseases, Physical Or Mental Health Problems and Types Of Doctor-Patient Relationships. Psychiatry and Psychological Disorders. 2023; 2(2). https://mediresonline.org/article/empathies-rather-than-empathy-in-the-clinical-context-of-general-medicine-acute-or-chronic-diseases-physical-or-mental-health-problems-and-types-of-doctor-patient-relationships
- Turabián JL, Pérez Franco B. The process by which family doctors manage uncertainty: Not everything is zebras or horses. Aten Primaria. 2006; 38(3): 165-7. https://pubmed.ncbi.nlm.nih.gov/16945276/
- Turabián JL, Pérez Franco B. The symptoms in family medicine are not symptoms of disease, they are symptoms of life]. Aten Primaria. 2012; 44(4): 232-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7025203/
- Epstein RM, Mauksch L, Carroll J, Jaén CR. Have You Really Addressed Your Patient's Concerns? Have You Really Addressed Your Patient's Concerns? Fam Pract Manag. 2008; 15(3): 35-40. http://www.aafp.org/fpm/20080300/35have.html
- Rosendal M, Jarbøl DE, Pedersen AF, Andersen RS. Multiple perspectives on symptom interpretation in primary care research. BMC Family Practice. 2013; 14: 167. https://www.ncbi.nlm.nih.gov/pubmed/24188544
- Rudebeck CE. The clinical method of general practice. Scand J Prim Health Care. 1991; (supple 1): 30-9. http://www.tandfonline.com/doi/abs/10.3109/02813439209014088
- 8.Turabian JL. Prognosis-based medicine-The importance of psychosocial factors: Conceptualization from a case of acute pericarditis. Trends Gen Pract. 2018; 1(1): 1-2. http://www.oatext.com/prognosis-based-medicine-the-importance-of-psychosocial-factors-conceptualization-from-a-case-of-acute-pericarditis.php#Article
- https://www.oatext.com/pdf/TGP-1-101.pdf
- Heim E. Illness as a crisis and opportunity]. Stuttgart, Berlín: Kreuz-Verlag. 1980.
- Turabian JL. Interpretation of the Reasons for Consultation: Manifest and Latent Content. the Initiation of the Diagnostic Process in General Medicine. Archives of Community and Family Medicine. 2019; 2(1). https://www.sryahwapublications.com/archives-of-community-and-family-medicine/pdf/v2-i1/1.pdf
- Turabian JL. Symptomatic Acts. A Type of Guidance Signs Not to Get Lost in the Forest of the Clinic in General Medicine. Presentation and Conceptualization from Two Cases. J Case Rep Med Spec. 2019; 1-10. https://www.researchgate.net/profile/Jose-Turabian-2/publication/337399385_Case-Report_Abstract_Symptomatic_Acts_A_Type_of_Guidance_Signs_Not_to_Get_Lost_in_the_Forest_of_the_Clinic_in_General_Medicine_Presentation_and_Conceptualization_from_Two_Cases/links/5dd56260299bf11ec866ae98/Case-Report-Abstract-Symptomatic-Acts-A-Type-of-Guidance-Signs-Not-to-Get-Lost-in-the-Forest-of-the-Clinic-in-General-Medicine-Presentation-and-Conceptualization-from-Two-Cases.pdf
- Freud S. Psychopathology of everyday life. Madrid: Alianza Editorial. 1966.
- Heath C. Demonstrative Suffering: The Gestural (Re)embodiment of Symptoms. J Commun. 2002; 52: 597-616. https://academic.oup.com/joc/article-abstract/52/3/597/4110034
- May C, Allison G, Chapple A, et al. Framing the doctor-patient relationship in chronic illness: a comparative study of general practitioners' accounts. Sociol Health Illn. 2004; 26(2): 135-58
- http://home.attbi.com/~miketerpstra1/illnessrelshp.html
- Turabián JL, Pérez-Franco B. Too many theories of health promotion?. Med Clin (Barc). 2006; 126(5): 198. https://pubmed.ncbi.nlm.nih.gov/16469286/
- Hellström O. Health promotion in general practice. One meanings and aims in interaction. Eur J Public Health. 1994; 4(2): 119-24. http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-98529
- Adler HM. The history of the present illness as treatment: who's listening, and why does it matter? J Am Board Fam Pract. 1997; 10: 28-35. https://pubmed.ncbi.nlm.nih.gov/9018660/
- Gude T, Vaglum P, Anvik T, et al. Observed communication skills: how do they relate to the consultation content? A nation-wide study of graduate medical students seeing a standardized patient for a first-time consultation in a general practice setting. BMC Medical Education. 2007; 7: 43. https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-7-43
- Charon R. Narrative and medicine. N Engl J Med. 2004; 350 (9): 862-4. https://pubmed.ncbi.nlm.nih.gov/14985483/
- Núñez S, Marco T, Burillo-Putze G, Ojeda J. Procedures and skills for the communication of bad news in emergency units. Med Clin (Barc). 2006; 127: 580-3. https://pubmed.ncbi.nlm.nih.gov/17145016/
- Kuehn BM (2012) Patient-centered care model demands better physician-patient communication. JAMA; 307(5): 441-2. https://pubmed.ncbi.nlm.nih.gov/22298662/

