Research article - Volume 4 - Issue 2
Investigating the risk of non-alcoholic fatty liver disease and fibrosis in type 2 diabetics
Bagdagul Yuksel Guler¹; Cem Haymana²; Ibrahim Demirci³*; Alper Sonmez³
1Sincan Education and Research Hospital, Department of Endocrinology, Sincan, Ankara, Türkiye
2University of Health Sciences, Gulhane School of Medicine, Department of Endocrinology and Metabolism, Etlik, Ankara, Türkiye.
3Department of Endocrinology and Metabolism, Ankara Guven Hospital, Turkey.
Received Date : Jan 29, 2024
Accepted Date : Feb 23, 2024
Published Date: Mar 01, 2024
Copyright: © Demirci I 2024
*Corresponding Author : Ibrahim demirci Department of Endocrinology and Metabolism, Ankara Guven Hospital, Turkey.
Email: dr.idemirci@gmail.com
DOI: Doi.org/10.55920/2771-019X/1639
Abstract
Aim: Non-alcoholic fatty liver disease (NAFLD) is very common in individuals with type 2 diabetes. The frequency of NAFLD in type 2 diabetics in our country and how many of these cases have fibrosis are unknown. This study aimed to determine the risk of fibrosis in type 2 diabetics with a noninvasive, easy method.
Method: In the study, the records of adult type 2 diabetes cases who applied to an endocrinology outpatient clinic between 1-30 April 2022 were retrospectively examined. Pregnant women, patients with type 1 diabetes, and those with a history of chronic liver disease due to other causes were excluded. The risk of fibrosis was calculated with ‘’FIB4 Score = [ (Age x AST) / (Platelet x √(ALT)]’’. Age, gender, concomitant diseases, diabetic complications of all cases were also recorded.
Discussion: With this study, it is understood that more than one third of type 2 diabetics who apply to a tertiary endocrinology outpatient clinic are at risk of NAFLD and related fibrosis. It is important to know that these patients are at increased risk not only for liver cirrhosis but also for coronary artery disease, and patients should be evaluated carefully in this regard in clinical practice. This study shows that the FIB-4 score should be expanded in the follow-up of cases with type 2 diabetes in our country and that cases with medium-high risk should be subjected to further evaluation in cooperation with gastroenterology/hepatology clinics.
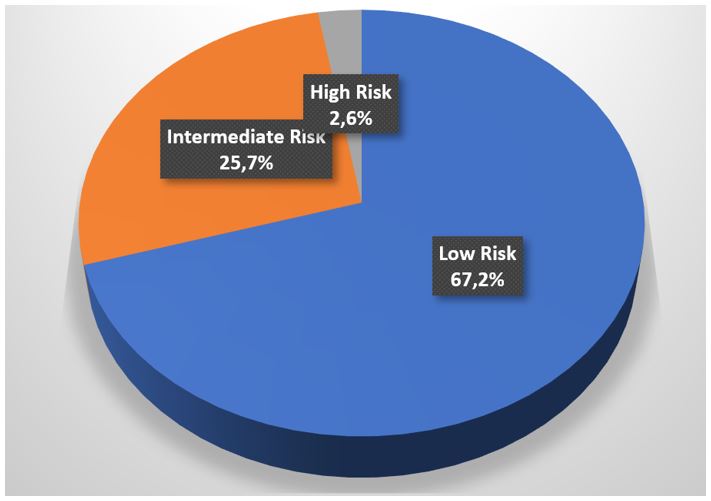
Results: 997 type 2 diabetic patients were included in the study. Low-risk (n=671, 67.2%), medium-risk (n=257, 25.7%) and high-risk (n=26, 2.6%) patients were identified according to the FIB-4 score. It was observed that the diagnosis of coronary artery disease was significantly higher in patients in the medium and high risk groups (p < 0.05).
Introduction
Non-alcoholic fatty liver disease (NAFLD) is defined as the accumulation of 5% or more fat in the liver when no other causes are present [1]. It has been reported that one in four people worldwide have NAFLD, with even higher rates in the Middle East and South America [2]. Given the global obesity epidemic and Türkiye's status as having the highest obesity prevalence in Europe, NAFLD is a significant concern for our country. Non-alcoholic fatty liver disease is one of the most common causes of chronic liver disease worldwide. However, it is important to note that not all individuals with NAFLD develop advanced liver disease, such as cirrhosis or hepatocellular carcinoma. This raises the question of which individuals are at a higher risk of complications. Research has shown that type 2 diabetes is a more significant risk factor for serious liver disease than obesity and hyperlipidemia, increasing the risk by two-fold [3]. Hepatosteatosis can cause the development of steatohepatitis or cirrhosis, as well as insulin resistance and diabetes [4]. Additionally, type 2 diabetes doubles the risk of advanced fibrosis, cirrhosis-related complications, and mortality due to liver disease [5]. There is a bidirectional relationship between NAFLD and type 2 diabetes. Patients with NAFLD are also at an increased risk for cardiovascular disease and related mortality[6].Ultrasonography is commonly used to diagnose hepatic steatosis in routine practice. Hepatosteatosis is characterized by a bright appearance of liver echo and blurring of hepatic vascular structures. Although magnetic resonancebased measurements are more sensitive in detecting adiposity, they are not frequently used in clinical practice. Some scoring systems have been developed to determine which patients are at higher risk for advanced liver disease. Indices such as NAFLD f ibrosis score, FIB-4 score, and AST/platelet ratio are practical and inexpensive methods based on laboratory parameters and demographic data commonly used in daily practice. It is important to note that type 2 diabetes is a significant risk factor for the development of advanced liver disease. Therefore, the availability of easy-to-use and inexpensive methods to assess a large population is crucial. While studies have shown that the FIB-4 score can effectively detect liver cirrhosis or hepatocellular carcinoma in patients with diabetes, there is currently no population study on this subject in our country [7]. The objective of this study was to calculate FIB-4 scores in individuals with type 2 diabetes, which represents a significant portion of the applications to our outpatient clinic. Additionally, we aimed to determine the proportion of this patient group that has a moderate to high level of fibrosis risk according to the FIB-4 score.
Materials and Methods
The study retrospectively examined the records of patients who applied to endocrinology outpatient clinic of a tertiary center between April 1, 2022, and May 1, 2022. The study included patients aged 18 years and older with type 2 diabetes mellitus. Patients with type 1 diabetes mellitus, latent autoimmune diabetes in adults (LADA), autoimmune hepatitis, viral hepatitis, alcohol-related liver cirrhosis, or malignancy were excluded from the study due to potential effects on liver enzyme levels. The patient records included information on age, gender, duration of diabetes, height, weight, and any comorbidities present, such as hypertension, dyslipidemia, coronary artery disease, congestive heart failure, asthma/ chronic obstructive pulmonary disease and hypothyroidism. Micro and macrovascular complications, including retinopathy, neuropathy, nephropathy, history of cerebrovascular disease/ transient ischemic attack, and diabetic foot were also recorded. The laboratory parameters that were screened include alanine aminotransferase (ALT), aspartate aminotransferase (AST), platelet count, low density lipoprotein (LDL) cholesterol, triglyceride, high density lipoprotein (HDL) cholesterol, and HbA1c levels. Age, ALT, AST, and platelet counts were used to calculate the FIB-4 score. The FIB-4 score was calculated using the formula (Age x AST)/(Platelet√ALT). Patients with a FIB-4 score < 1.3 were classified as having the lowest risk of fibrosis, those with scores between 1.3 and 2.67 were classified as having intermediate risk, and those with scores ≥ 2.67 were classified as having high risk [8]. The study also evaluated survival data and whether patients in the high-risk group underwent liver imaging.The study protocol received approval from the Clinical Research Ethics Committee of Health Sciences University Gülhane Training and Research Hospital (Acceptance no:2023/102 Date:17.05.2023) and was conducted in accordance with the revised 2013 Declaration of Helsinki. Statistical analyses were conducted using SPSS Ver. 22.0 (IBM Corp., Armonk, N.Y, USA). The normal distribution conformity of continuous variables was calculated using the Shapiro-Wilk test. Continuous variables were presented as mean±standard deviation (SD), median (interquartile range, IQR), minimum value-maximum value. Categorical variables were presented as number (n) and percentage (%). Chi-square test was used to evaluate differences in categorical variables, such as gender, between groups with low, medium, and high FIB-4 scores. The student’s t-test was used to evaluate intergroup differences of continuous variables with normal distribution, while Mann-Whitney U test was used for continuous variables without normal distribution. To evaluate differences between three or more groups of continuous variables with normal distribution, we used a one-way ANOVA test. For continuous variables without normal distribution, we used the Kruskal Wallis test. Simple and partial correlations were analyzed using the Pearson correlation coefficient for normally distributed continuous variables and the Spearman correlation coefficient for non-normally distributed continuous variables. Univariate and multivariate logistic regression analyses were conducted to identify the variables independently associated with the outcomes. A significance level of p < 0.05 was used for all comparisons.
Results
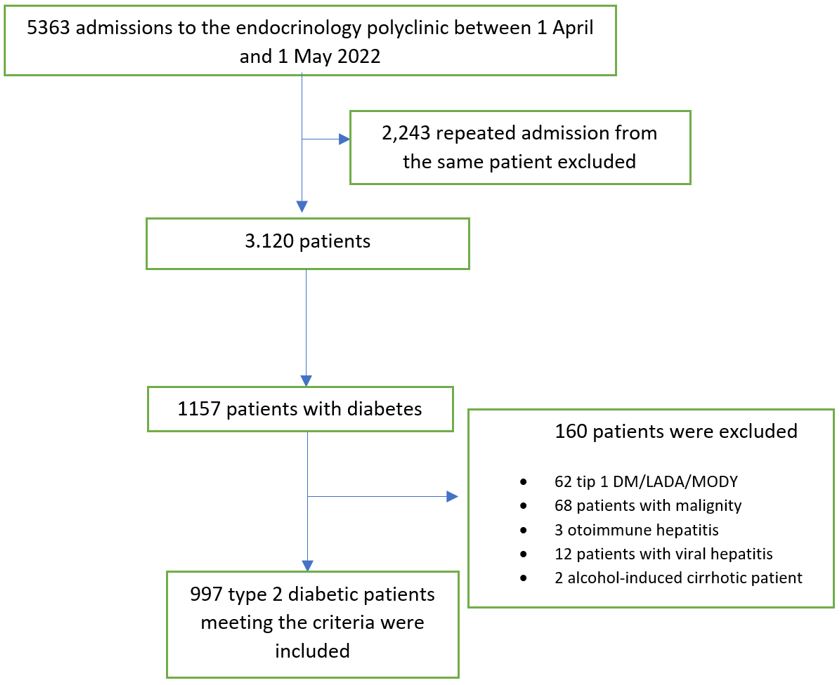
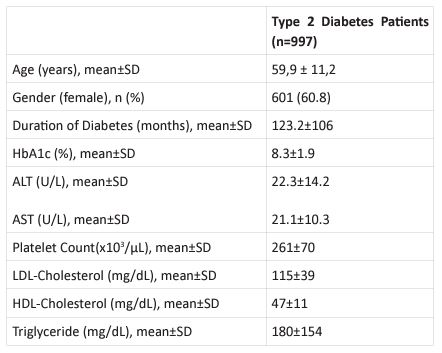
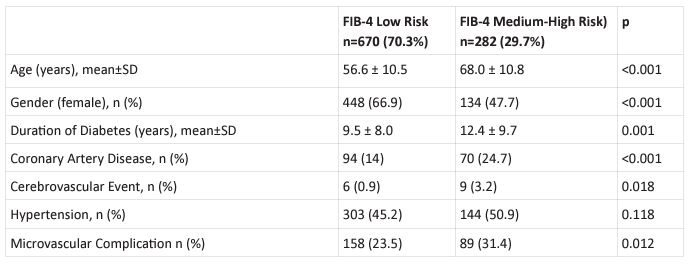
The study involved 997 patients who met the criteria for type 2 diabetes (Figure 1). We excluded 62 patients with diabetes other than type 2, 68 patients with malignancy, 3 patients with autoimmune hepatitis, 12 patients with viral hepatitis, and 2 patients with alcohol-related liver cirrhosis. The study included patients with an average age of 59.9 ± 11.2 years and a mean duration of diabetes of 123.2 ± 106 months. The female population accounted for 60.8% of the patients. Table-1 provides demographic and laboratory parameters of the patients. When the patients' FIB-4 scores were calculated and categorized according to risk groups, 67.2% were in the low-risk category, 25.7% in the medium-risk category, and 2.6% in the high-risk category (Figure-2). FIB-4 scores could not be calculated in some patients due to missing laboratory data. The study divided patients into two risk categories, low and medium-high, based on their FIB-4 scores. Analysis of demographic data and comorbidities revealed that the risky group was comprised of older patients with longer duration of
Figure 1: Flowchart on the patient inclusion process.
Figure 2: Distribution of patients according to FIB-4 score.
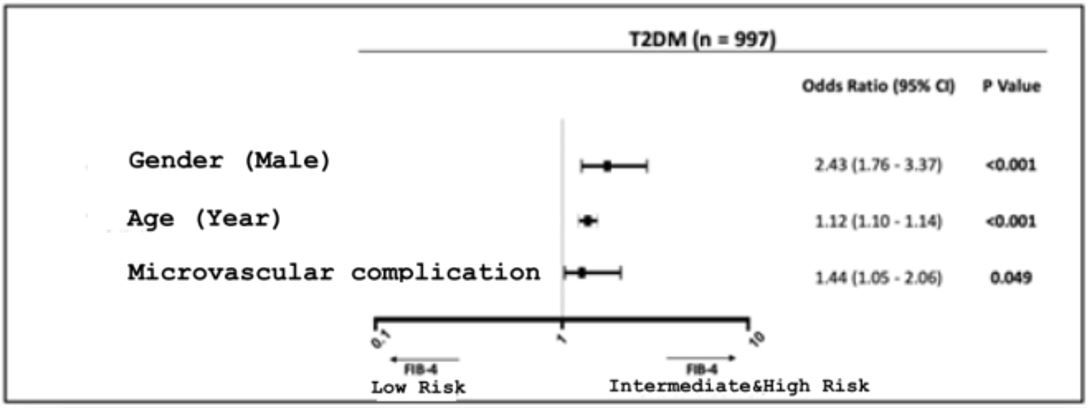
Figure 3: Determinants of High FIB-4 Score.
Table 1: Demographic and laboratory characteristics of the patients.
Table 2: Comparison of demographic data and comorbidities according to FIB-4 score.
diabetes. Patients in the medium-high risk category according to the FIB-4 score had a significantly higher incidence of coronary artery disease. Additionally, a higher FIB-4 score was found to be associated with an increased risk of microvascular complications (Table 2).
Regression analysis was conducted to identify the determinants of a high FIB-4 score. The results showed that male gender, advanced age, and microvascular complications significantly increased the FIB-4 score (Figure 3). Among patients in the high-risk category with a FIB-4 score ≥ 2.67, four had died at the time of screening, but the cause of death could not be determined from their medical records. Upon closer examination of the high-risk group, it was discovered that 40% of these patients had not undergone any liver imaging in the past 5 years, despite their high-risk scores.
Discussion
This study represents the largest patient cohort in a single center in Türkiye to evaluate the risk of fibrosis in patients with type 2 diabetes. It is common in clinical practice to overlook the assessment of NAFLD while investigating complications such as retinopathy, nephropathy, and neuropathy. However, it is wellestablished that individuals with type 2 diabetes have a higher prevalence of NAFLD compared to the general population, and are at an increased risk of developing advanced liver disease. Although guidelines have recommended screening for micro- and macrovascular complications in patients with diabetes for many years, ultrasonography for the detection of NAFLD in individuals with type 2 diabetes or prediabetes was only recommended by the American Diabetes Association (ADA) in 2019 guideline [9]. In the most recent guidelines of the Turkish Society of Endocrinology and Metabolic Diseases, it is recommended that patients with diabetes and NAFLD should be monitored with noninvasive imaging tools such as elastography and referred to gastroenterology specialists in the presence of fibrosis findings [10]. However, the difficulty in accessing elastosonography in practice is one of the major factors limiting its use. Due to the rapidly increasing prevalence of diabetes in Türkiye, there is a need for simple, easily accessible, and inexpensive screening methods [11]. The FIB-4 score, which we chose to determine the risk of fibrosis in our study, is valuable because it can be easily evaluated even during primary health care. However, it has a major disadvantage in that it can be affected by many factors that can also affect liver function tests and platelet count. The results on how effective the FIB-4 score is in predicting the severity of fibrosis vary in studies. Although there are publications stating that it is not a useful tool due to high false positive and false negative rates in the general population where the prevalence of fibrosis is low, there are also opinions that systematic screening of diabetic patients should start with FIB-4 [12,13]. In a meta-analysis, it was found that the sensitivity of FIB-4 remained <60% but its specificity was 91% when the threshold values for FIB-4 score were <1.3 and ≥2.67.[14]. Based on these data, it can be concluded that the FIB-4 score is a useful and practical tool to answer the question of which patients should be referred to a gastroenterologist in diabetic patients, who are known to have higher fibrosis than the general population.In our study, we used the FIB-4 score thresholds agreed upon by national and international guidelines [8,15]. According to these thresholds, one in four patients with type 2 diabetes is at intermediate to high risk for fibrosis. Identifying this subgroup is extremely important to determine which patients should be referred to gastroenterology clinics. But another point that we now know very well is that NAFLD is a multisystemic problem. It will not be sufficient to follow these patients just from a liver point of view. Individuals with diabetes mellitus with NAFLD are a group of patients who should be watched for increased cardiovascular risk. NAFLD is thought to contribute not only to cardiovascular disease, but also to the development of other cardiac conditions such as LV dysfunction and hypertrophy, atrial fibrillation, and valve calcification [1]. Given that these conditions are common in patients with diabetes, the significance of NAFLD in this patient population will be better understood. One of the major limitations of the present study is its retrospective design. Data such as comorbidities, diabetic complications, medications, and body mass index were not available for some patients. Another limitation of the study is that patients with abnormal thyroid function tests were not excluded. Since the patients in the study population were diabetic patients presenting to the endocrinology outpatient clinic, it is likely that some of them presented with thyroid dysfunction and consequently had elevated liver enzymes. Although interest in NAFLD has increased in recent years, few countries have developed national strategies or policies [5]. In the present study, it was found that even the high-risk group in terms of fibrosis was not adequately evaluated, and 40% of these patients had no liver imaging in the past five years. However, even in the short period of 6 months between the time the patients were admitted and the time the data were analyzed, 15% of the patients in the high-risk group died. Therefore, early identification of high-risk patients may benefit morbidity and mortality by closer followup for hepatic and extrahepatic complications. Presentation at a national or international medical society: 7th Diabetes Associated Diseases Treatment Congress.
Funding statement: The study was not supported by a Foundation.
Conflict of Interest: The authors declare no potential conflicts of interest.
Data access statement: The data supporting this study's findings are available from the corresponding author upon reasonable request.
Authorship Contribution Statements: The authors confirm responsibility for study conception and design, data collection, analysis and interpretation, and manuscript preparation.
References
- Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1 Suppl):S47-64.
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
- Jarvis H, Craig D, Barker R, Spiers G, Stow D, Anstee QM, Hanratty B. Metabolic risk factors and incident advanced liver disease in non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis of population-based observational studies. PLoS Med. 2020;17(4):e1003100.
- Viscarra J, Sul HS. Epigenetic Regulation of Hepatic Lipogenesis: Role in Hepatosteatosis and Diabetes. Diabetes. 2020;69(4):525-31.
- Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397(10290):2212-24.
- Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69(9):1691-705.
- Kawata N, Takahashi H, Iwane S, Inoue K, Kojima M, Kohno M, et al. FIB-4 index-based surveillance for advanced liver fibrosis in diabetes patients. Diabetol Int. 2021;12(1):118-25.
- Kaya A. Diyabete Bağlı Nonalkolik Yağlı Karaciğer Hastalığı Tanı ve Tedavi Rehberi. 2022.
- American Diabetes A. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S34-S45.
- Derneği TEvM. Diabetes Mellitus ve Komplikasyonlarının Tanı, Tedavi ve İzlem Kılavuzu 2022.
- Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28(2):169-80.
- Graupera I, Thiele M, Serra-Burriel M, Caballeria L, Roulot D, Wong GL, et al. Low Accuracy of FIB-4 and NAFLD Fibrosis Scores for Screening for Liver Fibrosis in the Population. Clin Gastroenterol Hepatol. 2022;20(11):2567-76 e6.
- Castera L, Cusi K. Diabetes and cirrhosis: Current concepts on diagnosis and management. Hepatology. 2023;77(6):2128-46.
- Mozes FE, Lee JA, Selvaraj EA, Jayaswal ANA, Trauner M, Boursier J, et al. Diagnostic accuracy of non-invasive tests for advanced fibrosis in patients with NAFLD: an individual patient data meta-analysis. Gut. 2022;71(5):1006-19.
- Cusi K, Isaacs S, Barb D, Basu R, Caprio S, Garvey WT, et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract. 2022;28(5):528-62.