Case Report - Volume 4 - Issue 2
Revision of total knee arthroplasty with a hinge-type cemented total prosthesis and augments for the internal tibial plateau was performed following a periprosthetic fracture: Case report
Gelu Florin Murvai1*; Calin Tudor Hozan, Calin Magheru1; Gheorghe Szilagyi1; Madalin Bulzan1; Viorela Romina Murvai1; Simona Cavalu2
1Clinical Department, Faculty of Medicine and Pharmacy, University of Oradea, 410068 Oradea, Romania.
2Preclinical Department, Faculty of Medicine and Pharmacy, University of Oradea, 410087 Oradea, Romania.
Received Date : Feb 09, 2024
Accepted Date : Mar 05, 2024
Published Date: Mar 12, 2024
Copyright: © Murvai GF 2024
*Corresponding Author : Gelu Florin Murvai Clinical Department, Faculty of Medicine and Pharmacy, University of Oradea, 410068 Oradea, Romania.
Email: gelu.f.murvai@gmail.com
DOI: Doi.org/10.55920/2771-019X/1646
Introduction
Methodology: In this study, we present a case study of a patient who underwent a total knee replacement (TKA) and subsequently suffered a periprosthetic fracture. The surgical intervention was carried out without using a hemostatic band, and the postoperative treatment excluded the administration of non-steroidal anti-inflammatory drugs (NSAIDs) for the first 7 days. The periprosthetic fracture occurred in the left tibial plateau and was observed in a patient with a cemented knee prosthesis. To address this issue, a revision total knee arthroplasty was performed. During this procedure, the original prosthesis was replaced with a hinge-type prosthesis, and augmentations were added to support the internal tibial plateau.
Results and discussion
The patient in question is a 73-year-old woman from an urban environment who was admitted to the Orthopedics Department 1 of SCJU Bihor with pain in her left knee and relative functional impotence in her left lower limb.
From the anamnesis, we learned that the patient underwent left total knee replacement surgery approximately 2 years ago, performed in another clinic. Initially, the patient felt well postoperatively and resumed her normal physical activity. However, about 1 year after the operation, she went through a difficult time, having experienced the death of two loved ones in a very short interval: her husband and son. These events led to both mental and physical deterioration of the patient's condition. Later, the patient suffered a fall at home from the same level, resulting in a periprosthetic fracture of the internal tibial plateau in her left knee.
The patient refused to be operated on again at the center where she was initially treated and arrived at the Orthopedics 1 ward of SCJU Bihor approximately one year after the fracture. During this interval, the patient mobilized with the help of a walking frame.
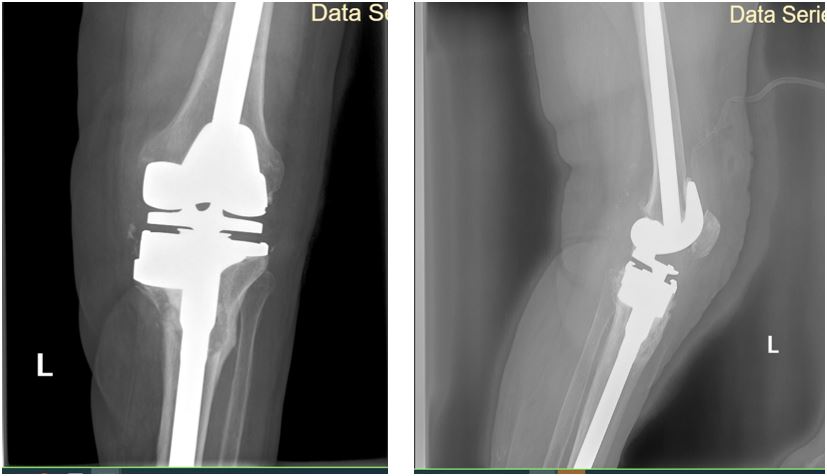
On admission, she underwent a clinical examination, radiographs (figure 1), laboratory tests, and an EKG. Treatment with anti-algesics, anticoagulants, antibiotics, and infusion solutions was also instituted.
Figure 1: Presentation of lateral (A) and anteroposterior (B) radiographs at the time of admission to our ward, 1 year after trauma, with an attached video (C).
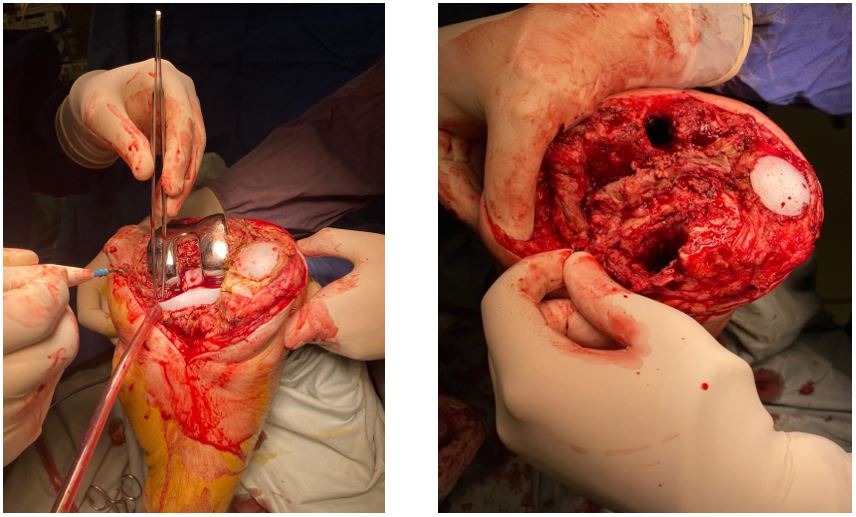
Figure 2: Intraoperative pictures before removal of the prosthetic components (A) and after removal of the prosthesis (B).
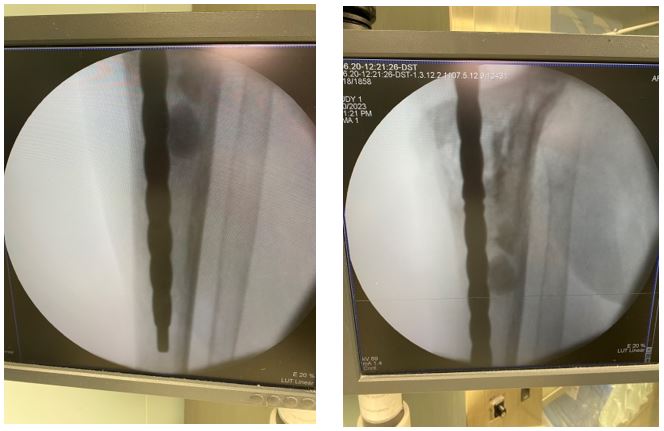
Figure 3: Reaming of the tibial medullary canal under radiological control in the first phase (A) and after successful removal of cement remaining in the femoral canal (B).
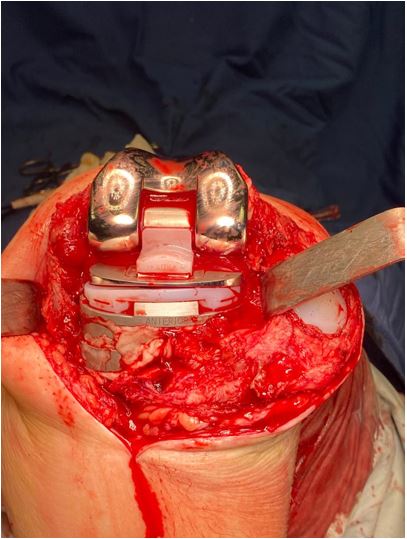
Figure 4: Intraoperative photo after mounting the new prosthesis, before wound closure. The operation was performed without the use of hemostasis tape.
On clinical examination, the left knee was found to be swollen, with global deformity, varus deviation of the knee axis, and approximately 3 cm of shortening compared to the contralateral lower limb. Additionally, marked instability of the ligaments was observed, and the varus stress test was positive.
Gait examination revealed a difficult gait (video in Figure 1C), with support on the walking frame and a shortening of the loading time on the left lower limb.
After operative planning and adequate preparation of the patient, the surgical intervention called "Revision of total knee arthroplasty with cemented hinge-type total prosthesis and augments for the internal tibial plateau" was performed.
During the surgery, a fracture with infiltration and marked bone destruction was found at the level of the medial tibial plateau (Figure 2A). The prosthetic components were extracted, and nonviable and fibrosed periprosthetic tissues were removed (Figure 2B).
One of the major problems encountered intraoperatively was the presence of remaining cement in the femoral and tibial canal, which was successfully removed with reamers under radiological control (Figure 3).
The rapid immunochromatographic test, with a relative sensitivity of 98% and a relative specificity of 99.6%, was initially negative, then turned positive. A new alternative test method needs to be explored and validated.
Due to the lack of bone substance at the level of the internal tibial plateau, it was necessary to utilize 2 augments to correct the bone defect and restore the normal loading axis of the knee, as depicted in Figure 4.
Paraclinical examination shows the following results: ESR = 15 mm/h, Ac HCV = negative, Uric acid = 7.10 mg/dl, GPT = 15.00 IU/L, Creatinine = 0.89 mg/dL, GGT = 22.00 U/L, Glucose = 103 mg/dL, C-reactive protein = <1 mg/L, urea = 26 mg/dL. ABO/RH group determination = A RH positive, RH/Kell phenotyping = ccEc/Kell negative RH positive, Ag HGs = negative, GOT = 24.0 U/L.
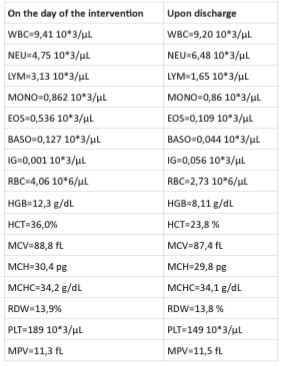
The hematological examination was performed on the day of the intervention and upon discharge of the patient. The results are presented in Table 1.
Table 1: The hematological examination on the day of the intervention and upon discharge of the patient.
Figure 5: Reaming of the tibial medullary canal under radiological control in the first phase (A) and after successful removal of cement remaining in the femoral canal (B).
Figure 6: Reaming of the tibial medullary canal under radiological control in the first phase (A) and after successful removal of cement remaining in the femoral canal (B).
Other parameters: Fibrinogen = 345 mg/dl, PT = 12.2 sec, INR = 1.08, Prothrombin activity = 87%, APTT (sec) = 29.9 sec, APTT (%) = 0.97%.
Urine examination: Bilirubin = 0 µmol/L, Urobilinogen = normal, Ketones = normal, Glucose = 0 mmol/L, Protein = 0 g/L, Erythrocytes = 0 CELL/uL, pH = 5.0, Nitrites = negative, Leukocytes = 70 CELL/uL, Density = 1.017, Microalbumin = 10 mg/L, Creatinine = 8.8 mmol/L, Calcium = 2.5 mmol/L, Hematocytes = very rare, Leukocytes = very rare, Flat epithelial cells = negative, Hyaline cylinders = negative, Microbial flora = relatively frequent, leukocyte clusters = negative, Calcium oxalate = negative, Uric acid crystals = negative, Other crystals = negative, Yeasts = negative, erythrocyte clusters = negative, Squamous cells = negative, amorphous salts = negative.
Compatibility: Saline compatibility negative autoantibody, Enzymatic = CM ENZ Comp, AGH = CM AGM Comp.
Postoperatively, following skin repair and application of aseptic dressings, the drain tube is removed, physical therapy is initiated, and the established treatment is continued. 24 hours after surgery, the patient mobilizes and has a favorable evolution, which can also be seen from Figure 5, after the postoperative radiological examination. The patient is discharged after 4 days.
Recommendations at discharge: continuation of anticoagulant treatment (enoxaparin sodium 0.6 ml) for 20 days, alendronic acid with cholecalciferol for 6 months, and administration of aceclofenac 100 mg and omeprazole 20 mg for 10 days, starting 7 days after the postoperative intervention.
14 days after the intervention, the patient returns for a follow-up visit to have the sutures removed. He continues to show favorable progress with a spectacular recovery, achieving 90 degrees of flexion (Figure 6A and 6C), full extension (Figure 6B), and walking with cane support with minimal postoperative pain.
Discussion
The required knee range of motion (ROM) for daily activities has been determined through biomechanical and gait analysis studies. A 2005 study emphasized the importance of range, showing that 67° of flexion is required during the balance phase of walking, 83° for climbing stairs, 100° for descending, 93° for rising from a chair, and between 71° and 117° for grasping an object from the floor [1]. Considering that preoperative flexion is crucial in achieving healthy postoperative flexion [2], in our case study, we encountered limited knee mobility. The inability to maintain adequate knee extension can have a significant negative impact on gait and functional abilities [3]. Flexion contracture causes an increase in energy expenditure and imposes excessive pressure on the quadriceps [4,5]. Post knee joint replacement, intraoperative surgical strategies and intensive rehabilitation methods are utilized to correct the flexion contracture [6,8].
Seyler pointed out that some aggressive postoperative rehabilitation methods may have limitations, and some knee arthroplasty patients may not respond well and continue to experience muscle spasms. In this context, botulinum toxin type A has been used as a temporary neuromuscular transmitter blocker to treat muscle spasms in patients with neurological disorders and as a treatment method for clubfoot [9].
Ceasing non-steroidal anti-inflammatory drugs in the first 7 postoperative days is associated with favoring the healing process [10,11], but other reasons appear in the literature, such as sensitivity to NSAIDs [12,14], or other complications [15,16]. Other studies compared the effect of the combination of Tramadol hydrochloride/acetaminophen with NSAIDs and found that this combination was superior to NSAIDs [17]. In our case, during the first 7 days, the patients received only antialgesic treatment (paracetamol or tramadol, or their combination).
Mizner et al [18] and Yoshida et al [19] suggested that quadriceps femoris strength is one of the strongest predictors of long-term function in patients undergoing total knee replacement (TKA), including stair climbing and chairlift abilities. Similar results were reported by Dennis et al [20], who concluded that patients who underwent TKA and used a tourniquet showed a decrease in quadriceps strength during the first 3 months after surgery. Thus, the use of a tourniquet may adversely affect the early improvement of muscle strength and lower limb function in knee replacement patients.
Surgery with a tourniquet was significantly associated with a higher risk of deep vein thrombosis and infection compared with surgery without a tourniquet. However, no significant association was found between tourniquet surgery and the risk of pulmonary embolism or reoperation compared with non-tourniquet surgery.
Conclusion
Revision of total knee arthroplasty with a hinge-type cemented total prosthesis and augments for the internal tibial plateau resulted in a favorable evolution of knee osteoarthritis, evidenced by reduced local pain and swelling, 90° flexion, and improved mobility. A spectacular recovery was noted, with the patient achieving 90 degrees of flexion, full extension, and walking with cane support, experiencing minimal post-operative pain.
Data availability: The data presented in this study are available within the article. Other data that support the findings of this study are available upon request from the corresponding authors.
Conflicts of interest: The authors declares that there is no conflict of interest regarding the publication of this paper.
Funding statement: This study was funded by University of Oradea.
Acknowledgments: The authors would like to thank to the University of Oradea, for supporting the payment of the invoice, through an internal project.
References
- Carvalho Júnior LHd, Castro CACd, Gonçalves MBJ, Rodrigues LCM, Cunha FVPd, Lopes FdL. Amplitude de movimento após artroplastia total do joelho. Acta Ortopédica Brasileira. 2005; 13.
- Parsley BS, Engh GA, Dwyer KA. Preoperative flexion. Does it influence postoperative flexion after posterior-cruciate-retaining total knee arthroplasty? Clin Orthop Relat Res. 1992; 204-210.
- Burnham RR, Bialek SE, Wozniak A, Brown NM. Does contralateral knee range of motion predict postoperative knee range of motion after total knee arthroplasty? Knee Surgery & Related Research. 2020; 32: 1-6.
- Cheuy VA, Foran JRH, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis Associated with Total Knee Arthroplasty. The Journal of Arthroplasty. 2017; 32: 2604-2611. doi: 10.1016/j.arth.2017.02.005.
- Magit D, Wolff A, Sutton K, Medvecky MJ. Arthrofibrosis of the Knee. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2007; 15.
- Su EP. Fixed flexion deformity and total knee arthroplasty. J Bone Joint Surg Br. 2012; 94: 112-115. doi:10.1302/0301-620x.94b11.30512.
- Bonutti PM, Marulanda GA, McGrath MS, Mont MA, Zywiel MG. Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010; 18: 194-199. doi:10.1007/s00167-009-0947-1.
- McGrath MS, Mont MA, Siddiqui JA, Baker E, Bhave A. Evaluation of a custom device for the treatment of flexion contractures after total knee arthroplasty. Clin Orthop Relat Res, 2009; 467: 1485-1492. doi:10.1007/s11999-009-0804-z.
- Seyler TM, Jinnah RH, Koman LA, Marker DR, Mont MA, Ulrich SD, Bhave A. Botulinum toxin type A injections for the management of flexion contractures following total knee arthroplasty. J Surg Orthop Adv. 2008; 17: 231-238.
- Zhao-Fleming H, Hand A, Zhang K, Polak R, Northcut A, Jacob D, Dissanaike S, Rumbaugh KP. Effect of non-steroidal anti-inflammatory drugs on post-surgical complications against the backdrop of the opioid crisis. Burns Trauma. 2018; 6: 25. doi:10.1186/s41038-018-0128-x.
- Lanas A, Benito P, Alonso J, Hernández-Cruz B, Barón-Esquivias G, Perez-Aísa Á, Calvet X, García-Llorente JF, Gobbo M, Gonzalez-Juanatey JR. Safe Prescription Recommendations for Non Steroidal Anti-inflammatory Drugs: Consensus Document Elaborated by Nominated Experts of Three Scientific Associations (SER-SEC-AEG). Reumatología Clínica (English Edition). 2014; 10: 68-84. doi: 10.1016/j.reumae.2013.10.008.
- Xiao X, Zhang Q, Ouyang Z, Guo X. Comparison of perioperative flurbiprofen axetil or celecoxib administration for pain management after total-knee arthroplasty: A retrospective study. Medicine. 2018; 97.
- Rømsing J, Møiniche S, Ostergaard D, Dahl JB. Local infiltration with NSAIDs for postoperative analgesia: evidence for a peripheral analgesic action. Acta Anaesthesiol Scand. 2000; 44: 672-683. doi:10.1034/j.1399-6576.2000.440607.x.
- Murvai GF, Hozan CT, Magheru C, Szilagyi G, Bulzan M, Murvai VR, Cavalu S, Ghitea TC. Highlighting the Advantages and Benefits of Non-NSAID Treatment After Total Knee Arthroplasty: A Cross-sectional Study. in vivo. 2023; 37: 2371-2380.
- Berardino K, Carroll AH, Ricotti R, Popovsky D, Civilette MD, Urits I, Viswanath O, Sherman WF, Kaye AD. The ramifications of opioid utilization and outcomes of alternative pain control strategies for total knee arthroplasties. Orthopedic Reviews. 2022; 14.
- Nistor-Cseppento CD, Moga TD, Bungau A, Tit DM, Negrut N, Pasca B, Bochis CF, Ghitea TC, Jurcau A, Purza AL, et al. The Contribution of Diet Therapy and Probiotics in the Treatment of Sarcopenia Induced by Prolonged Immobilization Caused by the COVID-19 Pandemic. Nutrients. 2022; 14: 4701.
- Mochizuki T, Yano K, Ikari K, Hiroshima R, Takaoka H, Kawakami K, Koenuma N, Ishibashi M, Shirahata T, Momohara S. Tramadol hydrochloride/acetaminophen combination versus non-steroidal anti-inflammatory drug for the treatment of perioperative pain after total knee arthroplasty: A prospective, randomized, open-label clinical trial. Journal of Orthopaedic Science. 2016; 21: 625-629. doi: https://doi.org/10.1016/j.jos.2016.07.011.
- Mizner RL, Petterson SC, Stevens JE, Axe MJ, Snyder-Mackler L. Preoperative quadriceps strength predicts functional ability one year after total knee arthroplasty. The Journal of rheumatology. 2005; 32: 1533-1539.
- Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clinical biomechanics. 2008; 23: 320-328.
- Wu Y, Lu X, Ma Y, Zeng Y, Xiong H, Bao X, Shen B. Efficacy and safety of limb position on blood loss and range of motion after total knee arthroplasty without tourniquet: A randomized clinical trial. Int J Surg. 2018; 60: 182-187. doi: 10.1016/j.ijsu.2018.11.008.